antibody-mediated rejection (PPTX / 11626.55 KB)
advertisement
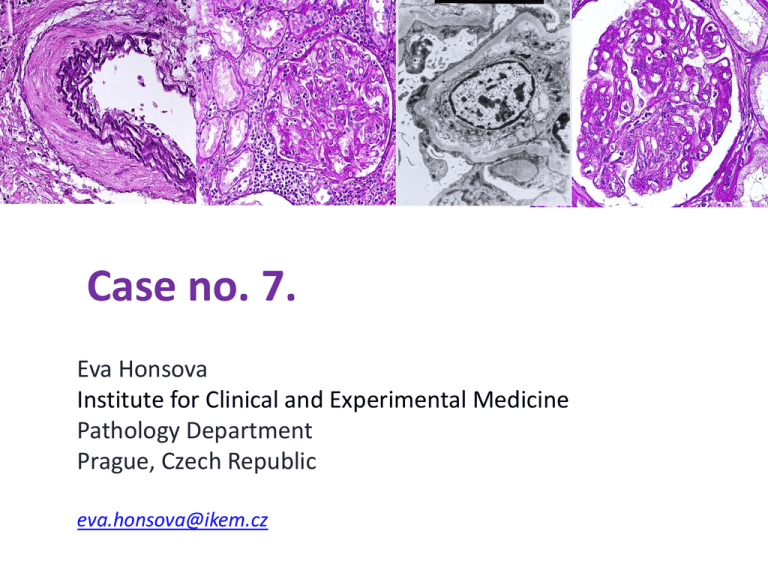
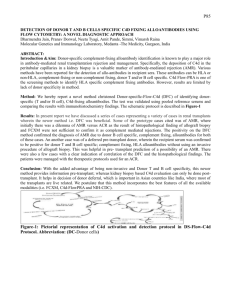
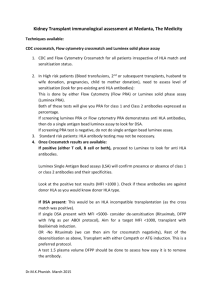
Case no. 7. Eva Honsova Institute for Clinical and Experimental Medicine Pathology Department Prague, Czech Republic eva.honsova@ikem.cz Clinical history • A 55 y/o woman was admitted to our transplant centre to be considered for the second renal transplant • She had agenesis of the left kidney and several stenotic segments in the right ureter: repeated pyelonephritides • Partial resection of the right kidney: when she was 15 year old • Haemodialysis started when she was 35 y/o. • A year later she received a cadaveric kidney and that graft functioned for 18 years. Clinical history • Graftectomia. • After one year on dialysis she received the 2nd cadaveric kidney transplant (AB0 compatible) • The donor: 61y/o woman who died of cerebral edema due to pulmonary embolism. • No induction therapy (0% PRA) and the recipient received standard triple IS protocol therapy (prednisone, tacrolimus, MMF). • Delayed graft function, and a renal biopsy was performed on POD6. Biopsy sample: 6th day C4d staining negative (IF) Dg.: Acute T cell rejection, grade IIA, acute tubular injury Clinical course • Treatment: solumedrol. • Her renal function slowly improved and the S-Cr stabilized on 170μmol/l (1.9mg/dl). • She developed pollen allergy with asthmatic problems • High level of Tacrolimus was identified (tac 17.2 ng/ml), 8ng/ml • She felt well and came to the our centre 3 months later for a graft biopsy according to the protocol • (S-Cr was between 130-160μmol/l) 2nd biopsy sample (under protocol, 3 months) C4d staining negative (IF) Dg.: Acute T-cell-mediated rejection, grade IIB, interstitial inflammation as a part of rejection, glomerulitis No TMA, mild arteriolar lesions Clinical course • She was treated with thymoglobulin and S-Cr improved and descended on the level of 110μmol/l. • She remained well but her renal dysfunction slowly progressed • A new graft biopsy for graft dysfunction (S-Cr 160200μmol/l) was performed 2 years later. 3rd biopsy sample (for dysfunction, 2 years post transplant) C4d staining negative (IF and IH) Dg.: Morphological features of C4d negative humoral rejection Repeated cross match and Luminex were negative. Clinical course • Progressive anemia with reticulocytopenia • Infection by parvovirus B19 was diagnosed (consistent sternal bone marrow smear, virus DNA and IgM antibodies in serum). • Therapy: ivIgs, IS continued • 2 years later: a liver mass (4cm) which was considered FNH. Normal architecture of the liver tissue. 4th biopsy sample (for dysfunction, 5 years postTx, S-Cr 300μmol/l; 3.39mg/dl; PU 4g/day) C4d staining negative (IF and IH) 4th biopsy sample (for dysfunction, 5 years postTx, S-Cr 300μmol/l; 3.39mg/dl; PU 4g/day) Ptc, BM multilayering Repeated cross match and luminex were negative Summary • 1. 2. 3. 4. 