GUEST ESSAY - Cengage Learning
advertisement

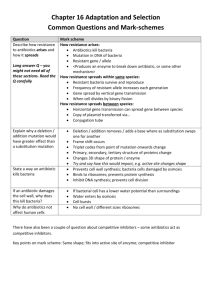
GUEST ESSAY The Current Peril of Antibiotic Resistance Paul F. Kamitsuka, M.D. Paul Kamitsuka is an infectious disease expert and physician in Wilmington, North Carolina. He is also clinical associate professor at the University of North Carolina School of Medicine and a guest lecturer on infectious diseases at Harvard Medical School. He received his medical degree at Harvard Medical School, where he later served as a research fellow in infectious diseases. A few years ago I picked up an infection while in the hospital and I credit Dr. Kamitsuka's expertise with saving my life. When most of us seek medical attention for an infection, we naturally assume that there is an antibiotic that will speed up our recovery. After all, it has been seven decades since the discovery of penicillin. Whereas "new" infections such as Legionnaire's disease or AIDS occasionally arise for which effective therapies must be discovered, medical science has had decades of experience treating more common ailments such as strep throat, bacterial pneumonia, or staph infection of the skin. Surely with all that experience, and with all of the antibiotics that have been developed since penicillin, the treatment of such infections must by now be a routine, almost trivial matter. Or so it would seem. In reality, microorganisms are constantly threatening the utility of our antibiotics, and in many cases have evolved ways to successfully disarm them. Consider pneumococcus, for example, which is a kind of strep bacteria that is the most common cause of pneumonia and meningitis in the United States. Just a decade ago, penicillin–resistance among pneumococcus was almost unheard of in the United States. Now over 25% of all pneumococcus isolates are at least partially resistant, rendering penicillin useless in many instances. Surely, one might think, there are new antibiotics that may take the place of penicillin. In the case of pneumococcus, there are other options but resistance to even these antibiotics is quickly emerging. The fact is that we are steadily losing the race to find new antibiotics to treat resistant organisms. Strains of bacteria already exist for which no effective treatments are left. The emergence of antibiotic resistance amounts to an example of biological evolution occurring at a highly accelerated pace. Biological evolution occurs when Copyright ©2005 Brooks/Cole, a division of Thomson Learning, Inc. Thomson Learning is a trademark used herein under license. members of a species acquire a genetic trait that confers a survival advantage. As a consequence of this advantage, the trait is more likely to be passed on to the next generation and eventually predominates within the population as long as its presence remains advantageous. In the case of antibiotic resistance, the genetic trait enables the bacterium to survive exposure to the antibiotic. Only a tiny proportion of the bacterial population may harbor the resistant trait at first. Because these are the bacteria most likely to survive, however, over the next few generations these resistant bacteria become predominant. Several factors have contributed to the speed which antibiotic resistance has evolved. First, is the fact that bacteria replicate with generation times as short as 20 minutes. Thus, resistance may evolve within the time course of even a single infection—that is, within only a few days as opposed to the prolonged evolutionary time frame we usually think of. The second factor that accelerates the pace at which antibiotic resistance evolves is that bacteria exchange genetic information with extraordinary frequency, and not just when actual replication is occurring. Moreover, such exchange may occur not only within members of the same species, but also among members of unrelated species. In contrast, genetic exchange among mammals, for example, only occurs within members of the same species and only at the time of mating. Bacteria harbor their genes not only on chromosomes, but also on mobile genetic elements, such as plasmids or transposons. Bacteria may transfer plasmids to each other through a process called conjugation. If the plasmid carries a gene encoding antibiotic resistance, then the recipient of the plasmid will become antibiotic–resistant and pass this trait on to its progeny and to other bacteria. Transposons, or "jumping genes," are segments of genetic material that may jump from chromosome to plasmid, or vice versa. They are one mechanism by which resistance genes residing on chromosomes may be transferred to plasmids, and then to other bacteria via conjugation. It is a process akin to a computer software program being copied from the hard drive of one computer and then passed on to other computers. There are numerous examples of bacterial plasmids that harbor antibiotic resistance genes. Gram–negative bacteria, which are common causes of infections of the urinary tract and lung, routinely carry resistance plasmids. These