To:
advertisement
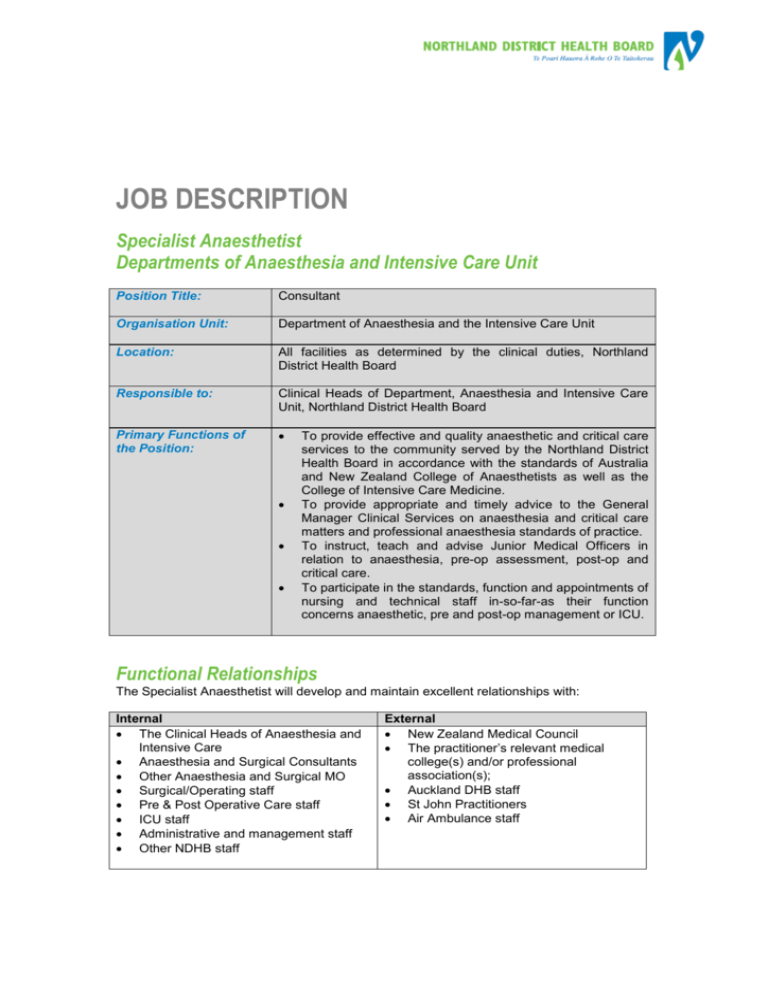
JOB DESCRIPTION Specialist Anaesthetist Departments of Anaesthesia and Intensive Care Unit Position Title: Consultant Organisation Unit: Department of Anaesthesia and the Intensive Care Unit Location: All facilities as determined by the clinical duties, Northland District Health Board Responsible to: Clinical Heads of Department, Anaesthesia and Intensive Care Unit, Northland District Health Board Primary Functions of the Position: To provide effective and quality anaesthetic and critical care services to the community served by the Northland District Health Board in accordance with the standards of Australia and New Zealand College of Anaesthetists as well as the College of Intensive Care Medicine. To provide appropriate and timely advice to the General Manager Clinical Services on anaesthesia and critical care matters and professional anaesthesia standards of practice. To instruct, teach and advise Junior Medical Officers in relation to anaesthesia, pre-op assessment, post-op and critical care. To participate in the standards, function and appointments of nursing and technical staff in-so-far-as their function concerns anaesthetic, pre and post-op management or ICU. Functional Relationships The Specialist Anaesthetist will develop and maintain excellent relationships with: Internal The Clinical Heads of Anaesthesia and Intensive Care Anaesthesia and Surgical Consultants Other Anaesthesia and Surgical MO Surgical/Operating staff Pre & Post Operative Care staff ICU staff Administrative and management staff Other NDHB staff External New Zealand Medical Council The practitioner’s relevant medical college(s) and/or professional association(s); Auckland DHB staff St John Practitioners Air Ambulance staff Key Responsibilities and Expected Outcomes Northland District Health Board has established a set of values by which the organisation will respond, in part, to achieving its goals and objectives through their workforce. The following Values and supporting statements are expected behaviours of each individual employed with NDHB: Values Supporting Statement People First Tangata I te tuatahi Respect Whakaute (tuku mana) Caring Manaaki Communication Whakawhitiwhiti korero Excellence Taumata teitei (hirangi) People are central to all we do We treat others as we would like to be treated We nurture those around us, and treat all with dignity and compassion We communicate safely, openly and with respect to promote clear understanding Our attitude of excellence inspires success, competence, confidence and innovation The position of Specialist Anaesthetist encompasses the following major functions or key result areas: Clinical Responsibilities Records and Documentation Patient Information and Informed Consent Staff and Patient Relations Consultation Advice Health Promotion and Disease Prevention Quality Assurance Team Effectiveness Service Planning Budgeting and Management Resource Utilisation Teaching Responsibilities Continuing Medical Education Treaty of Waitangi Health and Safety The outcome requirements of the above key responsibility areas are outlined below: Key Responsibility Area Clinical Responsibilities Expected Outcomes Professional responsibility to patients is paramount. The Anaesthetist will share responsibility with his colleagues to ensure an efficient and effective quality anaesthetic and critical care services are provided. The Anaesthetist will perform anaesthetic duties which lie within his training and ability and will manage patients according to contemporary convention and college guidelines. Duties performed will be realistically possible within agreed contracted hours. Routine Hours are 8 am to 6pm Monday to Friday Clinical Duties of the Anaesthetist may include: Provision of anaesthesia for elective surgery sessions. Provision of anaesthesia for acute (non booked) surgery. Scheduled anaesthetic duties in other locations, eg Radiology, CT, Psychiatric Unit, Delivery Suite. Pre-operative assessment clinics. ICU Cover - Clinical management and primary responsibility for Key Responsibility Area Records and Documentation Patient Information and Informed