Inotropic Agents and Other Drugs Used in Heart Failure
advertisement

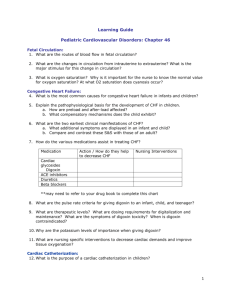
Cardiovascular Pharmacology - Inotropic Agents and Other Drugs Used in Heart Failure Edward JN Ishac, Ph.D. Professor, Pharmacology and Toxicology Smith 742, 828-2127, e-mail: eishac@vcu.edu OBJECTIVES 1. Identify the pharmacologic basis of the following in treating heart failure a. Converting enzyme inhibitors and angiotensin receptor blockers b. Diuretics (Loop , Thiazide, and K-Sparing diuretics) c. Vasodilators d. Cardiac glycosides (Digoxin) e. Inotropics other than digitalis (dobutamine, xanthines) f. Beta Blockers g. Beta natriuretic peptide (Nesiritide) HEART FAILURE: cardiac output inadequate for body demand of oxygen (demand-supply) Prevalence: - heart failure is a common disease - approximately 6 million Americans have symptomatic heart failure - carries a mortality of 20 - 25% per year Causes: - coronary artery disease (main cause, 60-70%) - primary cardiomyopathy - hypertension (main cause for Afro-Americans) - toxic injury by chemicals - congenital or genetic abnormalities - drug: adriamycin Compensated heart failure: - resting cardiac function meets demand - cardiac output may not be sufficient during stress or exercise Congestive heart failure (CHF, decompensated): - resting cardiac function inadequate - ↑venous pressure edema esp. lungs - shortness of breath (dyspnea) - ‘neurohumoral storm’ ↓ Cardiac function → Neuro-humoral activation → ↑Sympathetic NS & RAA system → Tissue remodeling (hypertrophy, ↓ CO) Dr. Ishac CHF & Cardiac Glycosides 2 Hemodynamic changes in congestive heart failure i. ii. iii. iv. v. sympathetic tone (tachycardia) parasympathetic tone activation of renin-angiotensin system blood volume vasopressin release Consequences: - force of contraction - CO, TPR, stroke volume - venous pressure, tissue perfusion - cardiac hypertrophy - Na+ & water retention - edema (especially standing) Figure 1. Treatment Options: Dietary, Lifestyle: - exercise as tolerated - salt restriction Pharmacotherapy: a. Positive inotropic agents: - cardiac glycosides (ie. digoxin) - catecholamines (ie. dobutamine) - phosphodiesterase inhibitors (ie. Milrinone) b. Beta-blockers (ie. Metoprolol caution with use) c. Diuretics (ie. Thiazides, Loop diuretics and K-sparing diuretics) d. Angiotension converting enzyme (ACE) inhibitors (ie. lisinopril) or Receptor-blockers e. Vasodilators (non-inotropic, ie. hydralazine, isosorbide dinitrate) f. Beta type natriuretic peptide (Nesiritide) Dr. Ishac CHF & Cardiac Glycosides Heart Physiology Electrical components: - Action potential (AP) generation (spontaneous) - AP conduction (via specialized conductive system) Excitation - contraction coupling: - key role of IC Ca++ Figure 2a & 2b. Cellular ion movements 3 Dr. Ishac CHF & Cardiac Glycosides 4 DIGITALIS GLYCOSIDES I. INTRODUCTION AND HISTORY The steroidal glycosides of digitalis have the unique ability to increase not only the contractility of the failing heart, but also its mechanical efficiency by means of a decrease in heart size which decreases O2 consumption. Plant extracts containing cardiac glycosides (white and purple foxglove; Digitalis lanata and D. purpurea) have been used in various parts of the world since the ancient Egyptians (3000 years ago). The modern use of digitalis in medicine stems from the classical observations of William Withering in 1785. Withering used digitalis with success in treating "dropsy", but was unaware of the action of digitalis on the heart. Only within the past 50 years have the actions of digitalis on the heart and their cellular mechanisms become well understood. Chemistry: Digoxin (USA), Digitoxin (Europe) i. steroid nucleus: - lipophilic, essential for activity ii. unsaturated five-membered lactone ring: - hydrophilic, essential for activity - opening the ring loss of activity - saturation loss of activity iii. series of sugars linked to C 3 of the steroid nucleus - non-essential, hydrophilic Figure 3. Structure of Digoxin