INTRODUCTION - Hampshire Hospitals NHS Foundation Trust
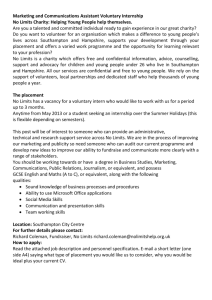
advertisement

Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 1 of 144 BASINGSTOKE AND NORTH HAMPSHIRE HOSPITAL PATHOLOGY USER HANDBOOK Author : Pathology Collaboration : Co-ordinator: David Beacher Authorised By : Dr. N. HUTCHINSON (Clinical Director) Date of Next Revision : June 2012 DO NOT USE AFTER : July 2012 This document replaces revision 6 issued December 2010 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 2 of 144 PREFACE ..................................................................................... 3 INTRODUCTION .......................................................................... 4 PATHOLOGY MANAGEMENT ..................................................... 5 General Pathology .............................................................................................. 5 Blood Sciences ................................................................................................... 5 Histopathology .................................................................................................... 6 Medical Microbiology and Control of Infection .................................................... 6 Hours of Business ............................................................................................... 7 Pathology Supplies ................................................................................................. 8 Electronic Requesting Through ICE ordercomms .................................................. 8 Request cards ........................................................................................................ 8 Blood collection .................................................................................................... 11 Important things to remember when taking blood ............................................. 11 Labelling of specimens/sample ......................................................................... 13 Date and time of samples ................................................................................. 13 High Risk specimens......................................................................................... 14 Specimen Transport ............................................................................................. 14 Transport to the laboratory within the Hospital (Trust Staff) .............................. 14 Transport of specimens from clinics and surgeries ........................................... 15 Research and Development ................................................................................. 15 Screening Programmes and other non-NHS work................................................ 15 Availability of Results ............................................................................................ 16 Turnaround Times ................................................................................................ 16 Reports ................................................................................................................. 16 Out-of-hours service ............................................................................................. 17 DEPARTMENTAL SPECIFIC INFORMATION.............................20 CHEMICAL PATHOLOGY ..........................................................20 Andrology .......................................................................................................... 26 HAEMATOLOGY AND BLOOD TRANSFUSION ........................28 Anticoagulant Services...................................................................................... 38 HISTOPATHOLOGY ...................................................................40 MORTUARY ................................................................................43 MEDICAL MICROBIOLOGY .......................................................48 How to get to Basingstoke & North Hampshire Hospital ........62 Site Map ......................................................................................64 TEST INDEX ...............................................................................65 BACTERIOLOGY .............................................................................................. 65 CHEMICAL PATHOLOGY ................................................................................ 71 HAEMATOLOGY ............................................................................................ 135 SEROLOGY .................................................................................................... 