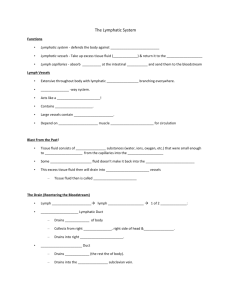
THE LYMPHATIC SYSTEM AND IMMUNITY
advertisement

THE LYMPHATIC SYSTEM AND IMMUNITY
Of what does the lymphatic system consist?
The lymphatic system consists of the fluid lymph flowing within lymphatic
vessels. It also consists of lymphatic tissue composed of aggregates of
lymphocytes and macrophages scattered throughout the body or forming dense
lymphatic nodules such as the tonsils, appendix, and peyer’s patches. The
lymphatic system also consists of lymphatic organs, composed of lymphatic
tissue and a connective tissue capsule. Examples include red bone marrow (
site of lymphocyte production) lymph nodes, thymus, and spleen.
What is Starling’s law of the capillaries?
According to Starling’s law of the capillaries, only 85% of the fluid that leaves
blood (by filtration) to enter the tissue spaces is reabsorbed. The other 15%
bathes the cells as interstitial fluid and is then moved into the lymphatic system
for eventual return to the blood.
What is lymph?
Once in the lymphatic system, the interstitial fluid is called lymph (“clear water”).
Interstitial fluid and lymph are essentially identical fluids.
What is lymphatic tissue?
Lymphatic tissue is a specialized form of reticular connective tissue that contains
large amounts of lymphocytes and macrophages.
List, and then briefly describe, the three essential functions of the lymphatic system.
draining the interstitial fluid -- Excessive interstitial fluid and escaped plasma
proteins are drained back to the blood so that they do not accumulate in
the tissue spaces.
transporting dietary lipids -- Lipids and lipid-soluble vitamins absorbed from the
diet are carried to the blood via the lymphatic system rather than by the
venous drainage of the small intestine.
protection against invaders -- Lymphatic tissue, using lymphocytes and
macrophages, provide immune responses. These are highly targeted to
particular invaders or abnormal cells.
A.
LYMPHATIC VESSELS AND LYMPH CIRCULATION
1.
LYMPHATIC CAPILLARIES
How do lymphatic vessels begin?
Lymphatic vessels begin as close-ended vessels called lymphatic
capillaries. They converge to form larger tubes called, lymphatic
249
vessels or simply lymphatics. They resemble veins in structure, but
are thinner and have more valves. At intervals along the lymphatics, lymph flows through lymphatic tissue structures known as
lymph nodes.
Where are lymphatic capillaries found in the body?
Lymphatic capillaries are found throughout the body, except for the
following areas: all avascular tissues (cartilage, cornea, lens, and
epidermis), the central nervous system, the spleen, and bone
marrow.
Describe the structure and function of the lymphatic capillary.
Lymphatic capillaries are similar to blood capillaries in structure, but
are unique in that they allow interstitial fluid to pass into them, but
not out. Instead of intercellular clefts separating adjacent endothelial cells, lymphatic capillary endothelium overlaps like shingles,
forming a type of one-way valve that allows fluid to move into the
capillary only. When pressure is greater inside the lymphatic
capillary than in the interstitial space, the overlapping cells are
pressed together, preventing the outflow of fluid.
2.
FORMATION AND FLOW OF LYMPH
Describe the components and volume of lymph and how flow of lymph
through its vessels is maintained even though there is no “heart” in the
system.
Most components of blood plasma freely move through the blood
capillary walls to form interstitial fluid; however, more fluid is filtered
than reabsorbed back into the blood capillary.
This excess fluid, about 3 liters/day, drains into lymphatic capillaries
and become lymph. Ultimately, this lymph is delivered back to the
blood via the lymphatic ducts.
In addition, plasma proteins that may have escaped from the blood
are also moved into the lymph and are returned to he blood. This is
important for maintaining blood colloid osmotic pressure.
The flow of lymph from the tissue spaces back to the blood, like
venous return, is maintained by the “milking” action of skeletal
muscles, numerous one-way valves located in lymphatic vessels,
and the respiratory pump.
250
3.
LYMPH TRUNKS AND DUCTS
What are lymph trunks?
Lymph passes from lymphatic capillaries to lymphatic vessels and
then through lymph nodes. When lymphatic vessels leave the
terminal-most group of lymph nodes for an area, they unite to form
large lymph trunks.