Consent Staff and Patient Relations Consultation Advice Health Promotion and Disease Prevention Quality Assurance Team Effectiveness Service Planning, Budgeting and Management Expected Outcomes patients in the Intensive Care Unit. Participation and coordination of air ambulance patient retrieval service. Acute Pain Service duties. Comprehensive and accurate medical records with respect to anaesthesia/ICU will be maintained for all patients with whom the Anaesthetist is involved. Patients will be given a clear explanation of all procedures and treatments where possible. Informed consent will be obtained from all patients in accordance with Northland District Health Board policy. The Anaesthetist will work together with other Anaesthetists to ensure provision of a quality service. The Anaesthetist will liaise with other clinical specialists as necessary to maintain optimal patient care. Annual leave will be coordinated within the Anaesthetic Department in order to maintain service continuity. The Anaesthetist will see and advise on inpatients referred by hospital specialist colleagues for an Anaesthetic opinion. The Anaesthetist shall make provision to be contacted by the junior medical staff regarding elective cases and non-list cases between 8am and 6pm weekdays. When on call for Anaesthetics, the Anaesthetist will liaise closely with theatre staff to allow effective planning of theatre usage. When on call for ICU the Anaesthetist will liaise with the ICU Registrars and Charge Nurse to ensure continuity of service and appropriate use of resources. When on call for ICU the Anaesthetist will also need to liaise with Auckland, Whangarei and peripheral hospital colleagues to ensure an efficient air retrieval service. The Anaesthetist shall take an active role in health promotion as appropriate and as requested by the Manager, Surgical Services, within contracted hours. The Anaesthetist will maintain the high standards of patient care as set out by the College of Anaesthetists. The Anaesthetist will participate in the Quality Assurance programme for Northland Health. This will incorporate review of patient care, review of complications and review of any deaths that occur in the service. The Anaesthetist shall ensure he fulfils the current Departmental audit requirements. The Anaesthetist will contribute to the ongoing evaluation of the surgical service as a whole. The Anaesthetist will attend as appropriate to any enquiries or complaints from patients, relatives, staff or management. The Anaesthetist will contribute to the formal review of anaesthetic staff within the Department annually. The Anaesthetist will work together with other Anaesthetists to ensure provision of a quality service. The Anaesthetist will liaise with other clinical specialists as necessary to maintain optimal patient care. Annual leave will be coordinated within the Department in order to maintain service continuity. Overall forward planning and budgeting for the Surgical Service will be conducted as a combined operation with Anaesthetists, other surgical staff and the Manager, Surgical Key Responsibility Area Resource Utilisation Teaching Responsibilities Continuing Medical Education Treaty of Waitangi Health & Safety Expected Outcomes Services. Surgical service business plans, service budgets and capital budgets and service priorities shall be prepared with the involvement of the Anaesthetic Department. Budget estimates will reflect the availability of resources. Each Anaesthetist shall contribute in part to administration of the Department and work together to achieve an effective surgical service As a user of finite resources each Anaesthetist is responsible for the effective and efficient use of such resources and the utilisation of such departments within the hospital which may aid in this matter. Expenditure on Theatre/ICU supplies and pharmaceuticals will be as cost effective as possible. The Anaesthetist will, with his anaesthetic colleagues, Theatre Manager, ICU Charge Nurse and other senior health professionals, work with the nursing personnel of the operating theatre and ICU and to ensure that resources are used efficiently. The Anaesthetist