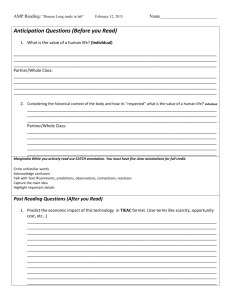
Signs of lung damage from smoking
advertisement

Physiology 1 Respiratory Case Study Name ________________________ Please read Chapter 17 and review Chapter 16 before you complete this case study. Part I. Smoking seriously hurts your lungs: 1. Smoking damages the lungs' natural cleaning and repair system and traps cancer-causing chemicals in the lungs. Smoking destroys the tiny hairs (cilia), which line the upper airways and protect against infection. Normally, there is a thin layer of mucous and thousands of these cilia lining the insides of your breathing tubes. The mucous traps the little bits of dirt and pollution one breathes in, and the cilia move together like a wave to push the dirt-filled mucous out of the lungs. Then one coughs, swallows, or spits up the mucous, and the dirt is out of the lungs. When the lungs' natural cleaning and repair system is damaged, germs, dirt and chemicals from cigarette smoke stay inside the lungs. This puts smokers at risk for chronic cough, chest infections, lung cancer and COPD. Learn more about what's in cigarettes. 2. Smoking permanently damages the alveoli (air sacs) in the lungs and causes emphysema, making it hard to breathe. The alveoli, little air sacs at the tips of your lungs, are built like tiny, stretchy balloons. As we breathe in, the alveoli help us absorb oxygen into our body, and as we breathe out, alveoli help get rid of the waste gas carbon dioxide. Smoke damages the lungs so much that the alveoli become less stretchy. This means it's harder for the lungs to take in the oxygen we need and harder to get rid of carbon dioxide. When the alveoli are damaged like this, smokers can feel short of breath and tired. Their heart has to pump much harder to give their body the oxygen it needs. Over time, this damage can lead to COPD and heart disease. Signs of lung damage from smoking It's common for smokers to ignore or downplay the symptoms of lung damage: o feeling out of breath when walking up a short flight of stairs o coughing o spitting up mucous o repeat chest infections These are not signs of aging or simply being out of shape. These are real signs of the damage that smoking is doing to your lungs. If you have these signs of smoking damage to your lungs, see you doctor. Unless you do something now, these symptoms will keep getting worse. How smoking hurts the rest of our body Smoking doesn't just damage our lungs. There are over 4,000 dangerous chemicals in cigarettes, cigars and pipes smoke for example: carbon monoxide (found in car exhaust), arsenic (rat poison) , ammonia (found in window cleaner), acetone (found in nail polish remover) , hydrogen cyanide (gas chamber poison), napthalene (found in mothballs), sulphur Compounds (found in matches), lead, volatile Alcohol , formaldehyde (used as embalming fluid), butane (lighter fluid). Many of these chemicals are cancercausing (carcinogen).It puts you at high risk for dozens of other serious disease, including cancer. Read more about the health effects of smoking. Modified from Canadian Lung Association.http://www.lung.ca/protect-protegez/tobacco-tabagisme/factsfaits/index_e.php 1 II. Pulmonary Test Pulmonary test is used to evaluate the symptoms and sign of lung diseases and to screen the risk of pulmonary diseases. Spirometry is the measurement of the air movement and lung capacity. To provide an accurate diagnosis, pulmonary test is usually companied with other tests. In this exercise, we just want to learn the different aspects of a pulmonary test and its relationship with cardiovascular system. Figure 1 shows the components of the respiratory cycle. Three of these components are important. They are the forced vital capacity (FVC), the forced expiratory volume in one second (FEV1) and the FEV1/FVC ratio. Typically, an FEV1 / FVC ratio below 0.70 indicates that a patient is suffering from obstructive lung disease. Table 1 compares the obstructive and restrictive pulmonary diseases. Obstructive pulmonary disease refers to a group of diseases that are caused airflow blockage and narrowing of airways. It includes emphysema, chronic bronchitis, and in some cases asthma. Restrictive lung diseases decrease the total volume of air the lungs can hold, due to a decrease in the elasticity of the lungs or the chest wall to expand during inhalation. Examples of restrictive lung diseases are sarcoidosis and pulmonary fibrosis. Figure 1 Lung capacity ( diagram from www. Hakeem-sy.com) Part III Case study of a smoker Joe Smith is a 69-year-old male with a 50-year history of smoking 2 packs of cigarettes a day (i.e. 100pack-year smoking history). Over the past 5 years, he has become increasingly short of breath. At first, he noticed this only when exercising, but now he is even short of breath at rest. Over the past two years, he has had several bouts of lower respiratory tract infection treated successfully with antibiotics. His shortness of breath hasn't subsided, and his breathing is assisted by use of his accessory muscles of respiration. The microscopic changes of his lung are typical for smokers like him. Normal lung His the 2 pulmonary function testing graph below: revealed The lung of Joe Smith Figure 2 Joe’s Pulmonary Function Test Questions: 1) Based on the figures 1 and 2 above and page 472 figure 16.16 of your text book, fill in the following data for Joe: i) tidal volume (TV) ____________ ii) inspiratory reserve volume (IRV) ______________ iii) expiratory reserve volume (ERV) _______________ iv) forced vital capacity (FVC) ______________ v) forced expiratory volume in one second FEV1 ___________________ vi) FEV1 / FVC ratio ___________ b) What pattern of lung disease may result in this FEV1/FVC ratio? _________________ 2) Based on the information given on Joe above and your knowledge about the smokers in general, describe the changes at microscopic level occurring in Joe's lungs. 3) Compare the given histology slides of normal lung on page 2, emphysema lung (from lecture) and Joe’s lung, does he seems to have emphysema? 4) What effect do these microscopic changes have on Joe's ability to transfer oxygen and carbon dioxide in the lungs? 3 5) Define hematocrit. 6) Blood testing showed that Joe's hematocrit to be 59% (normal = 42-54%). Why was his hematocrit so high? Explain the physiological mechanisms that contribute to his high hematocrit (include sensor, signal molecule and the organ that release it). 7) Joe’s arterial blood tests revealed the following: pO2 = 73 mm Hg (normal= 80-105 mm Hg) pCO2 = 50 mm Hg (normal 35- 45 mm Hg) pH = 7.32 (normal = 7.35-7.45) Hb-O2 sat (hemoglobin-oxygen saturation) = 84% (normal = 95-98%) i. Why was Joe's pCO2 increased above normal? ii. Define pH. iii. Why was his arterial blood pH below normal? (Hint: include chemical reaction formula) iv. How is the breathing monitored and regulated in a normal human? v. Joe's pO2 is clearly below the normal range. One's first instinct might be to give him air to breathe that is 100% oxygen. Why would this be dangerous for him (hardest question, give it a try anyway)? 8) Why is Joe susceptible to lower respiratory tract infections? 4