plasmids enable bacteria to inactivate antibiotics through a variety of different means. Some carry genes that encode enzymes that chemically destroy antibiotics such as Copyright ©2005 Brooks/Cole, a division of Thomson Learning, Inc. Thomson Learning is a trademark used herein under license. penicillin. Others may harbor mutant genes that render antibiotics such as tetracycline ineffective by changing the target site to which the antibiotic binds and exerts its antibacterial activity. One example of a transposon of particular medical significance is one that enables bacteria called Enterococcus to be resistant to the antibiotic vancomycin, an antibiotic that acts by binding to the cell wall of the bacteria and interfering with replication. This transposon includes a set of genes that encodes the production of a slightly altered bacterial cell wall so that vancomycin can no longer bind and exert its antibacterial activity. Another example involves highly virulent Staphyloccous bacteria, which is the number–one cause of infection in the United States. Some forms of Staphyloccous are resistant to all antibiotics except vancomycin. What would happen if the transposon encoding vancomycin resistance in Enterococcus were to jump onto a plasmid and be transferred to Staphyloccous ? Such an event, as it turns out, has already occurred under laboratory conditions and outside the lab. In 1998, doctors were shocked to learn of three cases in the United States of this bacterium developing resistance to the last antibiotic (vancomycin) capable of readily killing it. The third factor that favors the rapid emergence of antibiotic resistance among bacteria is our own antibiotic use. The fact that so much antibiotic resistance exists today is testimony to the extraordinary amount of antibiotics we use. Unfortunately, much of this use is unnecessary. The sad legacy of antibiotic use has been one of overuse followed by resistance, followed by the introduction of new antibiotics, and overuse of these agents, followed by the emergence of resistance to these, and so on. Unfortunately, emerging resistance is outpacing the ability of pharmaceutical companies to keep up. Overuse of antibiotics occurs in several different settings. Antibiotics are vastly overused in clinics and hospitals. Viruses that do not respond to antibiotics cause most cases of the common cold, sore throat, or bronchitis. Nonetheless, patients expect to be treated with an antibiotic. Health care providers are leery of disappointing them, and reluctant to spend the time convincing the patient otherwise. In the hospital setting, antibiotics are also used improperly. Rather than making the effort to obtain suitable specimens for culture and sensitivity determination to enable the selection of the narrowest–spectrum older agent that will effectively treat the infection, health care providers often choose the newest Copyright ©2005 Brooks/Cole, a division of Thomson Learning, Inc. Thomson Learning is a trademark used herein under license. "broad–spectrum" antibiotic. Resistance to the newer agents then occurs and future antibiotic options are curtailed. Another setting in which antibiotics are overused is in agriculture. Antibiotics are often added to animal feed. In the short term, this may reduce the incidence of infection among livestock, allowing animals to grow larger and faster. However, increasing data suggest that such practices may be increasing resistance levels of bacteria to which humans are ultimately exposed. A final factor that favors the rapid emergence of resistance is the inadvertent spread of resistant strains from person–to–person, or from place to place. Resistant bacteria may survive in the hospital environment. Furthermore, health care providers who fail to wash their hands between patient contacts may inadvertently spread resistant bacteria from one patient to the next. From a geographic standpoint, the advent of jet travel has meant that resistant organisms may spread from one locale to another. So what can be done about the problem of antibiotic resistance? Evolutionary principles dictate that first and foremost we must reduce the selective pressure favoring resistance by curtailing the unnecessary use of antibiotics. In controlled settings where this has been done, such as in individual hospitals with regard to specific antibiotics, resistance levels have fallen. No longer can we assume that new and better agents will appear in time to rescue us from therapeutic peril. The answer will lie in the disciplined judicious use of existing agents, and in measures that reduce the spread of resistant isolates in hospital settings. Critical Thinking 1. What do you believe are the three most important things we should do to reduce the development of genetically resistant infectious bacteria? 2. Use the library or the Internet to what progress is being made in dealing with this problem. Copyright ©2005 Brooks/Cole, a division of Thomson Learning, Inc. Thomson Learning is a trademark used herein under license.