Disproportionate Share Questionnaire
advertisement
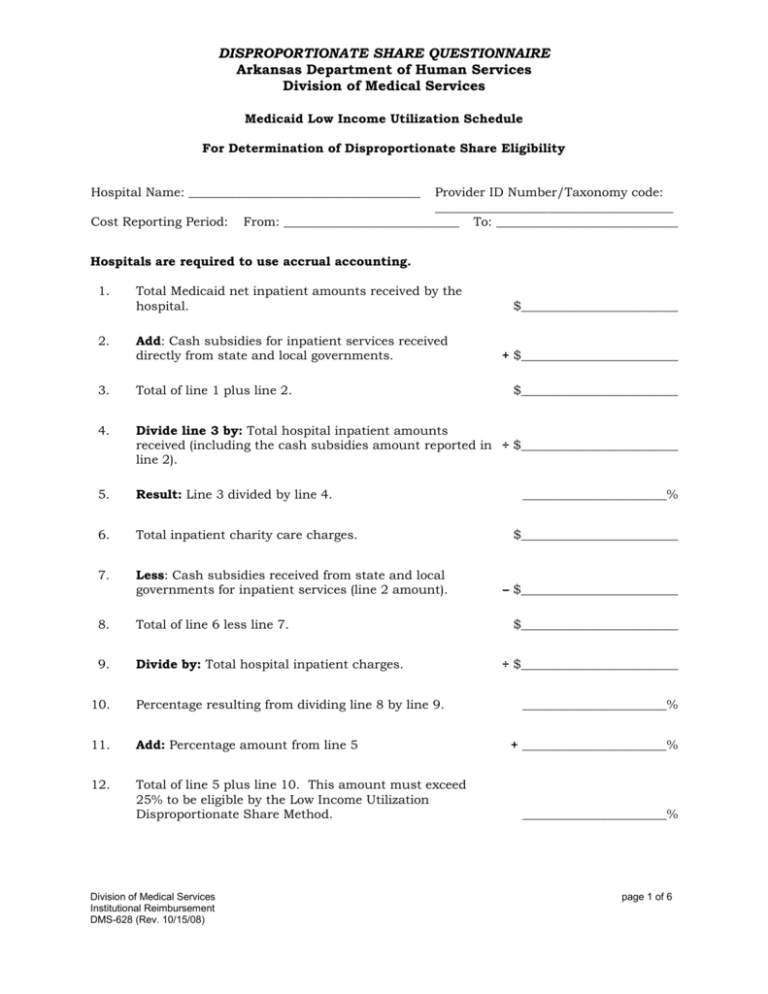
DISPROPORTIONATE SHARE QUESTIONNAIRE Arkansas Department of Human Services Division of Medical Services Medicaid Low Income Utilization Schedule For Determination of Disproportionate Share Eligibility Hospital Name: _____________________________________ Cost Reporting Period: Provider ID Number/Taxonomy code: ______________________________________ From: ____________________________ To: _____________________________ Hospitals are required to use accrual accounting. 1. 2. Total Medicaid net inpatient amounts received by the hospital. Add: Cash subsidies for inpatient services received directly from state and local governments. $_________________________ + $_________________________ 3. Total of line 1 plus line 2. 4. Divide line 3 by: Total hospital inpatient amounts received (including the cash subsidies amount reported in ÷ $_________________________ line 2). 5. Result: Line 3 divided by line 4. 6. Total inpatient charity care charges. 7. Less: Cash subsidies received from state and local governments for inpatient services (line 2 amount). 8. Total of line 6 less line 7. 9. Divide by: Total hospital inpatient charges. 10. Percentage resulting from dividing line 8 by line 9. 11. Add: Percentage amount from line 5 12. Total of line 5 plus line 10. This amount must exceed 25% to be eligible by the Low Income Utilization Disproportionate Share Method. Division of Medical Services Institutional Reimbursement DMS-628 (Rev. 10/15/08) $_________________________ _______________________% $_________________________ – $_________________________ $_________________________ ÷ $_________________________ _______________________% + _______________________% _______________________% page 1 of 6 DISPROPORTIONATE SHARE QUESTIONNAIRE Arkansas Department of Human Services Division of Medical Services Instructions for Medicaid Low Income Utilization Schedule Hospital Name: _____________________________________ Cost Reporting Period: Provider ID Number/Taxonomy code: ______________________________________ From: ____________________________ To: _____________________________ Hospitals are required to use accrual accounting. 1. Total Medicaid net inpatient amounts received by the hospital. 2. Add: Total amount of cash subsidies reasonably attributable to inpatient hospital services (monetary assistance) received from state and local governments. 3. Total of line 1 plus line 2. 4. Divide line 3 by the total amount received for inpatient services from all sources, including the cash subsidies amount reported in line 2. 5. Divide: line 3 by line 4 (expressed as a percentage, to two decimal places, example 17.20%). 6. Enter the total amount of the hospital’s charges for inpatient hospital services attributed to charity care (care provided to individuals who have no source of payment, third party or personal resources), which amount shall not include contractual allowances and discounts for the cost reporting period. 7. Enter the total from line 2 and subtract it from line 6. 8. Total of line 6 minus line 7. 9. Divide line 8 by the total of inpatient hospital charges in the period. 10. Result of line 8 divided by line 9, expressed as a percentage to two decimal places (example 17.20%). 11. Enter the percentage from line 5 and add it to the percentage in line 10. 