140 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 3 of 144 PREFACE This guide has been prepared to inform the users of Basingstoke & North Hampshire Hospital Pathology Laboratories of which services are available and how to obtain the services required. It is appreciated that with the ever increasing range of tests available it is difficult for the user to know which request form, specimen container, type of specimen and particular protocol is needed to obtain the specific investigation and result they require. Hopefully, this guide will address these difficulties. In addition to this type of information, the guide also contains lists of relevant telephone numbers to facilitate easy access to appropriate Consultants and other senior staff for advice as well as departmental numbers for result enquiries. Any laboratory is, to a large extent, only as good as the user allows it to be. It is important that all request forms and specimen containers are labelled properly with the relevant demographic and clinical details. Care must also be taken to follow any necessary protocol where a result could otherwise be adversely affected. If any doubt exists, it is advisable to contact the appropriate Consultant or department who will be pleased to provide the necessary information. Finally, any views that users may have about how this guide could be improved would be welcomed for incorporation into future editions. Please give these, preferably in writing to David Beacher, Quality Manager (mailto:David.Beacher@BNHFT.NHS.UK). Dr Nicki Hutchinson on behalf of the Pathology Directorate Seventh edition June 2011 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 4 of 144 INTRODUCTION The pathology directorate offers services in five Consultant led divisions, namely chemical pathology, haematology with transfusion, histopathology with mortuary facilities, specialist haemophilia and medical microbiology with infection control. The laboratories are located on the ground floor (Level B) of the theatre block in the main hospital with further facilities downstairs on A floor (mainly microbiology and mortuary). Clinical haemophilia services are based in a separate unit near Parklands. The directorate is an open-access service. Each department has to cope with a high workload and has to organise itself to provide urgent and emergency services as well as ensuring that all results reach the wards or GP surgeries with the minimum of delay. Because the type of work carried out varies considerably, some being labour intensive while some is automated, there are organisational differences from department to department. For example, there are different request cards for some departments and/or tests. If the appropriate request card is used and all the information required given, it enables the laboratory to provide an efficient service. Finally, remember you are always welcome to visit the laboratory and if the staff can put a face to a name, this can only help to improve communication and the service for your patients. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 5 of 144 PATHOLOGY MANAGEMENT General Pathology For general enquiries, complaints, comments, or to discuss service requirements/contracts. Pathology Clinical Director, Dr. Nicki Hutchinson Pathology General Manager, Katie Bolam Pathology Quality Manager, David Beacher Pathology office for general enquiries and results Pathology administrator Mr Alex Kelly, computer manager Mr Shaun Goldsmith for ICE order comms issues: Pathology department fax (in office) ext 3310 ext 2788 ext 3280 ext 4751 ext 3278 ext 3288 07770967360 01256 314905 Blood Sciences Includes Pathology specimen reception, Phlebotomy services, Haematology and Chemical Pathology laboratories and Transfusion services. Mr Ian Savill, Blood Sciences laboratory manager ext 3283 Chemical Pathology For consultant or technical advice including clinical advice and interpretation. Dr. Martyn Knapp, Consultant Clinical Biochemist Mr Robert Jupp, Consultant Clinical Biochemist Secretary Mrs Catherine Wands, Lead BMS in Chemical Pathology Miss Sarah Lewendon, Point of Care co-ordinator Urgent requests or sweat tests (normal hours) Andrology (semen analysis) GTT appointments ext 3270 or 3285 ext 3270 or 3285 ext 3278 ext 3284 ext 3288 ext 3284 ext 3324 ext 4751 Consultant advice is available 24 hours a day from the on-call Biochemist (contacted by the hospital switchboard). Haematology and Blood Transfusion For clinical or technical enquiries, requests for urgent work, to arrange special tests, or anticoagulant services including clinical advice and interpretation. Medical staff Dr Alison Milne, Consultant Haematologist Mrs Helen Todd, secretary Dr Sylwia Simpson, Consultant Haematologist Dr. Katharine Lowndes, Consultant Haematologist Dr Ashok Roy, Associate Specialist ext 3297 ext 3282 ext 3296 ext 3282 ext 3200 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 6 of 144 Mrs Gill Knight, secretary ext 3279 Consultant clinical advice and interpretation is available 24 hours a day from the oncall Haematologist (contacted by bleep via the Hospital switchboard). Other Haematology and Blood Transfusion staff Mr Stephen Knight, Lead BMS in Haematology Mr Roger Chant, Transfusion