RA Messages dated November 23, 2006
advertisement
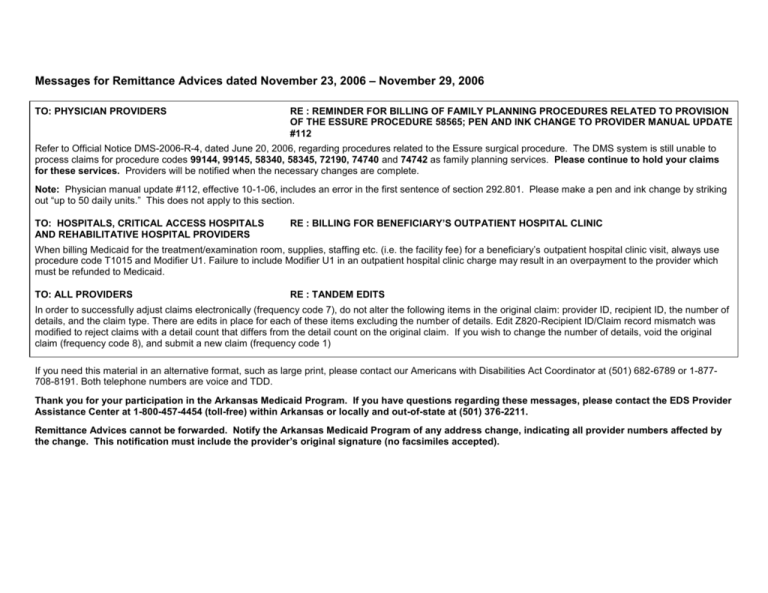
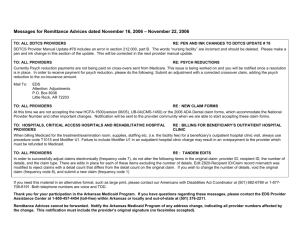
Messages for Remittance Advices dated November 23, 2006 – November 29, 2006 TO: PHYSICIAN PROVIDERS RE : REMINDER FOR BILLING OF FAMILY PLANNING PROCEDURES RELATED TO PROVISION OF THE ESSURE PROCEDURE 58565; PEN AND INK CHANGE TO PROVIDER MANUAL UPDATE #112 Refer to Official Notice DMS-2006-R-4, dated June 20, 2006, regarding procedures related to the Essure surgical procedure. The DMS system is still unable to process claims for procedure codes 99144, 99145, 58340, 58345, 72190, 74740 and 74742 as family planning services. Please continue to hold your claims for these services. Providers will be notified when the necessary changes are complete. Note: Physician manual update #112, effective 10-1-06, includes an error in the first sentence of section 292.801. Please make a pen and ink change by striking out “up to 50 daily units.” This does not apply to this section. TO: HOSPITALS, CRITICAL ACCESS HOSPITALS AND REHABILITATIVE HOSPITAL PROVIDERS RE : BILLING FOR BENEFICIARY’S OUTPATIENT HOSPITAL CLINIC When billing Medicaid for the treatment/examination room, supplies, staffing etc. (i.e. the facility fee) for a beneficiary’s outpatient hospital clinic visit, always use procedure code T1015 and Modifier U1. Failure to include Modifier U1 in an outpatient hospital clinic charge may result in an overpayment to the provider which must be refunded to Medicaid. TO: ALL PROVIDERS RE : TANDEM EDITS In order to successfully adjust claims electronically (frequency code 7), do not alter the following items in the original claim: provider ID, recipient ID, the number of details, and the claim type. There are edits in place for each of these items excluding the number of details. Edit Z820-Recipient ID/Claim record mismatch was modified to reject claims with a detail count that differs from the detail count on the original claim. If you wish to change the number of details, void the original claim (frequency code 8), and submit a new claim (frequency code 1) If you need this material in an alternative format, such as large print, please contact our Americans with Disabilities Act Coordinator at (501) 682-6789 or 1-877708-8191. Both telephone numbers are voice and TDD. Thank you for your participation in the Arkansas Medicaid Program. If you have questions regarding these messages, please contact the EDS Provider Assistance Center at 1-800-457-4454 (toll-free) within Arkansas or locally and out-of-state at (501) 376-2211. Remittance Advices cannot be forwarded. Notify the Arkansas Medicaid Program of any address change, indicating all provider numbers affected by the change. This notification must include the provider’s original signature (no facsimiles accepted).