Describe the following:
lumbar trunks -- Right and left lumbar trunks carry lymph to the
lower extremities, walls and viscera of the pelvis, kidneys,
adrenal glands, and abdominal wall.
intestinal trunk -- The intestinal trunk carries lymph from the
stomach, intestines, pancreas, and liver.
bronchomediastinal trunks -- Right and left bronchomediastinal
trunks carry lymph from the lungs, heart, anterior thoracic
wall, and diaphragm.
subclavian trunks -- Right and left subclavian trunks carry lymph
from the upper extremities.
jugular trunks -- Right and left jugular trunks carry lymph from the
head and neck.
lymphatic ducts -- These trunks eventually fuse to form the origins
of the two main channels that empty into the venous blood:
the left lymphatic (thoracic) duct and the right lymphatic duct.
4.
5.
THORACIC (LEFT LYMPHATIC) DUCT
RIGHT LYMPHATIC DUCT
Describe the thoracic duct (left lymphatic duct) and the right lymphatic
duct.
The thoracic duct (left lymph duct) is 15-18 inches long, beginning
as a dilation called the cisterna chyli at vertebral level L2.
It is the main collection duct of the lymphatic system, receiving
lymph from the left side of the head, neck, and thorax, the left upper
extremity, and the entire body below the diaphragm.
The intestinal trunk and the two lumbar trunks join to form the
cisterna chyli. The thoracic duct then ascends along the anterior
vertebral surface, posterior to the aorta and inferior vena cava.
251
Near its termination, the thoracic duct receives the left
bronchomediastinal, left subclavian, and left jugular trunks.
The thoracic duct terminates by joining the venous system where
the left subclavian vein and the left internal jugular vein merge to
form the left brachiocephalic vein.
The right lymphatic duct is a very short (1/2 inch) and is formed by
the union of the right jugular, subclavian, and bronchomediastinal
trunks.
It terminates by joining the venous system where the right
subclavian vein and right internal jugular vein merge to form the
right brachiocephalic vein.
B.
LYMPHATIC TISSUE
Lymphatic (lymphoid) tissue occurs in the body in many ways. List, and then
briefly describe, these tissues.
diffuse lymphatic tissue -- Individual lymphocytes are dispersed in the
mucosa of the GI, respiratory, and genitourinary tracts.
lymphatic nodules -- Lymphatic nodules are oval shaped concentrations of
lymphocytes and macrophages. They are not encapsulated
(having a capsule would make them organs), but rather found as
solitary discrete structures (tonsils, Peyer’s patches, in the
appendix).
primary lymphatic organs -- Bone marrow and the thymus gland are the
sites of lymphocyte production and therefore are the primary
lymphatic organs.
secondary lymphatic organs -- Lymph nodes and the spleen are
considered secondary lymphatic organs because lymphocytes
migrate to them and reside there. In addition, these structures
contain reticular tissue.
1.
LYMPH NODES
Describe lymph nodes as follows:
gross anatomy -- Lymph nodes are bean- or oval-shaped structures ranging in size from 1-25 mm in diameter. They are
located in specific groups along the lengths of lymphatic
vessels prior to the formation of lymph trunks. Each group of
252
nodes receives lymph from a particular drainage area of the
body.
capsule -- Each lymph node is covered by a capsule of dense
connective tissue that extends into the node as structures
called trabeculae (singular = trabeculum). Directly beneath
the capsule is the subcapsular or cortical sinus, a space that
receives lymph from afferent lymphatic vessels.
stroma -- Internal to the capsule is a supporting network of reticular
fibers and fibroblasts that together form the stroma or
framework of the lymph node. It is within this framework that
the parenchymal (the essential and distinctive tissue of an
organ as distinguished from its supporting framework) or
functional cells (lymphocytes and macrophages) of the
lymph nodes reside.
cortex -- Lymph nodes are specialized into two areas: cortex and
medulla. The outer cortex contains densely packed
lymphocytes arranged into masses called lymphatic nodules.
The outer rim of a nodule consists of T cell lymphocytes and
macrophages. When an immune response is occurring, the
nodule has a lighter central region called a germinal center
where B cell lymphocytes are proliferating into cells that
secrete antibodies (plasma cells).
medulla -- The inner region of a lymph node, the medulla, is
arranged into strands of packed lymphocytes called
medullary cords.
Describe the flow of lymph into, through, and out of a lymph node.
Lymph flows into a lymph node in one direction via afferent
lymphatics that penetrate the convex outer surface of the capsule
at several points.