4 graft biopsies (all C4d negative): V1, acute tubular injury V2, interstitial inflammation, glomerulitis Transplant glomerulopathy Transplant glomerulopathy, multilayering of ptc-BM, IF/TA • Clinical course: delayed function, slowly progressive dysfunction with proteinuria • Pretransplant cross match negative, 0% PRA • Last 2 biopsies with negative cross match, negative detection of anti HLA antibodies (luminex), negative MICA. Acute/active antibody-mediated rejection Triad of tx glomerulopathy, C4d+, anti-DSA: dg. criteria of chronic active or persistent AMR. Both could be present at variable time points. Abs and C4d are not stable, can increase and vanish. At any given time, these factors may or may not be demonstrable, even if AMR is present. AHR has occurred with all IS regiments. The pathology of AHR has a wide spectrum of findings. However, none of these features is specific. Transplant glomerulopathy (cg) The problem is that when morphological features (as tx glomerulopathy) once set-in, there is not any further known treatment option to reverse CR. Only early dg. of AMR can be beneficial. Acute vascular rejection (v1, v2) and DSA Analysis of 2079 recipients with 302 biopsy proven rejections. They tested all the patients for DSA in the stored sera. 71% of cases with vascular rejection (v1, v2) were associated with DSA. Lancet; 2013(381):313-319. More importantly, 45% v1 or v2 with DSA were C4d negative and classified as T-cell mediated rejection Luminex HLA antigens patients 1. Donor (1989) HLA incompability 2.Donor (2008) HLA incompability A3, A24 A2 A2 A31, A33 A31, A33 B13, B61 B13, B51 B51 B7, B40 (B60,61) B7, B60 DR7, DR11 DR7 no DR4,DR7 DR4 anti MICA anti HLA HLA class I HLA class II 1. Biopsy (IIA, v1) + (B60) 0 0 2. Biopsy (IIB, v2) n/d no serum n/d n/d 3. Biopsy cg 0 0 0 4. Biopsy cg, IF/TA 0 0 0 N. Angaswamy et al. / Human Immunology xxx (2013) xxx–xxx • We do not know whether only low level of anti DSA (HLA class I) were the antibodies which really cause graft injury in this case. • Recent evidence has demonstrated an important role of Th17 response against self-Ags as a mechanism leading to CR • Perclan, collagen IV and VI, agrin • The key point is inflammation • Exposure of cryptic self Ags or their determinants can lead to activation of both: cell- and Absmediated immune responses. • ??? Continuous detection of Abs Conclusion • AMR may occur in the absence of peritubular capillary C4d staining and may be difficult to identify. • Correlation with DSA is helpful. • However, both C4d staining and DSAb titers are not stable and can increase and vanish. • Therefore at any given time these factors may and may not be demonstrable, even if AMR is or has been present. • All v1 and v2 lesions may be indicative for AMR and CMR • In this case, different management focused on the treatment of AMR early after Tx would have been beneficial. Pathology - A gate to the future Future pre-congress meeting of ESP Nephropathology Working Group???