RA Messages dated November 16, 2006
advertisement
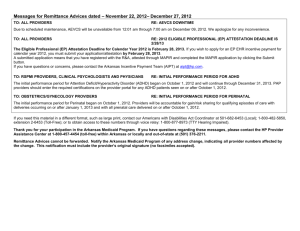
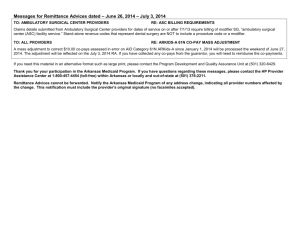
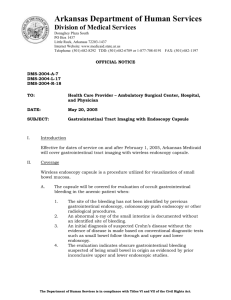
Messages for Remittance Advices dated November 16, 2006 – November 22, 2006 TO: ALL DDTCS PROVIDERS RE: PEN AND INK CHANGES TO DDTCS UPDATE # 78 DDTCS Provider Manual Update #78 includes an error in section 212.000, part B. The words “nursing facility” are incorrect and should be deleted. Please make a pen and ink change in this section of the update. This will be corrected in the next provider manual update. TO: ALL PROVIDERS RE: PSYCH REDUCTIONS Currently Psych reduction payments are not being paid on cross-overs sent from Medicare. This issue is being worked on and you will be notified once a resolution is in place. In order to receive payment for psych reduction, please do the following: Submit an adjustment with a corrected crossover claim, adding the psych reduction to the co-insurance amount. Mail To: EDS Attention: Adjustments P.O. Box 8036 Little Rock, AR 72203 TO: ALL PROVIDERS RE : NEW CLAIM FORMS At this time we are not accepting the new HCFA-1500(version 08/05), UB-04(CMS-1450) or the 2006 ADA Dental claim forms, which accommodate the National Provider Number and other important changes. Notification will be sent to the provider community when we are able to start accepting these claim forms. TO: HOSPITALS, CRITICAL ACCESS HOSPITALS AND REHABILITATIVE HOSPITAL PROVIDERS RE : BILLING FOR BENEFICIARY’S OUTPATIENT HOSPITAL CLINIC When billing Medicaid for the treatment/examination room, supplies, staffing etc. (i.e. the facility fee) for a beneficiary’s outpatient hospital clinic visit, always use procedure code T1015 and Modifier U1. Failure to include Modifier U1 in an outpatient hospital clinic charge may result in an overpayment to the provider which must be refunded to Medicaid. TO: ALL PROVIDERS RE : TANDEM EDITS In order to successfully adjust claims electronically (frequency code 7), do not alter the following items in the original claim: provider ID, recipient ID, the number of details, and the claim type. There are edits in place for each of these items excluding the number of details. Edit Z820-Recipient ID/Claim record mismatch was modified to reject claims with a detail count that differs from the detail count on the original claim. If you wish to change the number of details, void the original claim (frequency code 8), and submit a new claim (frequency code 1) If you need this material in an alternative format, such as large print, please contact our Americans with Disabilities Act Coordinator at (501) 682-6789 or 1-877708-8191. Both telephone numbers are voice and TDD. Thank you for your participation in the Arkansas Medicaid Program. If you have questions regarding these messages, please contact the EDS Provider Assistance Center at 1-800-457-4454 (toll-free) within Arkansas or locally and out-of-state at (501) 376-2211. Remittance Advices cannot be forwarded. Notify the Arkansas Medicaid Program of any address change, indicating all provider numbers affected by the change. This notification must include the provider’s original signature (no facsimiles accepted).