Lymph dumped into the subcapsular space percolates through the
node where it is monitored by the lymphocytes and macrophages
for foreign or abnormal cells and antigens as they are trapped by
the reticular fibers.
On the concave border of the lymph node at an indented area
known as the hilus, where one or two efferent lymphatics collect the
lymph from the nodes and carry it away.
Efferent lymphatics may pass to another lymph node (in which case
they become known as afferent lymphatics again) or they may fuse
with others to form lymph trunks.
253
Along with the lymph flowing from a lymph node, new lymphocytes
and antibodies that were formed in the nodule during an immune
response are carried our and thus ultimately back to the general
blood circulation.
Describe the lymphatic drainage of each of the following body regions, the
lymph nodes involved and, and the trunks that ultimately receive the
lymph.
head and neck -- All lymph from the head and neck region moves
to a chain of superficial cervical lymph nodes found in the
dermis of the neck.
After these nodes, lymph is passed to deep cervical lymph
nodes located along the carotid sheath just lateral to the
trachea.
From this terminal group lymph flows into the right or left
jugular lymph trunks.
lower extremity/ lumbar region -- Lymph from the leg flows first to
the popliteal lymph nodes located in the popliteal fossa of
the posterior knee.
All lymph from the lower extremity and lumbar region moves
to the inguinal lymph nodes located along the inguinal
ligament where the lower extremity joins the trunk.
The efferent lymphatics from the distal-most nodes unite to
form the right or left lumbar lymph trunks.\
viscera -- There are thousands of lymph nodes associated with the
viscera of the body.
These nodes are usually located where the blood supply
enters the organ and along the length of the aorta.
The efferent lymphatics form either the bronchomediastinal,
intestinal, or a portion of the lumbar lymph trunks.
upper extremity/anterior thoracic wall/ breast -- All lymph from the
upper extremity and anterior thoracic wall, including the
breast, moves to the axillary lymph nodes located in the
adipose tissue of the axilla.
There are 20 - 30 axillary nodes arranged into a series of
groups.
254
The efferent lymphatics from the distal-most unite to form the
right or left subclavian lymph trunks.
2.
TONSILS
What are tonsils?
Tonsils are multiple aggregations of large lymphatic nodules
embedded in mucous membrane, forming a ring of lymphoid tissue
around the junction of the oral cavity, nasal cavity, and pharynx.
They are strategically located to protect the body from invasion by
microbes that are ingested or inhaled.
What are their names and where are they located?
There are the paired palatine tonsils located on either side of the
fauces, the paired lingual tonsils at the base of the tongue, and a
single pharyngeal tonsil (adenoid) located in the posterior wall of
the nasopharynx.
3.
SPLEEN
Describe the spleen as follows:
location -- The spleen, the largest mass of lymphoid tissue in the
body, is situated in the posterolateral left hypochondriac
region between the stomach and the diaphragm.
structure -- The spleen is surrounded by a dense connective tissue
capsule with trabeculae. Internally, reticular fibers form the
stroma of the organ. (infrastructure is very much like that of
a lymph node)
parenchyma -- The parenchyma of the spleen consists of two types
of tissue: White pulp is lymphocytes arranged around
arteries passing through the organ. Red pulp consists of
venous sinuses and cords of lymphocytes and
macrophages.
function -- The spleen has no role in lymph filtration. Its lymphocytes and macrophages are involved in phagocytosis of
bacteria in blood, as well as old and damaged RBCs. It also
serves as a storage depot for blood that can be used during
times of high demand. With sympathetic stimulation, the
capsule of the spleen contracts and forces its blood back
into the circulation.
255
4.
THYMUS GLAND
Describe the thymus gland as follows:
location -- The thymus gland is located in the superior mediastinum,
posterior to the sternum, anterior to the heart, and between
the lungs.
structure -- It consists of two lobes held together by a connective
tissue capsule. Each lobe has an outer cortex containing
tightly packed lymphocytes, and an inner medulla with
scattered lymphocytes and epithelial cells.
function -- Immature lymphocytes leave the bone marrow and travel
via the blood to the thymus gland, where they take up
residence and receive immunocompetence to become T
cells.
atrophy -- The thymus gland grows to its maximum size in infancy,
when it is most active. After puberty, it begins to involute
with fat and connective tissue, so that by adulthood it is
considered atrophied.
C.
IMMUNITY (SPECIFIC RESISTANCE TO DISEASE)
What is nonspecific resistance to disease?