will participate in the teaching of Resident Medical Officers, Technicians and nursing staff. The Anaesthetist will keep up to date with trends and developments and utilisation of technology in anaesthesia and intensive care on an ongoing basis. This will be done through regular discussion with colleagues, reading literature and participating in conferences and meetings. Formal approval of an ethics committee via the Chief Medical Advisor will be sought for any research undertaken or involvement in therapeutic trials which will be conducted in assistance with other ethics committees’ protocols. Contribute to the promotion of the principles of Treaty of Waitangi and the involvement of Maori within the decision making process for their health and independence, within District Health Board management processes and procedures Include the principles of the Treaty of Waitangi within all aspects of the role and its outcomes Ensure that consultation and engagement processes include appropriate mechanisms to meet the need of Maori in a culturally appropriate and safe manner Attend the Northland District Health Board Treaty of Waitangi Training Observe and promote safe work practices, rules and instructions relating to work, and be pro-active in hazard management Willingly co-operate in the achievement of all health and safety goals and initiatives by: Practicing and observing safe work methods; The use of safety equipment; Reporting unsafe conditions or equipment; and Reporting and documenting all accidents or incidents Variation of Duties Duties and responsibilities described above should not be construed as a complete and exhaustive list as it is not the intention to limit in any way the scope or functions of the position. Duties and responsibilities may be amended from time to time, in consultation with the employee, to meet any changing conditions and service requirements. The Northland District Health Board will ensure Adequate dedicated support services (e.g. secretarial) provided to enable the Anaesthetist to carry out the duties described. Provision of adequate equipment, services and technical assistance to the standard recommended by the College of Anaesthetists as a minimum. Person Specification Education and Qualifications Desirable Essential Qualified Medical Practitioner Qualified Medical Practitioner Must be eligible for vocational registration Must be eligible for vocational registration with the Medical Council of New Zealand with the Medical Council of New Zealand Experience Desirable Previous experience as a Consultant Possession of FANZCA Awareness and Understanding of Desirable Privacy Act (1993) and Health New Zealand Council of Healthcare Information Privacy Code (1994) Standards Health and Safety in Employment Act The Treaty of Waitangi and its application (1992) to the health setting Health and Disability Commissioner (Code of Health and Disability Services Consumers’ Rights) Regulations (1996) Skills & Personal Attributes Skills Computer skills – proficient in Excel and Initiative Word Numeracy skills Excellent communication skills Knowledge of Patient Management System Demonstrated accurate documentation skills Excellent clinical skills in anaesthesia Ability to work under pressure Forward planning Confidentiality Anticipate and prevent clinical problems Organisational skills Efficacy and efficiency in clinical Demonstrated commitment to ongoing procedures education Personal Attributes Forward thinking Communication at all levels, excellent communication and interpersonal skills Professional and Clinical credibility Proven commitment to provision of quality care Function as a professional leader Ability to function as a multidisciplinary team member Commitment to own professional development Position Outline Section 1: The post is full time with the total hours to be outlined in Schedule I, as per job sizing. A separate consultant on call roster is provided to anaesthesia and intensive care. A total of six consultants provide an after hours call to the ICU with a minimum call frequency of a 1:6 roster averaged over the year. These numbers are subject to change and job size will be adjusted as necessary. Registrar