Lecture Notes - People Server at UNCW
advertisement

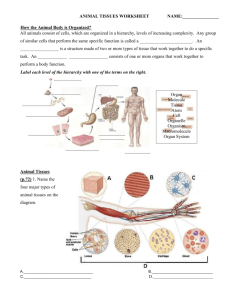
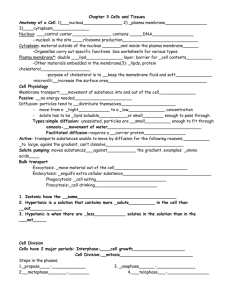
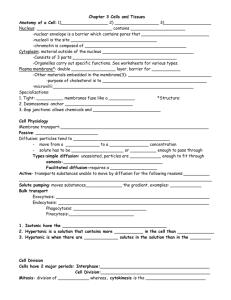
THE TISSUE LEVEL OF ORGANIZATION A. TYPES OF TISSUES List three characteristics of a tissue? 1. 2. 3. Group of similar cells AND their extracellular matrices Share a common embryological origin Function together as a group to carry out particular functions What determines the functions and properties of a tissue? The functions and properties of a tissue are determined by the nature of the cells and the extracellular matrix, if present, created by and surrounding the cells. List the four basic tissue types and give a brief description of each. B. 1. Epithelial tissues – cover the body surfaces; line hollow organs, body cavities, and ducts; form glands 2. Connective tissues – protect and support the body and its organs; binds organs together; store energy reserves as fat; provide resistance to disease in association with the immune system 3. Muscular tissues – responsible for movement and generation of force 4. Nervous tissue – initiate and transmit action potentials (nerve impulses) that help coordinate body activities EPITHELIAL TISSUES 1. GENERAL FEATURES Describe the general features of epithelial tissues. 1. 2. 3. 4. Closely packed cells with little or no extracellular material between them Cells arranged into continuous sheets, in either single or multiple layers Epithelial cells have an apical surface that is exposed to a body cavity, lining of an internal organ, or the exterior of the body. Epithelial cells have a basal surface that is attached to a basement membrane 29 5. 6. 7. 8. 2. The basement membrane (basal lamina) is a connective tissue matrix that attaches the overlying epithelium to the underlying connective tissue Epithelia are avascular, meaning that they have no blood supply. They receive their nutrition by diffusion from the underlying connective tissues. Epithelial have a nerve supply. Since epithelia are subject to a certain amount of wear, tear, and injury, they have a high capacity for mitosis. COVERING AND LINING EPITHELIA a. ARRANGEMENT OF LAYERS b. CELL SHAPES c. CLASSIFICATION Covering and lining epithelia are arranged into continuous sheets of cells consisting of one of three layer types depending upon the function of the tissue. Covering and lining epithelia are also classified according to the shape of the cells that lie on the apical surface of the epithelium. Describe the following: 1. simple epithelium – If the function is absorption or filtration, or the tissue is in an area of minimal wear and tear, the cells form a single layer, and is thus called a simple epithelium. 2. stratified epithelium – If the tissue is in an area with a high degree of wear and tear, then the cells are stacked into layers, and is thus called a stratified epithelium 3. pseudostratified epithelium – A third less common arrangement is the pseudostratified epithelium that has a single layer of cells, so it is simple, but some cells do not reach the apical surface, giving it a multilayered appearance. Describe each of the following: 1. squamous cells – squamous cells are flattened and scalelike 2. cuboidal cells – cuboidal cells are usually cube-shaped in cross-section, being roughly as tall as they are wide 3. columnar cells – columnar cells are tall and cylindrical or somewhat rectangular, and generally taller than they are wide 30 4. d. transitional cells – Transitional cells readily change shape and are found where there is a continuous amount of stretching then relaxation, such as in the urinary bladder. The apical layer may range from squamous to cuboidal. PHOTOMICROGRAPHS tissue location(s) description function(s) simple squamous lining heart (endocardium) and blood vessels (endothelium), lymphatic vessels, alveoli of lungs, glomerular capsule of kidneys, part of serous membranes keratinized form forms epidermis; nonkeratinized forms line mouth and tongue, pharynx, esophagus, anal canal, and vagina lines kidney tubules and small ducts of many glands, covers ovary, forms pigmented epithelium of retina relatively rare; lines larger ducts of some glands and part of the male urethra consists of a single layer of flattened, scalelike cells, much like a tile floor diffusion, osmosis, and filtration consists of multiple layers flattened on surface; cuboidal to columnar in deepest layers consists of a single layer of cube-shaped cells, about as tall as they are wide consists of two or more layers of cells, the upper most being cuboidal in shape single layer of rectangular (columnar) cells, often has interspersed goblet cells protection against wearand-tear not truly stratified; all cells contact basement membrane, but not all reach apical; surface secretion from goblet cells, movement of mucous across surface by ciliary action variable; apical cells vary from squamous to cuboidal depending on degree of stretch of organ allows distention of organ without causing an increase in tension in wall of organ stratified squamous simple cuboidal stratified cuboidal simple columnar pseudostratified transitional 3. lines GI tract from stomach to anal canal, ducts of some glands, gallbladder; ciliated form lines oviducts, uterus, central canal of spinal cord lines much of lower respiratory system down to bronchiolar level; nonciliated form may be found in some gland ducts, epididymis, and part of male urethra urinary bladder, portions of ureters and urethra absorption and secretion protection secretion and absorption GLANDULAR EPITHELIA Glandular epithelium forms the secretory portions of glands. Name the two major types of glands in the body and give a brief description of each. 1. Endocrine glands – endocrine glands are ductless; secrete hormones into the blood 31 2. a. Exocrine glands – exocrine glands secrete their product(s) either onto the apical surfaces of the cells or into ducts for transport to the free surface. STRUCTURAL CLASSIFICATION List the two major structural classifications of exocrine glands and give a brief description of each. b. 1. Unicellular glands – The best example of a unicellular gland is the goblet cell. This single cell secretes its product directly onto the free surface of many epithelia. 2. Multicellular glands – A multicellular gland consists of a secreting organ found deep to the free surface and attached to it via a duct. FUNCTIONAL CLASSIFICATION What is the basis for the functional classification of glands? Functional classification is based on whether a secretion is a product of a cell or consists of entire or partial glandular cells themselves. Describe each of the following: 1. holocrine secretion – In holocrine secretion the cells accumulate secretory product in their cytosol, die, and are discharged with their contents as the secretion. 2. merocrine secretion – In merocrine (eccrine) secretion the cells form a secretory product, store it in the cytoplasm in secretory vesicles, and release it by exocytosis. 3. apocrine secretion – In apocrine secretion vesicles with product accumulate in the apical portion of the cells. That portion pinches off from the rest of the cell to form the secretion. 32 C. CONNECTIVE TISSUES 1. GENERAL FEATURES Name the three basic elements of all connective tissues. 1. 2. 3. cells ground substance (ground substance is a more or less homogeneous, amorphous, water-based background substance in which the specific differentiated elements of a connective tissue are suspended) fibers Name the three basic fiber types of the connective tissues. 1. collagen 2. elastin 3. reticular fibers What is matrix? Matrix is ground substance embedded with fibers that separate the cells. 2. CLASSIFICATION Mature (adult) connective tissues are classified into five categories. List each of them, give their subdivisions, and the primary cell type of each. 1. loose connective tissues areolar tissue (fibroblast) adipose tissue (adipocyte) reticular tissue (fibroblast) 2. dense connective tissues dense regular connective tissues (fibroblast) dense irregular connective tissues (fibroblast) elastic connective tissues (fibroblast) 3. specialized connective tissues cartilage hyaline cartilage (chondrocyte) elastic cartilage (chondrocyte) fibrocartilage (chondrocyte and fibroblast) bone (to be discussed later) blood (to be discussed later) 33 3. PHOTOMICROGRAPHS tissue location(s) description function(s) areolar papillary dermis of skin, hypodermis, mucous membranes, blood vessels, nerves, and around body organs (i.e. everywhere) strength, elasticity, and support adipose hypodermis; around heart, kidneys, and eyes; yellow bone marrow; around joints reticular stroma of liver, spleen, lymph nodes; red bone marrow; basement membranes tendons, aponeuroses, and most ligaments loosely woven fibers embedded in ground substance; many different cell types wander through; fibroblasts form basic tissue adipocytes that store fats, forming a characteristic “signet ring” appearance net work of very short interlacing collagen fibers and fibroblasts collagen fibers arranged in parallel bundles, with fibroblasts scattered between collagen fibers randomly arranged and fibroblasts, forming a sheet elastic fibers that branch freely, forming sheets or ligaments provides extensibility and elasticity to various organs that must be stretched resists compressive forces, provides smooth surfaces for articulation at synovial joints support, fusion (between pubic bones and between vertebrae), deepening of shoulder and knee joints allows structure to be semi-rigid and extensible; structure can return to resting shape support, protection, storage, provides levers for movement; provides for blood cell formation transport of gases, immune function, blood clotting dense regular dense irregular elastic hyaline cartilage fibrocartilage dense fascia, reticular dermis, perichondrium, periosteum, joint capsules, dura mater, membrane capsules, heart valves lung, elastic arteries, trachea and bronchial tree, true vocal cords, vertebral ligaments, suspensory ligament of penis articular surfaces of bones; anterior ribs; nose, parts or larynx, trachea, and bronchial tree; embryonic skeleton pubic symphysis, intervertebral discs, menisci of shoulders and knees elastic cartilage epiglottis, external ear, auditory tubes bone comprises the bones of the skeleton blood within blood vessels and heart Chondrocytes embedded in cartilage matrix rich in collagen fibers consists of scattered Chondrocytes with hyaline cartilage matrix among bundles of collagen fibers Chondrocytes embedded in cartilage matrix rich in network of elastic fibers osteocytes embedded in a mineralized matrix of collagen fibers and ground substance formed cellular elements suspended ina liquid matrix (plasma) provide insulation, energy storage, protection from mechanical injury form framework of organs, binds together smooth muscle cells provides strong attachments between parts strength, support, and protection 34 D. MEMBRANES What is a membrane? An epithelial membrane is formed by a the combination of an epithelium and an underlying connective tissue layer. Name the three true membranes and the one false membrane of the body. mucous membrane (mucosa) serous membrane (serosa) cutaneous membrane (skin or integument) synovial membrane (not a true membrane because there is no epithelium) 1. MUCOUS MEMBRANES In general, where are mucous membranes found? Mucous membranes line body cavities that open directly to the external environment. What is the function of the epithelial layer? The epithelial layer secretes mucous to protect the epithelium by lubricating it and trapping harmful agents. Specifically, what body parts are lined by a mucosa? Mucosae are found lining the respiratory tract, the digestive tract, and the genitourinary tract. 2. SEROUS MEMBRANES In general, where are serous membranes found? Serous membranes line body cavities that do not open to the exterior of the body and cover the external surfaces of the viscera. What are the parietal and visceral layers of a serosa? The portion of the serosa attached to the body wall is called the parietal layer and the portion attached to an organ is called the visceral layer. 35 What is serous fluid, where is it found, and what does it do? Between the layers of the serosa is a small amount of serous fluid that lubricates the two layers and allows the organs to move freely within the cavity 3. CUTANEOUS MEMBRANE The cutaneous membrane (epidermis) will be discussed with the skin. 4. SYNOVIAL MEMBRANE Where are synovial membranes located? They line the joint cavity of synovial (freely movable) joints. Why are they not considered to be true membranes? Synovial membranes are not true membranes because they do not contain an epithelial layer. What is the structure of a synovial membrane? Synovial membranes are composed of areolar connective tissue with elastic fibers and varying amounts of adipose tissue. The cells are synoviocytes that secrete synovial fluid. 36