Nonspecific resistance comprises those defense mechanisms that provide
a general response against a wide variety of pathogens (a specific
causative agent {as bacterium or virus} of a disease).
What is immunity?
The nonspecific defenses are not specifically directed against any one
particular invader. The ability of the body to defend itself against specific
invaders (bacteria, viruses, toxins, foreign tissue, cancer cells) in a
specific manner is called immunity.
What is an antigen?
Substances that are recognized by the immune system and provoke
immune responses are called antigens.
256
Two properties distinguish immunity from nonspecific resistance. List and briefly
describe them.
specificity -- The cells of immunity show specificity for particular foreign
molecules (antigens). This also involves the ability to distinguish
“self” from “nonself” molecules.
memory -- The cells of immunity have “memory” for most previously
encountered antigens so that a second encounter prompts an even
more vigorous and faster response.
1.
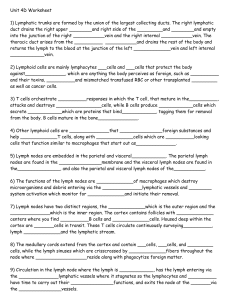
FORMATION OF T CELLS AND B CELLS
What are T cells and B cells? Where do they become immunocompetent?
What does immunocompetence mean?
The cells that carry out immune responses are lymphocytes (T and
B cells) and macrophages antigen-presenting cells).
Both types of lymphocytes, T and B cells, develop from stem cells
in the bone marrow and must then receive immunocompetence in
order to become functional.
B cells become immunocompetent in bone marrow, and then pass
into the blood for distribution throughout the lymphoid tissues.
Immature T cells pass from bone marrow to the blood, enter the
thymus gland, and after a few days emerge as immunocompetent T
cells for distribution throughout the lymphoid tissues.
With immunocompetence, T and B cells acquire several distinctive
proteins on their cell surface that function as antigen receptors.
Each cell is now capable of recognizing a specific antigen and has
therefore gained antigen specificity.
2.
TYPES OF IMMUNE RESPONSES
Describe cell-mediated immunity. What is it effective against?
Immunity consists of two kinds of closely allied immune responses,
both of which are triggered by the presence and recognition of
antigens.
In cell-mediated (cellular) immune responses, T cells proliferate into
several subpopulations (subclones) that are involved in directly
attacking the invading antigen.
257
Cytotoxic (killer) T Cells (CD8) directly destroy antigens by
secreting cytotoxins on to the antigen. Helper T Cells (CD4) aid
both T and B cell responses. Suppressor T cells suppress the
response so that it is controlled.
Memory T cells remain in the lymphoid tissues, allowing a
secondary or anamnestic response that occurs quickly, destroying
the pathogen before signs and symptoms of the disease appear.
Cellular immunity is particularly effective against slowly developing
bacterial infections (tuberculosis, brucellosis), intracellular viruses,
fungi, cancer cells, and transplanted cells and tissues.
Three Phases
a. Recognition
-antigen presentation
- T Cell Activation
(costimulation and
clonal selection)
b. Attack
-role of Helper T cells
- role of Cytotoxic T cells
c. Memory
-memory T cells
-anamnestic response
258
259
Describe antibody-mediated immunity. What is it effective against?
In antibody-mediated (humoral) immune responses, B cells
proliferate to form two subclone populations, plasma cells and
memory B cells.
Plasma cells secrete antibodies specific for the particular antigen
that stimulated the response. Antibodies bind to the antigen and
deactivate it, thus marking it for destruction.
Memory B cells remain in the lymphoid tissues and initiate an
anamnestic (secondary) response so that the pathogens are
destroyed before signs and symptoms of the disease appear.
Humoral immunity is particularly effective against antigens dissolved in bodily fluids (viruses), and bacteria that multiply in
extracellular fluids but do not invade body cells.
Three Phases
a. Recognition
-antigen binds to B cell receptors
-B cell activation
-clonal selection
-plasma cells
-memory B cells
b. Attack
-plasma cell secrete antibodies
-antibodies mark antigen for destruction
c. Memory
-memory B cells
-anamnestic response
260
D. FOUR CLASSES OF IMMUNITY
-Natural active immunity- production of one’s own antibodies after exposure naturally
-Artificial active immunity-production of one’s own antibodies as of a result of
vaccination
-Natural passive immunity- naturally acquiring antibodies by another person
(temporary)
-Artificial passive immunity- acquires antibodies from injection from human or antimal
(temporary)
261