support is provided at all hours. Terms and Conditions of the senior medical staff national MECA apply. This is an enhanced contract above those terms. The full time Anaesthetist/Intensivist will undertake eight rostered sessions comprising a mix of 7 Clinical rostered sessions and an additional rostered non clinical session Section 2: CLINICAL DUTIES Rostered session means any rostered period (five hours duration) performing clinical work or being available to perform such work. This includes pre-operative visiting. Rostered sessions may include: Elective theatre sessions Day time acute anaesthesia call Scheduled anaesthetic duties in other departments, e.g. imaging Pre-assessment clinics Pain service duties Intensive Care Retrieval service A morning session is from 0800 – 1300 hours. An afternoon session is from 1300 – 1800 hours. Section3: NON CLINICAL DUTIES Rostered Administration Teaching Audit Quality Assurance Research Unrostered The following activities are not specifically rostered to scheduled times, but will usually take place within the context of other scheduled activities. Remuneration for these duties and activities is deemed to be included in the non rostered payment of 5 hours per week. regular participation in continuing medical education activities on a week-by-week basis, by: - attendance at weekly clinical meetings - personal literature review – adherence to college guidelines of 40 hours Journal reviews per annum is required either personally or by participation in journal review meetings (attendance of at least 50% of planned meetings is therefore encouraged). - Participation in national and local organisations dedicated to education and maintenance of standards within. Administrative tasks not directly associated with clinics, ward rounds, theatre sessions. Preparation of materials for and provision of formal teaching to junior medical staff, nursing staff, and other clinical support staff. Case preparation and research (planning for major cases). Business meetings (at least monthly) Note that the following activities are also required, and are specifically covered by other remuneration and leave provisions: Attendance at New Zealand / Australian CME meetings at least once per annum, and at regional / world CME meetings at least once every three years. (Note the provision of CME leave and financial support for CME activities). Section 4: Weekly timetable is compiled by department roster maker. The usual arrangement is to provide 8 sessions on four days with a fifth day unallocated. Section 5: The medical practitioner is required to undertake their clinical responsibilities and to conduct themselves in all matters relating to their employment, in accordance with best practice and relevant ethical and professional standards and guidelines, as determined from time to time by: the New Zealand Medical Association; the practitioner’s relevant medical college(s) and/or professional association(s); the New Zealand Medical Council; the Health & Disability Commissioner; and the employer’s policies and procedures except to the extent that they may be inconsistent with any other provision of the Collective Agreement Section 6: No clinical leadership management role with this post. Section 7: An annual professional review will occur. This will include a review of job description. The Clinical Head of Department will perform the annual review Specific Objectives will be agreed annually and form part of the performance review. Section 8: Provisions for all leave are outlined in the Collective Agreement for Senior Medical Staff. This provides for six weeks annual leave and twelve days CME with expenses. At least 4 weeks notice of leave is required. Leave does not exist until approved by the Clinical Head of Department. Section 9: The remuneration schedule, to be outlined in Schedule II, will be determined by years of experience after review of Curriculum Vitae. A full time enhancement for flexibility of rostering is added to Collective Employment terms. Authorised by: Date: Acceptance Acceptance of the position implies acceptance of this position description. Position Title: Signature of employee: Date: