The Female Reproductive System
advertisement

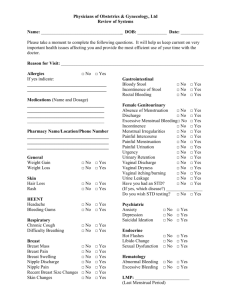
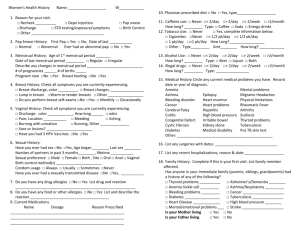
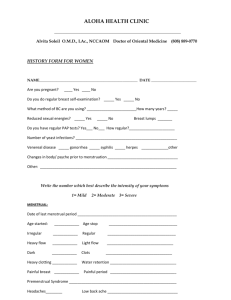
The Female Reproductive System The External Genitalia I. Collectively, the external genitalia of the female are known as the vulva & they include the mons pubis (veneris), labia majora, labia minora, clitoris, vestibule & the urethral opening A. Mons pubis (veneris) or mount of Venus - the rounded, soft area above the pubic bone that becomes covered with hair at puberty B. Labia majora (major lips) – 2 large folds of skin whose main function is to protect the external genitalia C. Labia minora (minor lips) – 2 folds of skin lying inside the labia majora D. Clitoris – most sensitive structure in the female body - contains 2 spongy bodies (corpora cavernosa) that have the capacity to fill with blood during arousal E. Vestibule – when clitoris is erect & labia minora are spread, the urethral & vaginal openings (the vestibule) become visible 1. Urethral opening – urine excreted from it F. Hymen – thin connective tissue containing relatively large number blood vessels 1. Covers vaginal opening in women with an intact hymen; function unknown 2. They vary in shape & size; may surround vaginal opening (annular), bridge it (septate) or form sievelike covering (cribriform) The Internal Genitalia I. Vagina – hollow, tunnellike structure (~4.5 inches [11.4 cm] long); opens outward to the vestibule & at opposite end into the uterus A. It has several reproductive functions: B. When it is empty, the lips & walls of the vagina are in contact 1. During childbirth, it can expand wide enough for baby to pass through C. No muscles surround the vaginal entrance (the introitus) 1. Pubococcygeal & bulbocavernosus muscles support vagina & can be voluntarily contracted to intensify sexual responsiveness (force vaginal walls to close on penis) II. The Grafenberg (G) Spot – stimulation of area along anterior (front) wall of vagina several inches into canal& just under bladder appears to be sexually exciting for many females A. Named after Ernest Grafenberg, who first noticed its erotic potential B. There are glands in this area (Skene's glands) through which a type of ejaculate is expelled in some women when they experience orgasm by G spot stimulation C. Others argue that there is no particular spot in vagina that is more sensitive than others to stimulation D. To stimulate, insert 2 fingers into vagina & press deeply into tissue of vagina anterior wall between posterior side of pubic bone & cervix E. The G spot as the female prostate – front wall of the vagina has prostate-like glandular tissue; substances within gland contain fluids similar to those in male prostate 1. Thus some experts conclude that there is a female prostate (Skene's glands) & a female ejaculate F. The fact that some women expel fluid from vagina during orgasm is established; the prevalence of this phenomenon is unknown III. The uterus – lies at top of vagina; a pear-shaped, hollow organ with muscular walls; it nurtures the developing embryo & fetus A. Normally, it is ~3 inches (8 cm) long, 3 inches wide at the top & 1 inch (2.5 cm) thick 1. It extends into the vagina at its cervix; the opening in the cervix to the uterus is the os B. Uterus consists of 3 layers 1. Perimetrium – outermost layer is very elastic; enables uterus to accommodate a growing embryo during pregnancy 2. Myometrium – middle layer; consists of smooth muscles whose ability to contract helps push the newborn through the cervix & into the vagina (the birth canal) 3. Endometrium – innermost layer; loaded with blood vessels & therefore can provide nourishment needed to sustain developing fetus IV. Fallopian tubes and ovaries – at fundus, uterus opens into 2 fallopian tubes (oviduct); at the other end of each tube is an ovary that produces & stores the ova (eggs) A. When a female is born, each of her ovaries contains ~40,000 – 400,000 eggs B. When egg is released from ovary, it is directed into fallopian tubes (routes to uterus) 1. Newly released ovum is caught by fingerlike end of fallopian tube (fimbria) & guided into cone-shaped open end of tube; fertilization usually takes place there C. Sometimes woman can produce >1 egg per cycle, therefore being prone to multiple births D. Sometimes egg may attach in abdominal cavity or fallopian tube rather than uterus (ectopic pregnancy) V. Breasts are not reproductive organs, but are significant in sexual arousal & response; they serve important reproductive function in providing milk for newborn A. Each breast contains ~15-20 clusters of milk-secreting structures (mammary glands) 1. Each mammary gland cluster has an opening to nipple which is also where milk ducts open 2. Stimulation of newborn sucking on nipple causes pituitary gland to secrete the hormone prolactin, which in turn stimulates the production of breast milk B. Nipples of women (& men) are richly supplied with nerve endings that respond with pleasurable sexual feelings when stimulated C. Breast reconstruction is common 1. In past, liquid silicone was injected to enlarge breasts, but ~60% of women experienced problems like infection, deformity, or exceptional hardness of breast The Hormones I. Stages in sexual response after sighting of attractive person A. If sighting is interesting enough, first sexual response stage occurs – elevated heart rate, vaginal lubrication, erection of penis or clitoris – how does sight cause physical changes? 1. Starts with hypothalamus (structure in brain that, either through direct nerve pathways or through chemical releasing factors, can instruct various body parts to function B. These powerful acting hormones are chemicals that influence organs & tissues; they are produced by endocrine glands (glands that secrete their hormones into bloodstream) II. Pituitary – pea-shaped gland located at base of brain; master gland to others in system A. Stimulates other glands to release hormones; front part of pituitary secretes 3 sexual hormones (gonadotropins); stimulate gonads (testes, ovaries; also endocrine glands) 1. Follicle-stimulating hormone (FSH) 2. Luteinizing hormone (LH); interstitial-cell-stimulating hormone (ICSH) in males 3. Prolactin – B. Once stimulated by gonadotropic hormones, gonads produce their own hormones – estrogens, progesterones, androgens 1. In women, estrogens & progesterones regulate menstrual cycle, with estrogens important in producing vaginal lubrication C. Despite the fact that hormones account for & influence sexual differences, males & females produce the same ones (estrogens, progesterones – female; androgens – male) 1. Males & females produce all 3 but they differ in the amounts they produce Menstruation I. Sometime during puberty, a girl reaches menarche; she has her first menstrual cycle A. Cyclically after that point, blood-enriched endometrium is discharged from vagina for several days B. Menarche – why does menstruation begin when it does? 1. It may relate to the increase in body fat at puberty as the result of hormonal secretions – evidence for this comes from long-distance runners 2. Many women who run long distances lose considerable weight & then develop secondary amenorrhea (stoppage in regular menstruation) C. Menstrual physiology – menstruation begins when the pituitary secretes 2 hormones: FSH (stimulates growth or ripening of follicles in ovary) & LH (stimulates ovulation) 1. Once egg is released, the area from which it is released (Graafian follicle) becomes a yellow body (corpus luteum) 2. Graafian follicle secretes estrogen & yellow body secretes progesterone & estrogen II. Phases of menstrual cycle – proliferative phase, secretory phase, menstrual phase; pertains to changes in uterus A. Proliferative phase – FSH production is increased by pituitary, which stimulates follicles in ovaries to mature; follicles then produce estrogen 1. Estrogen causes uterine endometrial lining to thicken & prepare for zygote implantation B. Secretory phase – begins once ovulation occurs & entails continuing secretion of LH, which stimulates development of corpus luteum (CL) 1. CL secretes progesterone, causing further thickening & engorgement of blood of endometrium C. Menstrual phase – uterine endometrial lining is sloughed off as menstrual flow III. Some divide menstrual cycle into 3 different phases – follicular phase, ovulation & luteal phase; this categorization pertains to changes in ovaries A. Follicular phase coincides with menstrual & proliferative phases B. Ovulation is marked by discharge of ovum from Graafian follicle C. Luteal phase is the same as the secretory phase IV. In 28 day cycle, ovulation occurs on day 14 with menstrual flow lasting 4 days – not very common A. Despite differences in lengths of cycle, luteal phases in cycles do not differ very much B. Regardless of length of menstrual cycle, once ovulation occurs, it basically takes 14 days until menstruation begins V. Effects of menstruation on body & mind – it can have physical & emotional effects, although they can vary greatly from woman to woman & cycle to cycle A. Evidence that ~10% of women take time of from work, school or other activities due to menstrual discomfort B. Whatever symptoms a woman experiences may be a function of what she expects to experience; there is evidence for this 1. If researchers studying menstruating women let them know what study is about, women report more of these symptoms than if they do not know what study is about C. Stress research indicates that mind/body connection is real D. Depending on age & whether one has had a child or not cramping associated with menstruation can vary VI. Menstrual problems - dysmenorrhea – painful menstruation; some women experience some pain & discomfort during menstrual cycles; others experience it regularly A. >50% of women have periods so painful that they see a doctor at some point B. Primary dysmenorrhea (pain during menstruation) – cause is not specifically known 1. Many feel the cause is prostaglandins – produced by body tissues & act as hormones; found in unusually high amounts in women with dysmenorrhea 2. They cause uterine muscles to contract; contraction causes pain & cuts off some of blood supply to uterus, which causes more discomfort C. Secondary dysmenorrhea – painful menstruation caused by some other identifiable condition 1. Endometriosis – condition in which endometrial cells attach & develop on some other body tissue than the uterus; it can cause secondary dysmenorrhea 2. Can also be caused by pelvic inflammatory disease, uterine tumors, blockage of the uterine opening (the os) VII. Menstrual problems – amenorrhea; it is the absence of menstrual flow A. If a woman is 18 & has never menstruated, it is called primary amenorrhea; if menstruation ceases after menarche, it is called secondary amenorrhea B. May be caused by pregnancy, ovary malfunction, cysts or tumors, disease, hormonal imbalance, poor nutrition, emotional distress, strenuous exercise (runners, young dancers) VIII. Menstrual problems – premenstrual syndrome (PMS); it is mood changes & other physical & emotional discomforts just prior to menstrual periods A. >150 complaints associated with it like: 1. Depression, tension, anxiety, mood swings, irritability/anger, difficulty concentrating, 2. Lethargy, weight gain, fluid retention, bloating, breast soreness, join or muscle pain, nausea, vomiting, headaches B. At some time during reproductive years, 40% of women experience PMS C. Described by Katharina Dalton; some were happy to find out that others suffered from it; others did not like implication that cycle was illness with accompanying discomforts 1. Only 10% have symptoms severe enough to interfere with normal functioning D. Theories about the causes of PMS & corresponding treatments 1. Prostaglandins – released into bloodstream as uterine lining begins to be shed; as they build up, they cause uterine walls to become tense & to contract —> cramping 2. Progesterone – builds up during menstrual cycle —> PMS symptoms; antiprogesterone meds recommended to alter menstrual cycle (speeding or delaying bleeding onset 3. Natural opiates – women experience drop in neurotransmitter -endorphin, which is manufactured in brain the week before menstrual flow 4. State of mind symptoms of PMS are result of brain activity (mind); moods, thoughts, perceptions, ideas, self-confidence, self-image choreographed by brain premenstrually E. Other treatments 1. Birth control pills to stop ovulation 2. Medications like injectable medroxyprogesterone acetate (Depo-Provera) to stop ovulation & menstruation temporarily in severe cases 3. Antidepressants in lower doses than usually prescribed for depression like: F. Also the following recommendations are made: IX. Menstrual problems – endometriosis; tissue resembling inner uterine lining (endometrium) is found outside uterus; not an uncommon occurrence; causes not known A. Found most often on lining of pelvic cavity, ovaries, on rectum, colon, in uterus & bladder; sometimes also found on small intestine, liver, spleen, & lymph nodes B. Theories about the cause of endometriosis 1. Pieces of endometrium somehow get into fallopian tubules & are transported into pelvic cavity (retrograde menstruation) 2. In early fetal development, only a few cells are present & they eventually differentiate into different tissue 3. Endometrial cells are transported through blood stream or through lymphatic system to sites elsewhere in body 4. Breakdown in function of immune system resulting in inability to destroy endometrium cells that manage to leave uterus —> endometriosis C. Sufferers usually experience a great deal of pelvic pain, just before or during menstrual bleeding & usually abates after bleeding cessation 1. Pain may also be felt in lower back or lower abdomen & may be associated with urination; there may be fatigue &/or bloated feelings D. Treatments depend on severity of symptoms & location of tissue 1. Laparascopic surgery – 2 small incisions made in abdomen; insert viewing instruments to perform surgical cut; determine if tissue is endometrium-derived & its location 2. Tissue can then be removed surgically before procedure is completed; sometimes tissue has spread so far that abdomen must be opened to remove it (laparotomy) 3. Some medications result in lower levels of estrogen than normal & alleviate much of pain associated with endometriosis X. The menstrual cycle & sex – is there a relationship between the menstrual cycle & sexual interest? —> results are contradictory A. Some say women are more interested in sex before menstruation; others say they are more interested during menstruation; others say the middle of the menstrual cycle B. Time of sexual arousal probably varies from woman to woman & depends on menstrual physiology, the lover, the setting & numerous psychosocial factors like: C. No medical reasons for refraining from sex during menstruation, but many do so; over half of men & women in survey believe couples should refrain during menstruation 1. Some do so because of religious taboos – Orthodox Jews menstruating women are unclean & should sleep in separate bed; cleanse themselves in ritual bath (mikvah) Pregnancy & Lactation I. Hormones are important in pregnancy & lactation; missed period usually means a woman's hormonal level has changed due to pregnancy, but hormones are active before period missed A. After conception, fertilized egg moves down fallopian tube to become implanted in endometrium, which has been enriched by earlier estrogen secretions 1. Pituitary waits for diminished estrogen as signal to continue cycle (by FSH release) B. 1 – 3 days after birth, mother's breasts begin producing milk to prepare for breastfeeding 1. Milk production results from effect of sucking infant on nipple, which stimulates pituitary to secrete prolactin (a hormone) & another hormone called oxytocin II. Advantages of breastfeeding – pediatricians recommend breastfeeding for first year of lives A. Nursing provides nutrients necessary for newborn & passes antibodies that provide protection against a variety of illnesses B. Breastfeeding helps uterus return to previous size & location & helps to stop internal bleeding C. Breastfeeding has some effectiveness as a contraceptive since high levels of prolactin inhibit ovulation; however, it should not be relied upon since it is not as effective as other methods D. Nursing provides a saving in costs & convenience E. Also provides psychological advantages – may provide more closeness to baby (bonding or attachment) III. Disadvantages of breastfeeding A. If mother has ingested certain drugs or medications, they may be passed to infant through breast milk & be potentially damaging B. Cow milk ingested by mother contains antibiotics suspected of causing colic in breast-fed babies C. Does increase convenience since bottles do not need to be prepared, but mother's flexibility is limited D. Fathers can participate in bottle-feeding not in breastfeeding so some men prefer bottlefeeding, but many families do mostly breastfeeding with father giving one bottle per day Menopause I. Between 40 & 55, women make progressively less estrogen & progesterone due to effects of aging on ovaries A. Pituitary continues to make FSH & LH, but ovaries cannot respond to them as once could B. Decrease in estrogen & progesterone takes place over ~5- to 10-year period & results in cessation of menstruation II. Symptoms of perimenopause & menopause - ~80% of women report mild or no symptoms[ 20% have symptoms severe enough to seek medical attention A. Headaches, dizziness, palpitations, insomnia, anxiety, weight gain, hot flashes, vaginal dryness B. Hot flashes (hot flushes) – sudden waves of heat felt throughout the body, often accompanied by reddening, sweating & sometimes dizziness 1. Some experience them infrequently; others have them every few hours or so; some never have them C. Vaginal dryness – results from lowered estrogen in vaginal walls; causes shrinking & thinning; vaginal mucosa becomes thinner D. Decalcification of bones also caused by decreased estrogen levels; leads to osteoporosis 1. Osteoporosis occurs when enough calcium is lost in bones to make person susceptible to bone fractures & bending (curved back [dowager's hump] in older woman III. Treatment of menopause A. Estrogen replacement therapy (ERP) – treats menopause as estrogen deficiency; replaces estrogen; controversial since associated with increased breast & endometrial cancer risks 1. Estrogen supplements used a lot until 1970s until endometrial cancer risks recognized 2. Progestin added causing sloughing of endometrial lining & eliminating endometrial cancer; now widely used B. ERT & breast cancer – early on found estrogen without progestin was connected to development of breast cancer 1. More recent results suggest that ERT increases breast cancer risk & the longer she takes it the greater the risk; others conclude that ERT does not affect breast cancer risk C. Current medical opinion weighs in on the side of ERT for most women; its benefits are thought to outweigh the risks D. Other treatments for menopause specific to osteoporosis E. Some physicians prescribe tranquilizers for women having difficulty with the psychological aspects of menopause F. Treatment for vaginal dryness – use of