Dr. Ishac II. CHF & Cardiac Glycosides 5 PHARMACOLOGIC ACTIONS OF DIGITALIS Congestive Heart failure: use decreasing for acute and chronic treatment Arrhythmias: In atrial tachycardia, atrial flutter and atrial fibrillation, the depressant action of digitalis on the A-V node conduction (via increasing vagal activity) protects the ventricles from excessive atrial impulses. A. Effect at the Cellular Level Ion movements into and out of cell Cardiac glycosides (CG): potent, highly selective inhibitors of Na+/K+ ATPase (Na+ pump) Na+/K+ ATPase: - membrane bound transporter (3 Na+ / 2 K+) - found all over the body, /-subunits - extracytoplasmic binding site for CG - phosphorylation of cytoplasmic -subunit stabilize CG binding - [K+]EC dephosphorylates -subunit CG binding (ie. ACEI, ARBs, K-sparing diuretics) - [K+]EC CG intoxication (ie. Thiazide, loop diuretics) Inhibition of (Na+, K+-ATPase) See Figure 2b exchange Na+ - K+ (3:2) [Na+]IC (10 10.5 mM) Na+ - Ca++ exchange (deploarized, 3:1) [Ca++]IC SR uptake Ca++ ( stores) contractile force Therapeutic consequence of CG: - moderate but persistent positive ionotropic effect, sensitivity of the baroreceptor reflex CO sympathetic activity HR and vascular tone pre- and afterload heart size oxygen demand CO renal blood flow improved GFR renin-angiotensin activity level Na+ excretion body Na+ volume + vascular reactivity pre- and afterload Dr. Ishac CHF & Cardiac Glycosides 6 B. Cardiac Effects 1. Increase in contractile force of myocardium (inotropic effect) 2. Increase in vagal activity - cardiac slowing (chronotropic effect) 3. Major effects on electrophysiologic parameters a. decreased A-V conductivity due to decreased conduction velocity and an increase in the refractory period b. EKG changes 1. T wave becomes inverted 2. ST segment becomes depressed 3. PR interval becomes prolonged 4. Heart size is decreased due to more complete ventricular emptying Table 1. Summary of the cardiovascular effects of CHF and the results of digitalis administration Figure 4. Use of the Frank-Starling mechanism as a compensation for congestive heart failure. Curves depict ventricular function in normal subjects and in those with congestive heart failure (CHF) and heart failure after treatment with digitalis. The points N through D represent in sequence: initial reduction of contractility due to congestive heart failure (N to A); use of FrankStarling compensation to maintain cardiac output (A to B); increase in contractility when digitalis is administered (B to C); and reduction in the use of Frank-Starling compensation, which digitalis allows (C to D). Of note is the fact that points N, B and D all lie on the same line in the vertical axis and thus all represent the same cardiac output, but each is on a different end-diastolic pressure Dr. Ishac CHF & Cardiac Glycosides 7 III. PHARMACOKINETIC CHARACTERISTICS: 1. Digoxin (USA; Lanoxin, Lanoxicaps) a. Absorption - from GI tract is good, but is incomplete and can be variable due to gut bacteria (10% of population resistant, Eubact. lentum) b. Fate - 15% liver metabolism, 85% excreted unchanged in the urine. 2. a. b. Digitoxin (Europe; Crystodigin) Absorption - from GI tract nearly complete. Fate - undergoes metabolism to other active glycosides, including digoxin. Most digitoxin is eventually converted to inactive metabolites. Only 5-10% of digitoxin is excreted unchanged. 3. Ouabain - no longer in clinical use in the USA Agent Route Biovail.