12. Express the sum of line 5 and line 10 as a percentage to two decimal places (example 34.40%). This sum must exceed 25% to be eligible by the Low Income Utilization Disproportionate Share Method. This questionnaire and instructions are based on the Arkansas State Plan under Title XIX of the Social Security Act (Attachment 4.19-A), as described in Subsections 250.300 through 250.500 of the Arkansas Medicaid Hospital / End-Stage Renal Disease Provider Manual. Division of Medical Services Institutional Reimbursement DMS-628 (Rev. 10/15/08) page 2 of 6 DISPROPORTIONATE SHARE QUESTIONNAIRE Arkansas Department of Human Services Division of Medical Services Obstetrical Information for Determination of Disproportionate Share Eligibility Hospital Name: _____________________________________ Cost Reporting Period: Provider ID Number/Taxonomy code: ______________________________________ From: ____________________________ To: _____________________________ 1. List all physicians with staff privileges who agreed to provide non-emergency obstetric services to Medicaid recipients during the cost reporting period. Physician From To ____________________________________________ ___________________ ____________________ ____________________________________________ ___________________ ____________________ ____________________________________________ ___________________ ____________________ ____________________________________________ ___________________ ____________________ ____________________________________________ ___________________ ____________________ ____________________________________________ ___________________ ____________________ 2. Were the hospital’s inpatients predominately (at least 50%) individuals under 18 years of age during the cost reporting period? Yes________________ No________________ 3. Did the hospital offer non-emergency obstetric services as of December 21, 1987? Yes________________ Division of Medical Services Institutional Reimbursement DMS-628 (Rev. 10/15/08) No________________ page 3 of 6 DISPROPORTIONATE SHARE QUESTIONNAIRE Arkansas Department of Human Services Division of Medical Services Determination of the Disproportionate Share Hospital Limit Hospital Name: _____________________________________ Cost Reporting Period: 1. 2. Provider ID Number/Taxonomy code: ______________________________________ From: ____________________________ To: _____________________________ Total cost of Medicaid inpatient and outpatient covered services. Less: Total Medicaid inpatient and outpatient reimbursement. Do not include any disproportionate share reimbursement $_____________________ – $_____________________ 3. Total of line 1 less line 2. $_____________________ 4. Total cost of inpatient and outpatient services to charity care patients. $_____________________ 5. Less: Total of payments made, plus estimated future payments to be made, by charity care patients. 6. Total of line 4 less line 5. 7. Plus: line 3. 8. Total of line 3 plus line 6 = Disproportionate Share Hospital Limit Division of Medical Services Institutional Reimbursement DMS-628 (Rev. 10/15/08) – $_____________________ $_____________________ + $_____________________ $_____________________ page 4 of 6 DISPROPORTIONATE SHARE QUESTIONNAIRE Arkansas Department of Human Services Division of Medical Services Medicaid Eligible Patient Days Hospital Name: _____________________________________ Cost Reporting Period: A. Arkansas Medicaid-Eligible Patient Days 1) Total Medicaid Paid Days (Per Cost Report): 2) Total Medicaid-Eligible Unpaid Days: B. C. Provider ID Number/Taxonomy code: ______________________________________ From: ____________________________ To: _____________________________ Other States’ Medicaid-Eligible Patient Days 3) Total Medicaid Paid Days: 4) Total Medicaid-Eligible Unpaid Days: Total Medicaid Eligible Days: Identify in lines 1) and 3) actual Medicaid paid days. Identify in lines 2) and 4) days not paid by Medicaid for Medicaid-eligible patients. The date of discharge is neither a covered day nor a Medicaid-eligible