lower genital tract infection

LOWER GENITAL TRACT INFECTION
مشاه دحاولا دبع لوتب
0
د
At birth, the neonate has been exposed to high levels of estrogen and progesterone from the mother and the vagina is lined with stratified squamous epithelium.
Sometimes a baby girl has a withdrawal bleed analogous to a period, as the effect of maternal estrogen wanes. It's possible for trichomonas vaginalis to be transmitted at birth, but the infection usually clears spontaneously.
In young females the vagina is lined with a simple cuboidal epithelium. The PH is neutral and it's colonized by organisms similar to skin commensals. Under the influence of estrogen at puberty, stratified squamous epithelium develops and lactobacilli become the predominant organisms. A drop in the PH accompanies this change to a level of approximately 3.5-4.5.Following the menopause, atrophic changes occur, with a return to bacterial flora similar to that of the skin. The PH rises again to 7. Vaginal discharge can be physiological, infective, malignant or due to other miscellaneous causes like foreign body.
Physiological vaginal discharge:
Physiological vaginal discharge is white becomes yellowish on contact with air, due to oxidation. It consist of desquamated epithelial cells, mucus originate from cervical glands, bacteria and fluid which's formed as transudate from the vaginal wall. More than95% of bacteria present are lactobacilli which metabolise epithelial glycogen into lactic acid thus maintain acidic PH. Physiological discharge increase due to increased mucus production from the cervix in midcycle, pregnancy, and women using combined oral contraceptive pills.
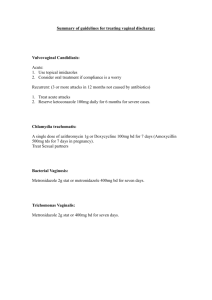
Vaginal candidiasis:
is mycotic disease which's usually caused by yeast candida albicans , a commesal of genital and digestive tracts, 'minority of cases are caused by non albicans spp e.g. C. glabrata, C.krusei, C.tropicalis however the clinical picture of albicans and non albicans spp are indistinguishable clinically there's vulval itching but vaginal soreness and burning may occur non of these symptoms is specific, typically the vulva is red fissured and dry a white curdish discharge that’s adherent to the vaginal wall and cervix is described acute infection is confirmed by the presence of candidal pseudohyphae or budding yeast forms but this is insensitive culture of
1
vaginal swab is the most sensitive test the presence of more than ten yeast colonies support the diagnosis recurrent vulvovaginal candidiasis is defined as 4 or more episodes of symptomatic candidiasis annually incidence prevalence of candida albicans in healthy young women is 20-
25% uncomplicated vulvovaginal candidiasis affect 75% of women at least once in the lifetime recurrence is said to occur in less than 5% aetiology
most episodes occur without obvious cause
small proportions of women treated with broad spectrum ABC subsequently develop vulvovaginal candidiasis as a result of prior colonization
there's strong association with sexual activity
DM
Immunosuppression
Pregnancy, OCP
PROGNOSIS uncomplicated vulvovaginal candidiasis is usually self limiting management
pt should avoid local irritant and tightly fitting underwears
topicaly applied azoles( clotrimazol, econazole, miconazole) no evidence that any imidazole is more effective than the other
4 days course cure over 1/2 of infections, whereas7 days course will cure more than90% of cases
Pregnant women need longer courses than non pregnant
No difference exist in terms of effectiveness and safety antifungal administered by oral or intravaginal routes for treatment of uncomplicated although oral treatment is preferred in non pregnant women
In woman with recurrent symptoms one should exclude DM, other vulval dermatoses like herpes simplex, eczema, lichen sclerosus should be excluded oral or topical antifungal maintenance therapy can be continued for 6 months once or twice a month.
2
Bacterial vaginosis:
It’s characterized by an overgrowth of predominantly anaerobic organism (Gardnella vaginalis, mycoplasma hominis, Bacteroids, mobiluncus)this lead to replacement of lactobacilli and an increase in
PH from a normal 4.5 to 7.BV can arise and remit spontaneously in both sexually active and non sexually active women.
Incidence:
It's the commonest cause of abnormal vaginal discharge in women of child bearing age. Studies in antenatal clinics and gynecological clinic show a prevalence of approximately 12%in the UK.
Risk factors:
It's commoner in Afrocaribbean origin
Those who have IUCD
Higher in women undergo elective termination of pregnancy
Cigarettes smoking
Lesbian women
Clinical features:
50% of proved cases are asymptomatic, symptomatic cases complain of offensive discharge, fishy smelling vaginal discharge not usually associated with itching. There's also a thin white homogenous discharge coating the walls of the vagina and vestibule.
Complications:
Gyn. Complications; BV commoner in women elect termination of pregnancy and is responsible for posttermination endometritis and
PID, vaginal cuff cellulitis and abscess formation following transvaginal hysterectomy, no studies investigate the role of post IUCD insertion endometritis.
Obst. Complications; late miscarriages, preterm labour, preterm premature rupture of fetal membrane and postpartum endometritis.
3
Diagnosis: Amsel's criteria at least 3 of 4 should be present for the diagnosis to be confirmed 1- thin white homogenous vaginal discharge.
2-clue cells on microscope ( epithelial cells their borders obscured due to heavy bacterial groth).
3-PH of vaginal fluid>4.5
4-release of fishy smell on adding alkali (10%koH)
Managemant:
Simple advice against vaginal douching, using of shower gel, and antiseptic bath agents.
Antibiotic for symptomatic cases, women undergo surgical procedures, and some pregnant women
Metronidazole 400-500 mg twice daily for5-7 days
Metronidazole 2 grams single dose
Vaginal metronidazole gel ( 0.75%) once daily for 5 days
Intravaginal clidamycin cream (2%) once daily for 7 days
All these Rx achieve cure rate 70-80% treatment of male partner is not recommended.
Vaginal t richomoniasis :
This is exclusively sexually transmitted can be carried asymptomatically for several months before causing symptoms caused by protozoon trichomonas vaginalis. It can be cquired perinatally and occurs in 5% of babies born to infected mothers.
Clinical features;
10-50% of women are asymptomatic
Vaginal discharge (the classic yellowish green frothy discharge occur in 10-30% of cases only
Vulval itching dysuria and offensive odour
Strawberry cervix appearance occur in 2% of cases in naked eye and in more cases by colposcope
Complications;
4
T .
vag inalis ha s determintal effect on pregnancy and is associated with preterm labour and low birth weight.
Direct observation of a wet smear from the posterior fornix will diagnose40-80% of cases Fineberg-Whittington culture the organism will correctly diagnose95% of infected women, it's sometimes diagnosed on cervical cytology, polymerase chain reaction (PCR) HAVE sensitivities and specificities approching100%.
Treatment ;
most T.vaginalis strain are highly meronidazole sensitive(95% cure rate either 2 g single dose or 400 -500mg twice daily for 5-7 days. The male be adviced not to use alcohol during treatment to avoid disulfiram-like reaction. Treatment failure either due to poor compliance, reinfection, or resistance. Metronidazole is relatively contraindicated in the 1 st TMS of pregnancy, local treatment such as cotrimazole100 mg daily for 7 days can be used.
Other causes of vaginal discharge include atrophic vaginitis, toxic shock syndrome, and Bartholine abscess.
Atrophic vaginitis:
It's common in post menopausal women. Over the 5 years following the cessation of menstruation, the vaginal epithelium atrophies and the lactobacilli are once again replaced by typical skin commensals organisms. this can lead to superficial dyspareunia and vaginal soreness, the treatment of choice is estrogen replacement with either local or systemic estrogen therapy. occaasionaly a true bacterial vaginitis is encountered with either streptococci or other organism. It respond to appropriate antibiotic therapy.
Toxic shock syndrome:
Is a rare condition associated with the retention of tampons or foreign body in the vagina, an over growth of staphylococci producing toxin cause systemic shock with fever, diarrhea, vomiting and an erythematous rash. There's 10% mortality rate, more commonly a FB or retained tampon merely cause an offensive discharge.
Bartholin's abscess:
Bartholin 's gland are situated on either side of the vagina, with their ducts opening in to the vestibule. Cyst can develop if the opening becomes blocked; these present as painless swellings. If they become infected Bartholin abscess develop culture may yield Niesseria gonorrhea, streptococci, staphylococci, mixed anerobes, E coli
Clinically they are hot , tender, swellings adjacent to the lower part of the vagina, treatment is by marsupialization, gland excision indicated for repeated recurrences
5
with damaged gland duct, in women >40 years lesion suspicious of Bartholin's adenocarcinoma .
Infestations :
Pubic lice and scabies are transmitted by close bodily contact, pubic lice attach their eggs to the base of pubic hair. Their claws only attach to thick body hair, so they can only colonize the axillae and eyelashes. Infected individuals may report small itchy papules, or notice depris from the lice on their underwears, treatment is with topical agent like malathion and should be repeated after 7 days partner should be treated as well.
Scabies (sarcoptes scabiei) cause intensly itching popular rash , if acquired during sexual intercourse, it may be initially confined to the genital area it respond to malathion application but symptoms require 6 weeks to resolve completely
6