Pathophysiology, Treatment & Prevention of Antibody - wi
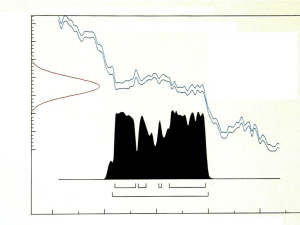
advertisement

Antibody-Mediated Rejection: Prevention, Pathophysiology,Treatment, Brenda Muth, RN, MS, ACNP Transplant Nephrology and Desensitization Objectives Define rejection Acute vs Chronic Clinical vs subclinical rejection AMR, ACR, mixed Discuss prevention of AMR Review immunologic components involved in AMR Review diagnosis of acute AMR Examine treatment options Current therapies Novel treatment including off-label use UW protocols for AMR treatment Definitions AMR Graft rejection caused by Ab directed against HLA molecules, ABO antigens or endothelial cell antigens Clinical Rejection Biopsy confirmed with associated graft dysfunction Subclinical Rejection Histological changes specific for acute rejection on protocol biopsy w/o graft dysfunction Definitions • Hyperacute Rejection – Due to preformed Ab • Early AMR – Due to amnestic Ab response • Late AMR – Due to de novo DSA production • Chronic AMR – Recall secondary DSA response • Mixed rejection • Accomodation – Resistance to injury in presence of Ab Lymphocytes Myeloid Stem cell Lymphoid Stem Cell SC Lymphoblast T PC B NK CD 20 The sequence of letters & numbers identify which HLA gene it is & it’s location HLA-DQB3*0101 (DR52) Gene Specific HLA protein Allele (alternate form of the same gene) Pathophysiology of AMR Donor Organ Capillary Endothelial cell C1 complex 4 Damaged Cell Releases platelet aggregation factors, cytokines Formation of Antigen-Ab complex C4 C4b C4d Endothelial cell necrosis C4d is by-product and marker of complement activation Schwartz, NEJM 2010 Prognosis of AMR • Vasculopathy • Fibrosis • Loss of graft function/graft loss Diagnostic Criteria for Kidney AMR Must have at least 2 of the following • Presence of anti-donor antibodies • C4d staining – C4d1: – C4d2: – C4d3: Minimal C4d stain/detection: 1<10% Focal C4d stain/positive: 10–50% Diffuse C4d stain/positive: >50% • Morphologic evidence of tissue injury – Capillary and or glomerular inflammation (ptc/g >0) and/or thromboses • Graft dysfunction Diagnostic criteria for Pancreas AMR • Acute AMR: (all 3 criteria) – Circulating DSA – morphologic evidence of microvascular tissue injury – C4d staining of interacinar capillaries • Suspicious for AMR – 2 of 3 criteria Drachenberg et all, AJT 2011(9) Consensus Statement for Heart AMR • Based on pathology: – Histology • • • • • Endothelial activation Intravascular macrophages Neutrophilic infiltrates Capillary destruction Interstitial edema, hemorrhage – Immunopathology • May include DSA, graft dysfunction Kobashigawa et al, Journal of Heart and Lung Tx, 2011 (3). Diagnostic Criteria for Liver AMR • Lack of clear criteria for diagnosis. • May include: – Positive C4d staining of sinusoidal endothelium – Proliferation of small bile ducts – Sinusoidal accumulation of neutrophils – cholestasis Kozlowski, et al, Liver Transplantation, 2011 Diagnostic Criteria for Lung AMR • Difficult to diagnose • May be determined by prominence of B cells and plasma cells in inflammatory infiltrate, endothelialitis and small airway inflammation Takemoto et al, AJT, 2004 Antibody mediated rejection Peritubular capillaritis and focal interstitial hemorrhage Nickeleit, Neph Dial and Transplant 18: 2232-2239, 2003 Peritubular capillary Immunofluorescent Staining for C4d Peritubular capillary Immunohistochemistry staining for C4d. Nickeleit, Neph Dial and Transplant 18: 2232-2239, 2003 CD 20 AMR Treatment T PC AMR Treatment • • • • Suppression of T cell response Elimination of circulating Ab Inhibition of Ab Suppression/Depletion of B cells Suppression of T-cell Response Depletional Antilymphocyte Ab (rATG) • Has multiple anti-T cell Ab specificities, costimulatory pathways, cell adhesion molecules, cell surface molecules expressed on B cells and plasma cells. • Usually used as adjuvant therapy in AMR • Used for severe or steroid resistant ACR • FDA approved for Kidney transplant rejection Steroids • inhibits IL-1,IL-2, IL-6 production, T-cell proliferation, cytokine gene transcription & antigen presentation MPA • Prevents proliferation of T & B-cells • FDA approved for kidney CNI • Both CsA & Tac inhibit T & B-cell activation and proliferation • FDA approved for kidney, liver, heart Singh et al, Transplantation Review, 2009 Samaniego et al, Nature