Specialist Practitioner ext 3294 ext 4756 Dr Jane Needham, Principal BMS Haematology/Coagulation laboratory Transfusion laboratory Urgent requests - Haematology/Coagulation - Blood Transfusion Sister Vicki Warburton, Anticoagulant Nurse Practitioner Sister Jackie Schuster, Anticoagulant Nurse Practitioner Sister Niamh MacIndoe, Anticoagulant Nurse Practitioner ext 3293 ext 3294 ext 3290 ext 3292 ext 3290 ext 3295 ext 3295 ext 3295 Phlebotomy Mrs Jenny Dykes, Phlebotomy services and training ext 3961 Histopathology For clinical advice and interpretation, technical advice, histology reports or to arrange urgent investigations Dr Hanan El-Mahallawi, Consultant Histopathologist Dr Ian Ilesley Consultant Histopathologist Dr Asmat Mustajab, Consultant Histopathologist Consultant’s secretaries Miss Alison Taylor, Department Manager Laboratory enquiries Mr William Chapman, Mortuary Manager Histopathology fax ext 3298 ext 3302 ext 3301 ext 3271, ext 3533, ext 3640 ext 3280 ext 3300 ext 4749 01256 313273 NOTE – Please give four days notice of slide requests for MDT or other meetings Medical Microbiology and Control of Infection For consultant or technical advice, microbiology results, to arrange urgent investigations or for control of infection matters including clinical advice and interpretation. Dr Nicki Hutchinson, Consultant Medical Microbiologist (bleep 2305) ext 3310 Dr Fatima El Bakri, Consultant Medical Microbiologist ext 3305 Dr Jorge Cepeda, Consultant Medical Microbiologist ext 3308 (Consultant on call available through switchboard out of hours) Mr Dave Thomas, Laboratory Manager ext 3311 Laboratory enquiries ext 4904 Infection Control (bleep2356) or contact senior infection control nurses:Hazel Gray, Mobile: 07500990914 or Linda Swanson, Mobile: 0750099012 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 7 of 144 Hours of Business Chemical Pathology – Routine service Mon – Fri 08.00 – 20.00 On call service at all other times including weekends Contact Chemical Pathology bleep 2303 Andrology service 08.30 - 14.00 Monday to Thursday Point of Care Testing. Routine service Mon - Fri 09:00 - 17:30. On-call service at all other times, Point of Care Coordinator contact via switchboard Haematology – Routine service Mon – Fri 08.00 – 20.00 On call service at all other times including weekends Contact Haematology bleep 2304 Phlebotomy Phlebotomy outpatients Mon – Fri 08.00 – 17.00 Phlebotomy service to BNHFT Wards Mon – Fri 07.00 – 11.00 Contact Phlebotomy supervisor for further information on Ext 3291. Limited Saturday service for INPATIENTS ONLY, 07.00 – 11.00 Limited Sunday service for INPATIENTS ONLY, 07.00 – 11.00 (Limited relates to the following: Wessex Ward, E Floor and C Floor) Microbiology – Routine service Mon – Fri 09.00 – 17.30 Saturday 09.00 – 12.00 On call service Mon – Fri 17.30 – 09.00 Saturday 12.00 – Mon 09.00 Contact Microbiology On call Biomedical Scientist: Monday to Sunday 9.00am Telephone: 07721 881673 Sunday 9.00am – Monday 9.00am Telephone: 07887 794673 Cellular Pathology – Routine service 09.00 – 17.15 On call service: An on call service is available at the discretion of the Department Manager and the Consultant Pathologist Please contact the department via switchboard Mortuary – Routine service Mon – Fri 08.00 – 16.00 On call service at all other times including weekends Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 8 of 144 Pathology Supplies At the BNHFT a ward top-up system is operated by supplies. Additional stock may be ordered and collected directly from pathology stores during core hours. Outside BNHFT orders can be made by fax, email or writing. These are dispatched as promptly as possible. However, please allow three working days for delivery. Urgent orders may be dispatched the same day within working hours. Service users are advised not to hoard supplies as stock is date-coded and issued on a rotational basis. For further information please contact Pathology reception. Electronic Requesting Through ICE ordercomms Internal Hospital Test Requests Please follow the instruction detailed in the Trust standard operating procedure TPGEN-ICEREQUEST, located on the Intranet, for requesting all Pathology tests. In the event of system failure please revert to the paper based request card system. GP Test Requests Please follow your local systems operating guide for requesting tests through the ICE system. There are 4 general GP systems covered, these are:- EMIS LV, EMIS PCS, VISION INPS & ISOFT. For EMIS LV, EMIS PCS & VISION Systems the ICE requesting procedure can be located on the GP section of the Trust Website. http://www.northhampshire.nhs.uk/gps-doctors/referral-guidance/-usefulinformation/gp-e-requesting/ If an interruption occurs with ICE then please revert to the paper request form as supplied Request cards The request card is a crucial document. It is usually the only link between the laboratory staff and the ward staff or general practitioner responsible for a patient on whom a test has been requested. For efficient processing, all the information requested must be given in a legible form. Accurate patient identification is obviously of vital importance and wherever possible, please use a computer printed patient label on cards or pots. Most computer labels are not suitable for use on blood tubes as they cause jams in the processing equipment. This is not the case however with those GP practices that print 2-dimensional bar coded patient ID labels when the small labels associated can be used on blood tubes without problems Requests for pathology tests will NOT be accepted unless there are three matching points of identification on both sample and request card. Acceptable data includes Full name, date of birth, NHS number, Hospital number or first line of the address. Incomplete or discrepant requests will be rejected and the requesting doctor informed. Laboratory staff are not authorised to make changes to cards or samples. NOTE there are slightly different and more stringent requirements for Blood Transfusion. Please specify specimen collection time and date on all samples and request cards. Clinical information is essential for validation and interpretation of results and to enable initiation of further investigations where appropriate. If insufficient information Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 9 of 144 is given, the Consultant Pathologists reserve the right to decline to perform the requested test. Request cards must be signed by a doctor or requesting practitioner. Please print your name at the bottom of the request form to ensure that you can be contacted promptly with significant results or problems. And finally, we can always perform tests but it is very difficult to send back reports if you don’t say who the consultant/GP is and where. Therefore the following legible information is required on the request card: Patient's full name - surname and forename (initials are not acceptable) Date of birth and sex of patient NHS number and, if known, hospital number Patient’s address including the postcode Patient’s contact telephone number The requesting clinician and location Relevant clinical information and any drug therapy The tests being requested Type of specimen with the date and time it was collected Indication if HIGH RISK status Additional information may be required for some investigations ie “Special Haematology, Thrombophilia and Ante natal screening”. Please see separate departmental sections. ‘Unknown’ patients e.g. those admitted unconscious, unaccompanied and without documentation, should have their specimens identified with the casualty number. See the Trust Policy for Unconscious Patients. Regrettably, specimens will be discarded if they are inadequately labelled, if the patient’s identification is in doubt, or if they have leaked and/or been contaminated. Request cards for Blood Transfusion and/or blood grouping must have at least three identification points. Essential Patient’s Full name - Surname and forename (initials are not acceptable) Date of birth Plus one of the following NHS number Hospital number or in exceptional circumstances , patient’s address including post code The labelling on the Request Card must match the labelling on the sample! Also required is Collector's signature, date and time of collection and the signature of the requesting doctor Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 10 of 144 EXCEPTIONS A&E shall use a unique patient number for patients who are brought in unconscious or unable to be identified. Follow trust procedure Sexual Health shall use the unique patient number and date of birth due to patient confidentiality. The Bone Bank shall use the Bone bank number and date of birth due to patient confidentiality. Specimen Collection / Sample Requirements It is important to use the correct specimen container and/or tube and take the sample at the appropriate time. If you have any doubts, please contact the department who will be happy to advise. Further information can be found in the departmental specific sections or in the test index at the rear of the handbook. Urgent requests All requests for work to be handled urgently must be made directly to the laboratory concerned by phone as soon as the sample is taken. It is the responsibility of the requesting doctor to take the sample and arrange for a porter to bring it to the laboratory (bleep charge hand porter on 1201). For Urgent samples from the community please discuss these with the relevant laboratory. Phlebotomy service Trained and experienced staff provide a phlebotomy service on the wards from 0700 to 1100 hr Mon-Fri. They have to follow a strict timetable and are instructed ONLY to collect samples which have been requested on to the Phlebotomy Round through the ICE system before 06.30. The phlebotomists do not collect for emergency tests, which must be organised by the requesting doctor. Between 0800hr and 1700hr Mon-Fri a phlebotomy service is provided in the laboratory suite for ambulatory patients, both hospital and GP. Glucose tolerance tests are performed during the morning sessions and can be booked through the pathology office on ext 4751 (external line 01256 314751). Training Phlebotomy training is offered by the laboratory for nursing and phlebotomy staff within the district. A charge for this service is made to cover our costs. Contact Mr Ian Savill ext. 3283. Blood Tube supplies The laboratory supplies phlebotomy materials to wards and GP practices. A topping-up service is provided during the week to wards. GP practices should requisition stocks on the appropriate form. It is important that expiry dates on blood tubes are reviewed regularly and any stock that is close to the expiry date should be Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 11 of 144 returned to the Pathology laboratory where prompt use will prevent wastage. Blood collection Please use only Vacuette system to collect blood samples rather than using a needle and syringe. Artefactual results may be obtained when using a syringe and then decanting the blood into Vacuum tubes, it is much more expensive and less safe. Safety blood collection sets (butterflies) with 30cm tubing combined with a dedicated holder should be used to collect samples for Blood Cultures. Other tubes can be filled after the Blood Cultures using the same collection set, but it is imperative that the Blood Culture bottles are inoculated first. To ensure that requests are dealt with effectively, it is essential to comply with the following guidelines. Specimens should be placed in the appropriate containers which must be securely fastened. The vacuum tube system has many advantages: Mixing of the correct volume of blood and anticoagulant is instantaneous. Wide selection of bottles available with different volumes and anticoagulants. Syringes are not required and the volume of blood needed does not have to be calculated in advance. Closed sampling is safer on the wards and in the laboratory. Adaptors for use with butterflies are available for: 'difficult veins' patients who cannot keep still situations where continued venous access is required Note the preferred order of tube use is ... Citrate samples Plain Gel Samples Heparinised samples EDTA samples EDTA samples Oxalate samples BLUE YELLOW/GOLD GREEN LAVENDER PINK GREY If you are not familiar with the system, or wish to have instruction, our phlebotomists will be happy to help you. Important things to remember when taking blood 1. Those taking blood must have received appropriate training as defined by the National Patient Safety Agency guidelines. 2. Identify patient correctly before taking blood. Ask patient to state their name and date of birth, check their identity bracelet if present. Ensure that all details match the request card. 3. Use the correct blood tube for the test required. Mix the bottle gently after collection to ensure activation of any additive. Do not shake. 4. The sequence of blood vacuum tube collection should be: BLUE, GOLD, GREEN, LAVENDER, PINK, GREY. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 12 of 144 5. Do not remove tops to manually fill bottles. Vacuum tubes are not designed for use in this way and will leak. 6. Gross errors occur when samples have been collected from an area that is receiving an intravenous infusion. Do not take samples from in-dwelling access devices unless specific training has been received. 7. Needles and holders are for single use only and must be disposed of immediately into an adjacent sharps container. Needles must not be resheathed or removed from the holder. 8. Take care to prevent needle stick injuries. If you do have a needle stick injury contact occupational health or the emergency department immediately. 9. Under-filled/over filled coagulation (citrate) bottles will be rejected as results will be unreliable. 10. Ensure complete identification is clearly written on the bottle immediately after taking samples. Do not pre-label tubes. If labels are used on cards ensure that they are on all layers of multi–part cards. 11. High-risk patients. Both samples and cards must be identified with a ‘high risk’ label and each sample should be sealed in a separate plastic bag. High-risk groups can include patients suffering from, or thought to be suffering from, Hepatitis, CJD, HIV, TB, E coli 0157 and other notifiable diseases. Intravenous drug users and patients who have travelled abroad recently and present with unexplained high pyrexia should also be treated as high risk. 12. All blood spillages must be cleaned up immediately. Gloves must be worn and special care taken with any broken plastic/glass. The contaminated area must be decontaminated with ViruSolve+ or a locally agreed disinfectant. 