CONSENT AUDIT
advertisement

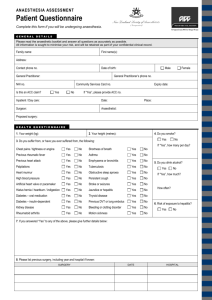
Consent and documentation of risks for anaesthesia audit. Consent for anaesthesia is a hot topic. Guidelines from the AAGBI published in 2006 exist, and salient points are as follows;1 "5.3.8 Information should be provided about: • generally what may be expected as part of the proposed anaesthetic technique. For example, fasting, the administration and effects of premedication, transfer from the ward to the anaesthetic room, cannula insertion, non- invasive monitoring, induction of general and/or local anaesthetic, monitoring throughout surgery by the anaesthetist, transfer to a recovery area, and return to the ward. Intra-operative and postoperative analgesia, fluids and antiemetic therapy should also be described; • postoperative recovery in a critical care environment (and what this might entail), where appropriate; • alternative anaesthetic techniques, where appropriate. Patients do not have to agree to the anaesthetist's preferred anaesthetic technique; • commonly occurring, 'expected' side-effects, such as nausea and vomiting, numbness after local anaesthetic techniques, suxamethonium pains and post dural puncture headache; • rare but serious complications such as awareness (with and without pain), nerve injury (for all forms of anaesthesia), disability (stroke, deafness and blindness) should be provided in written information, as should the very small risk of death. It is good practice to include an estimate of the incidence of the risk [22]. Anaesthetists must be prepared to discuss these risks at the pre-operative visit if the patient asks about them; • specific risks or complications that may be of increased significance to the patient, for example, the risk of vocal cord damage if the patient is a professional singer; • the increased risk from anaesthesia and surgery in relation to the patient’s medical history, nature of the surgery and urgency of the procedure. If possible, an estimate of the additional risk should be provided; • the risks and benefits of local and regional anaesthesia in comparison to other analgesic techniques; • the risk of intra-operative pain, and the need to convert to general anaesthesia, should a proposed local or regional technique be inadequate or ineffective. The risks and benefits of adjunctive sedation or general anaesthesia should be discussed; • the benefits and risks of associated procedures such as central venous catheterisation, where appropriate; • techniques of a sensitive nature, such as the insertion of an analgesic suppository." Current advice does not deem formal written and signed consent necessary for anaesthesia; however documentation of discussions of risk for proposed anaesthesia and anaesthesia techniques should be considered best practice in all circumstances. In a large Australian study2 of 850 cases risk discussion was found to be the least likely preoperative details to be adequately documented. The anaesthetist possesses skills necessary to assess and estimate risk and guide patients in choosing the safest and most efficacious techniques for them. Indeed it is among the 1 http://www.aagbi.org/sites/default/files/consent06.pdf Perioperative anesthetic documentation: Adherence to current Australian guidelines Elhalawani Islam, Jenkins Simon, Newman Nicole Year : 2013 | Volume: 29 | Issue Number: 2 | Page: 211-215 2 most important facet of the anaesthetist’s role to provide patients with relevant and accurate information to allow decision making about anaesthetic technique decisions. This audit follows recommendation from the 3rd edition of the RCOA audit recipe book3 and can be mapped to the following curriculum areas; CPD matrix code: 1F01 Basic curriculum competences: OA_BK_01, OA_BK_11, OA_BK_12, OA_135_06 Intermediate curriculum competence: GU_135_06 It seeks to understand the current practice of documentation of risk across the regions hospitals as the first phase in a three step process to clarify the broader questions raised surrounding consent for anaesthesia. Phase ONE Data collection to be performed from anaesthetic records prospectively across the region over a one week period using the attached data collection proforma, which should hopefully yield a sufficient number to provide a cohesive snapshot. We should attempt to collect data from every anaesthetic performed in patients over the age of 18 from all areas within the collection time. Obtaining a % of patients with whom discussion of risk and benefits of a particular technique is documented along with simple demographic data ( ASA and Urgency of surgery) Data to be collected includes demographic detail and detail on documentation of risk for GA, Regional technique and/or Neuraxial blockade. Proposed audit goals. Common risks in anaesthesia should be discussed and documented in 100% of elective cases Common and rare but significant risks should be discussed and documented in 100% of cases undergoing Neuraxial blockade Common and rare but significant risks should be discussed and documented in 100% of cases undergoing a regional anaesthetic technique Common and rare but significant risk should be discussed and documented in 100% of emergency cases Phase TWO A region wide survey of anaesthetists to stratify the importance attributed to the individual facets of risk. Phase THREE Patient survey of attitudes to which risks patients feel are important to them. 3 https://www.rcoa.ac.uk/system/files/CSQ-ARB-2012_1.pdf DATA COLLECTION TOOL Please ring or tick appropriate answers PRIORITY ELECTIVE DAY CASE EMERGENCY CONSULTANT SASG ST3-7 CT1-2 1 2 3 4 5 NUHNHST RDHNHST SFNHSFT CRNHST ULHNHST DEATH DIFFICULT INTUBATION/ FAILED INTUBATION ASPIRATION DURING ANAESTHESIA POSTOPERATIVE COGNITIVE DECLINE POSTOPERATIVE DELERIUM DROWSINESS DIZZINESS HEADACHE CVA PAIN PONV SORE THROAT DENTAL DAMAGE AWARENESS PERIPHERAL NERVE INJURY ANAESTHETIST ASA HOSPITAL TRUST GENERAL ANAESTHESIA OTHER (Please write) NEURAXIAL BLOCKADE SPINAL EPIDURAL PARAPLEGIA PERMANENT NERVE DAMAGE HAEMATOMA/ BLEEDING ABCESS/ INFECTION TRANSIENT NERVE DAMAGE DEATH FAILURE BACKACHE URINARY RETENTION PAIN UNILATERAL BLOCKADE POST DURAL PUNCTURE HEADACHE PATCHY BLOCKADE CONVERSION TO GA OTHER (Please write) PERIPHERAL NERVE BLOCKADE PERMENANT NERVE DAMAGE TRANSIENT NERVE DAMAGE FAILURE INFECTION PAIN PNEUMOTHO RAX SYSTEMIC LA TOXICITY DEATH OTHER (Please write) BLEEDING