unpaid day. Example #1 – In Arkansas, if a Medicaid-eligible patient is admitted to a hospital on June 1st and discharged June 10th, but the PRO authorizes only a 7-day stay, Medicaid reimburses the hospital for seven (7) days only. Per the calculation above, the seven (7) days would be included in line 1) and two (2) days would be included in line 2). Example #2 – Arkansas Medicaid-eligible clients aged 21 and above have an annual benefit limit of 24 paid inpatient days. A 30-year-old Medicaid-eligible patient is admitted as an inpatient on June 1st and is discharged June 30th. Medicaid will reimburse the hospital for 24 days if the PRO approves a stay of that length and the patient has not had any paid inpatient days in that same state fiscal year (dates of service July 1 through June 30). Per the calculations above, 24 days would be reported in line 1) and 5 days would be reported in line 2). Reference to Acute Psychiatric Hospitals only: Medicaid patients between 21 and 65 years of age are not eligible for Medical Assistance for days in which they are inpatients of an Institution for Mental Disease (IMDs), and their inpatient days in such institutions may not be counted as Medicaid days in computing the Medicaid utilization rate. Inpatient days for these Medicaid patients between 21 and 65 years of age in an IMD are not to be included in lines 1), 2), 3), or 4) above. Division of Medical Services Institutional Reimbursement DMS-628 (Rev. 10/15/08) page 5 of 6 DISPROPORTIONATE SHARE QUESTIONNAIRE Arkansas Department of Human Services Division of Medical Services Hospital Name: _____________________________________ Cost Reporting Period: Provider ID Number/Taxonomy code: ______________________________________ From: ____________________________ To: _____________________________ This questionnaire must be completed, signed and dated, and submitted with the provider’s annual cost report for the provider to be considered for eligibility as a Disproportionate Share Hospital. Out-of-state hospitals must attach to this questionnaire and certification copies of your Provider Statistical and Reimbursement Report (PS&RR) paid days summary worksheets for the cost reporting period that is being reported. Submit a copy of the PS&RR paiddays summary worksheet for each state from which you received Medicaid reimbursement. To calculate disproportionate share eligibility and payment adjustments, Arkansas Medicaid must have your total Medicaid-eligible paid and unpaid patient days from each state (see page 5 of 6). The annual disproportionate share payment adjustment to each disproportionate share hospital shall not exceed the limit for that hospital. If the total of all disproportionate share payment amounts for all disproportionate share hospitals (in-state and bordering city acute care, inpatient psychiatric and rehabilitative hospitals) exceeds, in any given year, $2,745,367 (which amount does not include additional disproportionate share payments to Arkansas State Operated Teaching Hospitals and Arkansas State Operated Psychiatric Hospitals), the disproportionate share payments will be reduced proportionately among disproportionate share hospitals. CERTIFICATION I hereby certify that to the best of my knowledge and belief, the information herein and attachments hereto constitute true, correct, and complete statements prepared from the books and records of the enrolled hospital provider. ___________________________________________ Signature of Authorized Provider Officer ___________________________________________ Title ___________________________________________ Signature Date Division of Medical Services Institutional Reimbursement DMS-628 (Rev. 10/15/08) page 6 of 6