Clinical Practice, 2006 micromedex Elimination of Circulating Ab Plasmapheresis • Fast, effective method of eliminating DSA • Used in combination with other therapies • Adverse effects: – Nonselective removal of proteins, bleeding diatheses, volume contraction, requires replacement fluid (albumin), allergic reactions, bld borne pathogens, need HD access • Dose: – 1-1.5 total plasma volume QD or QOD (3 to 6 treatments), followed by maintenance PP – Decision to stop PP should be based on: • elimination of donor-directed HLA antibody • establishment of good graft function • graft failure • Cost: ~ $2000.00 per treatment Apheresis Guidelines considered a therapeutic option when AMR has been confirmed by Bx and/or + DSA & immunosuppressive treatment has not been effective. Singh et al, Transplantation Review, 2009 Apheresis Guidelines, 2009 Inhibition of Antibody Immune Globulin Highly purified IgG from large pools of human plasma diluted in sterile water +/- glucose, sodium. Non-FDA labeled use • Action: – immunomodulatory effects on T cells, macrophages, cytokine synthesis, B-cell function & regulatory action on complement system – Down regulates antibody/blocks HLA Ab from binding to targets – T & B cell suppression • Adverse effects: – Arthralgias, mylagias, HA, HTN, hypotension, MI, Hypercoagulability, allergic reactions, volume overload, AKI • Dose: – T ½ = 3 weeks – Range 100 mg/kg to 2 gm/kg – ~ $500.00 for 100mg/kg dose Singh et al, Transplantation Review, 2009 Micromedex Suppression/Depletion of B-cells Rituximab Genetically engineered chimeric MoAb w/ mouse fused with human IgG. • Indication: – FDA approved for Non-hodgkin’s Lymphoma, rheumatoid arthritis. Use for AMR is off label. • Action: – binds to the CD20 antigen located on pre-B & mature B lymphocytes: mediates B cell lysis – Depletes CD19 & CD20 (Chemical splenectomy) – No effect on plasma cells • Adverse effects: – Infusion and hypersensitivity reactions, cytopenias, fever, infection risk including association with BK • Dose – 375 mg/m2 BSA IV – Duration of treatment ? – ~ $650.00 Singh et al, Transplantation Review, 2009 Micromedex Depletion of Plasma cell Bortezomib Reversible proteasome inhibitor • Indication: FDA approved for multiple myeloma. Use for AMR is off label. • Dose: 1.3 to 1.5 mg/m2 IV day 1, 4, 8, 11. • Adverse effects: – Neuropathy, plt, WBC, GI symptoms • Cost ~$2000 per injection UW experience: used in kidney, liver and pancreas AMR Steroids + PP + IVIG + Bortezomib +/- ATG Everly et al, Transplantation, 2008 Djamali et al, Clinical Transplants, 2009 Sollinger et al, WTC Abstract 2010 Complement Inhibition Eculizumb • Recombinant humanized monoclonal IgG antibody produced from murine myeloma cells that inhibits the cleavage of C5 • Indication: PNH, atypical HUS • Blocks graft injury in presence of DSA, may suppress plasma cells. • Adverse effects: – Risk of neisseiria meningitis, need immunization • Mayo monitored DSA, B & T flow CM, protocol Bx. • Dose: – 600 mg IV injection qw to q2w – Duration of therapy unknown – Cost $5000 for 300 mg vial Monitoring during treatment • Graft function • Infection – Viral, bacterial, fungal • Bone marrow suppression – Leukopenia, thrombocytopenia, anemia • DSA • Immunosuppression • Repeat biopsy Prevention • Identify who is at risk – Sensitized • Current PRA > 20%, Peak PRA > 50% • Black race, Female, retransplant – + crossmatch – Certain disease states (SLE, PSC) • Caution with minimizing immunosuppression • Monitor – DSAs, Biopsy, organ function UW Kidney Transplant Rejection Protocols Suspicious Dex 50 mg IV + taper IA, IB Dex 100 mg IV + taper IIA, IIB, III Dex 100 + taper + ATG C4d< 50% +/Banff I Early: (<3m) Dex 50mg + taper + TPE 3 to 5 treatments + IVIG 100 mg/kg after each TPE Late: (> 3m) Dex 50 mg + taper + IVIG 100 mg/kg weekly x 4wks C4d> 50% +/Banff I Early: Dex 100 mg + taper + TPE 3 to 5 treatments + IVIG 100mg/kg Late: Dex 100 mg + taper + IVIG 100mg/kg x 4wks C4d < 50% + Banff II or III Dex 100mg/kg + taper + TPE 3 to 5 treatments + IVIG 100mg/kg + either ATG or Bortezomib Conclusion • AMR can occur at any time • Biopsy confirmed diagosis • Due to preformed Ab, memory response or de novo Ab production • Causes vascular injury & fibrosis to long term graft survival • Can be recalcitrant to treatment risk for infectious complications after treatment Thank you!