lubricated creams, vegetable oils, water-soluble jellies (K-Y, Lubifax), suppositories (Replens), regular masturbation/sex reduce soreness IV. Benefits & positive aspects of menopause A. Fear of pregnancy removed & lovemaking is often more enjoyable B. Focusing on positive aspects of menopause is likely to minimize undesirable symptoms; focusing on negative aspects probably increases symptoms C. Women turn to support groups or online forums to share strategies for coping with symptoms V. Hormone therapy – also used for things other than menopausal symptoms Sexually-Related Diseases – The Breast I. Self-care & protection – some diseases not transmitted by sex but do affect sex organs A. Advances in chemical & surgical treatments of sex organ diseases have improved survival rates & made restoration of function more attainable than ever B. Maintaining reproductive health means following safer sex practices, paying attention to body (monitor it for certain signs), using specialized health services & seeking info C. Successful treatment of SRDs depends on early diagnosis of potential problems II. Breasts – most common: cancer, cystic mastitis (mammary dysplasia), fibroadenoma, nipple discharge, breast abscess; most occur only in women although men can get breast cancer A. Breast cancer – second leading site of cancer in American women (lung first) & second major cause of cancer death 1. 178,700 new cases diagnosed in 1998; 1600 cases in men 2. In 1980s, ~4% increase per year; now leveled off at ~110 cases per 100,000 people; ~43, 500 women & 400 men died of it in 1998 B. No specific cause known but certain risk factors predispose women to breast cancer 1. Age – as women get older, risk increases 2. Risk higher in women with family history of breast cancer C. Breast self-examination – among most valuable self-care procedures a woman can adopt 1. Checking every menstrual cycle increases chance of early detection 2. Technique is simple & value immeasurable; earlier diagnosis, better survival; early diagnosis means less invasive treatment D. Women should also have clinical breast exam and/or mammogram (breast X-ray that detects lumps usually before palpable) regularly depending on age & medical history 1. Between 20 & 40 every 3 years and annually thereafter E. If breast cancer is suspected, a biopsy is performed 1. In needle biopsy, fine needle is inserted into tumor & fluid & cells are withdrawn F. Patients are grouped into stages; determined by characteristics of tumor & lymph nodes & whether metastasis has occurred; treatment depends upon stage 1. Lumpectomy – tumor & lymph nodes under arm are removed usually followed by radiation therapy 2. Mastectomy – breast & lymph nodes under arm removed; chemotherapy (treatment with drugs) radiation therapy and hormone therapy; 3 kinds of mastectomy G. Patients with no lymph node involvement – hormone therapy often used to prevent recurrence (tamoxifen & designer estrogens most often used); administered for 5 years H. Survival rates for early stage breast cancer with modified radical & lumpectomy with radiation are similar I. Women who have had mastectomy suffer feelings of loss, fear of rejection & fear of recurrence due to "importance" of breast in our society III. Cystic mastitis (chronic cystic mastitis, fibrocystic condition, mammary dysplasia [cell change]); the most common breast condition; usually found in women 30 – 50 years old A. Uncommon in postmenopausal women & believed to estrogen activity B. Small & large cysts form in breast tissue; generally filled with fluid & may have to be drained frequently; sometimes they must be removed IV. Fibroadenoma – benign, noncancerous tumor that may develop in white women in early 30s & in black women somewhat earlier; tumor is usually firm, round & somewhat movable V. Nipple discharge – in non-nursing women could most often be due to cystic mastitis, to a small benign tumor (papilloma) in a duct leading to nipple A. Could also be due to an uncommon condition (ectasia) in which breast ducts enlarge & distend allowing fluid to accumulate & escape VI. Breast abscess (infection) – usually seen in nursing women but seen in non-nursing women as well & should be treated by a physician A. Redness, swelling or tender, painful mass is symptomatic of breast infection Sexually-Related Diseases – The Cervix and the Uterus I. Rates of invasive cervical cancer, which involves deep-tissue layers of cervix & sometimes spreads to other organs have decreased steadily over the last several decades A. Decrease from 14.2 per100,000 in 1973 to 7.8 per100,000 in 1994 is attributed to increase in Pap smear screening —> early detection & early treatment B. Exact cause is unknown but several factors can put one at risk C. American Cancer Society recommends annual Pap smear with pelvic exam in sexually active women (are or have been) or who are 18 or older 1. After 3 consecutive normal tests, do it less frequently at woman's/doctor's discretion D. Treatment usually consists of surgery and radiation or both II. 1998 – estimate of 36,100 uterine cancer cases diagnosed (mostly of endometrium); rates of uterine cancer steady since mid-1980s at 21 per 100,000; in 1998, ~6,300 deaths from it A. Mortality rate since 1989 relatively constant at 3 per 100,000 B. Estrogen is major risk factor; risk rises for women who: C. Accommodations that have been made to reduce the risk D. Other risks for uterine cancer – infertility, diabetes, hypertension, obesity; pregnancy & use of oral contraceptives provide protection against uterine cancer E. Pap test does not detect uterine cancer efficiently so ACS recommends that women >40 have a yearly pelvic exam F. Treatment depends on stage – surgical removal of uterus and/or ovaries, radiation therapy, hormonal therapy & chemotherapy III. Ovaries – ovarian cysts (abnormal cavity filled with fluid) & tumors occur at any age A. Most common cysts are functional cysts; they occur on follicle or corpus luteum; usually caused by failure of follicle to rupture & discharge egg B. Dermoid cysts – common inn young women; contain hard, fatty material & sometimes remnants of teeth; considered to be embryonic in nature & are considered benign C. Stein-Leventhal syndrome – ovaries become enlarged & have cysts on them; also may cause infertility & secondary amenorrhea; seen in females 15 – 30 years of age 1. Thought to be of endocrine origin; once diagnosed treated with surgery or medication IV. Ovarian cancer – killed ~14,500 American women (1998); causes more deaths than any other female reproductive system cancers A. 25,400 new cases diagnosed in 1998 (4% of all cancers in women); deadly because its symptoms are silent; they go unnoticed until late in cancer development B. Risk factors for ovarian cancer C. Early detection is once again important; pelvic exams most valuable; Pap tests rarely effective in detecting ovarian cancer D. Treatment can include: E. One-year survival rate from time of diagnosis is 76%; 5 year survival rate is 46% 1. If detection & treatment are early survival goes up to 93% Sexually-Related Diseases – The Vagina I. Normal vaginal secretions are odorless & acidity helps it to cleanse itself A. However, some women choose to cleanse their vaginas by douching – rinsing with water or vinegar-water solution; not recommended & can be harmful if not done correctly B. Damage can occur in 2 main ways 1. Improper insertion of douching material may damage tissue, resulting in increased chance of infection 2. Chemical balance of vagina can be altered, affecting contraceptive function; spermicidal cream or other spermicide may have its effectiveness destroyed II. Smegma (cheeselike substance secreted by glans penis of males may have health implications for women A. Women having sex with man who has not cleaned away smegma could be subjecting herself to vaginal infections; may also contribute to cancer of cervix B. STDs should also be given attention – check vulva looking for unusual discharges, also pay attention to abdominal pain or open sores on genitalia III. Toxic shock syndrome (TSS) – toxins that cause this are produced by Staphylococcus aureus bacteria, which may grow in vagina & be absorbed by body A. Toxins enter bloodstream & cause high fever (>102°C), nausea, vomiting, diarrhea, rapid drop in blood pressure & sometimes aching muscles & peeling skin on palms & feet B. Exact mechanism of transmission unknown 1. Appears to be linked to use of tampons, particularl those made of superabsorbant material C. It is recommended that superabsorbent tampons not be used because they pack vagina tightly, prevent air circulation & allow bacteria to proliferate D. TSS has relatively high fatality rate (5%) originally reported in 3 out of 100,000 women IV. Any unusual signs or symptoms should be reported to a specialist in reproductive health – gynecologist/gynecological nurse practitioner; women should have regular exam every year A. Inspection of external genitals for irritations, discolorations, unusual discharges or other abnormalities B. Internal check for cystoceles (bulges of bladder into vagina) & rectoceles (bulges of rectum into vagina) C. Inspect vagina & cervix by means of speculum (plastic or metal instrument inserted into vagina to hold vaginal walls apart during exam – looks for lesions, inflammation, Pap test D. Bimanual exam – slide index & middle fingers of one hand into vagina & press down on abdominal wall from outside E. Examination of breasts for lumps or thickenings F. Exam should not be painful & practitioner should take complete gynecological history, including whether mother used DES during her pregnancy higher vaginal cancer rates