% Bound% Peak effect Digoxin Digitoxin oral, iv oral, iv 45-85 >90 25 90 6 hr 12 hr VI. TOXICITY: Narrow therapeutic window (50%): T1/2 35 hr (kidney) 6-7 day (liver) oscillatory afterdepolarization ventricular tachycardia Cardiac Glycoside (CG) Toxicity: ventricular tachycardia, delirium, fatigue, weakness, dizziness, nausea, vomiting, vision/light disturbances (halo effect, mainly yellow and green, [van Gogh]) Figure 5a & 5b: Therapeutic index and toxicity of cardiac glycosides Dr. Ishac CHF & Cardiac Glycosides Important interactions: a. Hypokalemia CG binding, ↑effect (Thiazides & Loop diuretics) b. Hyperkalemia ↓CG binding, ↓effect (ACEIs/ARBs & K-sparing diuretics) b. Quinidine displaces CG from plasma binding (↑effect) c. Ca++-blockers enhance effect, ie. increase toxicity (eg. verapamil) d. Catecholamines enhance toxicity (synergist effect) e. Amiodarone: serum concentration of cardiac glycosides (↓clearance) f. Cholestyramine decrease CG absorption, ↓effect g. Thyroid dysfunction Hyperthyroidism ↓[CG)], Hypothyroidism ↑[CG)] h. Antibiotics CG bioavailability (eg. erythromycin) i. Alteration in renal function can affect digoxin concentration Treatment of Toxicity: a. discontinue cardiac glycoside or alter dose b. discontinue K+ depleting diuretics or add K-sparing c. administer K+ arrhythmias (esp. with diuretics) d. use of antiarrhythmic agent eg. lidocaine, phenytoin e. use of antidigoxin antibodies eg. digoxin immune FAB (expensive) CATECHOLAMINES: Usually used (iv) in acute decompensated HF, sometimes used long-term. Can induce angina and arrhythmias discontinue or reduce dose Dobutamine (Dobutrex); Dopamine (second line agent) Stimulation of cardiac beta-1 receptors by dobutamine results in an increase in contractile force, but relatively little increase in heart rate. Dobutamine does not activate renal dopamine receptors. cAMP Ca++ influx CO. Figure 6: Actions of dobutamine and phosphodiesterase inhibitors. 8 Dr. Ishac CHF & Cardiac Glycosides 9 CARDIOACTIVE BIPYRIDINES: PHOSPHODIESTERASE INHIBITORS: Inamrinone (previously Amrinone), Milrinone Inhibition of specific phosphodiesterase III. PDE inhibition leads to increased cyclic AMP content of cardiac muscle and an increase in intracellular calcium via phosphorylation of Ca-channel. - used in acute and chronic HF - cAMP Ca++ influx CO (as per catecholamines) - can decrease preload and afterload - higher mortality reported with chronic use - bronchodilation, benefit in asthma individual OTHER AGENTS USED IN HEART FAILURE: -discussed in detail in other sections of cardiovascular course (Hypertension) a. Converting enzyme inhibitors / Angiotensin II receptor blockers (ARBs) Frontline agents. Increasing use (e.g. Lisinopril, Enalapril) and Angiotensin II receptor blockers (e.g. Losartan, Valsartan) - decrease preload and afterload, increase survival, tissue remodeling Renin Inhibitor: Aliskiren, newest agent, actions similar to ACEIs, no cough Actions of Angiotensin-Converting Enzyme (ACE) Inhibitors/ARBs - decrease activity of sympathetic NS - TPR, CO unchanged, HR unchanged - no reflex HR, probably due to resetting () of baroreceptor reflex sensitivity - aldosterone production Na/water retention - bradykinin level (inhibit metabolism, only ACEIs) - improves intrarenal hemodynamics - less effective in elderly and Afro-Americans Adverse effects: hyperkalemia, dry cough (ACEI only), loss of taste (Zn loss), angioedema (<1%, less with ARBs), glossitis (<5%), tetrogenic (CI: pregnancy & renal artery stenosis) ARBs recommended if can not tolerate ACE inhibitors Dr. Ishac CHF & Cardiac Glycosides 10 b. Diuretics: Frontline agents: decrease preload and increase fluid excretion 1. Loop diuretics (Furosemide) - Inhibit Na-K-2Cl ion cotransporter, ↓Na+, H2O reabsorption: ascending loop of henle, hypokalemia, hypomagnesemia, hypocalcemia ototoxicity, most potent 2. Thiazides (Hydrochlorothiazide, Metolazone) - Inhibit Na-Cl cotransporter, ↓Na+, water reabsorption in distal convoluted tube, hypokalemia, hypercalcemia, ↑uric acid→gout, DM-2, photosensitivity 3. K+-sparing (Spironolactone, Eplerenone) - aldosterone antagonism at collecting tube, hyperkalemia, least potent, adjunct, decreases mortality, tissue remodeling, gynecomastia c. Vasodilators: Good adjuncts, can decrease preload and afterload Adverse effects: reflex tachycardia, headache, nausea, sweating, flushing 1. Not Ca-channel blockers 2. Hydralazine: direct vasodilation, mainly afterload Bidil: combination of Isosorbide dinitrate and Hydralazine (FDA approved 2005 for use in Afro-Americans). Adverse effect: Lupus reaction 3. Nitrates: NO/cGMP; decrease preload and afterload - Nitroprusside, acute use (prolonged use can cause cyanide toxicity) d. Beta blockers: (e.g., Metoprolol, Carvedilol and Bisoprolol; EBM, FDA approved) Good agents (not all) in CHF Classes II-III, decrease mortality. Increasing use Beneficial effects include: reduction of tachycardia and other adverse effects of high catecholamine levels, alpha-1 blocking action with carvedilol, peripheral vasodilator effects, blockade of renin secretion and scavenging of O2 free radicals CI: decompensated HF, mental depression, bronchospasm, severe bradycardia Adverse effects: - effects enhanced in elderly - myocardial reserve (blockade of cardiac 1-ARs) - fatigue, dizziness - asthma (blockade of bronchial beta2-ARs) - peripheral vascular insufficiency - diabetes (blockade of hepatic beta2-ARs) - CNS: nightmares, mental depression, insomnia - withdrawal syndrome (supersensitivity, rebound HT) - may worsen Raynand’s syndrome e. Beta-type natriuretic peptide [Nesiritide (Natrecor)] Increasing use for severe CHF (Class IV), iv. Administration (T1/2 – 18 mins) Binds to a receptor on the surface of the vascular smooth muscle cell and increases cGMP, leading to smooth muscle relaxation and vasodilation. Arterial and venous dilation decrease preload and afterload. Dilation of afferent renal arterioles increases GFR and sodium reabsorption, leading to diuresis. The SNS and RAA systems are also suppressed. Main adverse effect: - hypotension Dr. Ishac CHF & Cardiac Glycosides GUIDELINES: PHARMACOTHERAPY OF HEART FAILURE (2004) NYHA Heart Failure Classification Pharmacotherapy Class I (no limitations on activity) ACE Inhibitor/AT-1 - RB Class II (slight, mild limitation of activity, comfortable at rest) Bi-Ventricle Class III pacing (marked limitation of Bidil activity, only comfortable at rest) Bi-Ventricle Class IV pacing Bidil (complete rest, confined to bed or chair) Digoxin*, Furosemide, ACE Inhibitor/AT-1 - RB, Beta blocker Digoxin*, Furosemide, Thiazide, ACE Inhibitor/ AT-1 - RB, Beta blocker/ K+-sparing Digoxin*, Furosemide (IV), Thiazide, ACE Inhibitor/AT-1 Receptor blocker, K+-sparing/Inotropic Therapy/ Beta-Natruretic Peptide *Recommended Digoxin not to be used in females for routine CHF, higher mortality. Recommended Pharmacotherapy of CHF requires 4 or more agents Classes II-IV AT-1 – RB: Angiotensin II Type 1 Receptor blockers recommended if cannot tolerate ACEI Bidil: Isosorbide dinitrate & hydralazine (ISDN), effective for Afro-Americans PHARMACOTHERAPY SUMMARY: • Improved survival – ACE inhibitors/ARBs, Beta-blockers, K-sparing • Increased mortality – Phosphodiesterase III inhibitors (chronic) • Neutral on survival – Digoxin, Loop diuretics, Thiazides • Quality of life – Digoxin, Loop diuretics, Thiazides, Beta-blockers • Reduction of edema – Loop diuretics, Thiazides • Tissue Remodeling – ACE inhibitors/ARBs, K-sparing • Prevention of ischemia – Beta-blockers, Anticoagulant therapy • Hemodynamic improvement: All agents – ACEI, ARBs, Digoxin, Diuretics, Beta-blockers, K-sparing 11 Dr. Ishac CHF & Cardiac Glycosides 12 ACC/AHA vs NYHA Classification ACC/AHA (2001) NYHA (2004) A Asymptomatic with no heart damage but have risk factors for heart failure. No equivalent B Asymptomatic but have signs of structural heart damage I (Mild) C Have symptoms and structural heart damage II (Mild) D Endstage disease with advanced structural heart disease and marked symptoms at rest and require specialized interventions. IV Unable to carry out any physical activity (Severe) without discomfort. Cardiac insufficiency at rest. No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, or dyspnea. Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in fatigue, palpitation, or dyspnea. III Marked limitation of physical activity. (Mod.) Comfortable at rest, but less than ordinary activity causes fatigue, palpitation, or dyspnea. LEARNING RESOURCES Recommended Reading: Basic and Clinical Pharmacology, B.G. Katzung (ed.), 10th ed., 2009, Ch. 13, pp. 209-224.