13. Blood cannot be accepted by the laboratory without a request card/electronic request, which must be completed and signed by the requesting practitioner. Black ball point pen and clear printing must be used to ensure legibility. Blood Sciences cards are scanned, print one digit or letter within each entry box. 14. Samples sent to the laboratory must arrive in a leak-proof container. Blood tubes should be placed in the plastic bag attached to the request card. We are unable to guarantee the processing of leaking samples. If not processed, these will be disposed of immediately and the requesting doctor informed. Patients will be contacted directly if the samples were taken by the laboratory. 15. Samples should be delivered to the laboratory as soon as possible after collection. For some tests it is essential that the sample be received and processed within 30 minutes (See Test index). Coagulation assays must be performed within six hours of taking blood. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 13 of 144 16. Requests for urgent tests must be notified directly to the department concerned (see phone numbers on pages 5 - 6). Samples must be collected or organised by the requesting doctor who must also arrange their delivery to the laboratory; within the hospital this can be done by bleeping the chargehand porter on 1201. Pathology phlebotomists will NOT collect urgent samples nor deliver them to the laboratory. 17. It is the responsibility of the requesting doctor to ensure that all these requirements are met. The laboratory cannot accept the responsibility of changing any request card or sample identification. Incomplete request cards and incorrectly labelled samples will be brought to the attention of requesting doctors and discarded where appropriate. Labelling of specimens/sample Specimens must be identifiable. Unlabelled samples will not be processed and it is the requesting clinician’s responsibility to ensure that samples are labelled correctly. The minimum information required on the specimen label is three unique identifiers (see exceptions): Patient’s Full Name - Surname and forename (initials are not acceptable) Date of birth NHS number or, if not available, Hospital number In the absence of the NHS Number or Hospital Number the first line of address may be substituted. Post code only is not acceptable In addition Date, and time if appropriate, of collection ICE ordercomms labels MUST NOT BE USED on Transfusion samples Addressograph labels MUST NOT BE USED on Transfusion samples The container should be sealed in the bag attached to the combined pathology request card. Specimens should be transported to the laboratory as rapidly as possible after collection to ensure that no significant deterioration occurs before processing. EXCEPTIONS Microbiology requires a minimum of two points of ID for non ICE requests on samples rather than three. ICE requests should have minimum of three points of ID as above. A&E shall use a unique patient number for patients who are brought in unconscious or unable to be identified. They must also state sex and approximate age. Sexual Health shall use the unique patient number and date of birth due to patient confidentiality. The Bone Bank shall use the Bone bank number and date of birth due to patient confidentiality. Date and time of samples The date the specimen was taken is essential for the laboratory to asses whether there has been a delay in receipt of the sample. The 24-hour clock time on Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 14 of 144 specimens is preferred. Recording of sample time is especially important for blood glucose, Digoxin and other drug assays, as therapeutic drug monitoring may require dose related timing. Hormone profiles in women may also require the day in the menstrual cycle (if appropriate), for interpretation. High Risk specimens High-risk groups can include patients suffering from, or thought to be suffering from, Hepatitis, HIV, CJD, TB, E coli 0157 and other notifiable diseases. Intra-venous drug users and patients who have had recent foreign travel with unexplained high pyrexia should also be treated as high risk. Request forms and samples MUST be labelled with "Danger of Infection" labels, placed in a Bio-hazard bag and transported to the laboratory with care. To protect all healthcare workers, requests for investigations on high risk samples should be the minimum required for diagnosis and good patient management. Great care must be taken when obtaining specimens and equipment, such as needles and blades, must be immediately disposed of safely into approved sharps boxes. Should a spillage of blood, fluids or tissue occur, this should be made safe and disposed of appropriately. Specimen Transport Transport to the laboratory within the Hospital (Trust Staff) All specimens, in appropriate containers, inside the designated sealed specimen bags must be transported to the laboratory in either a sealed Transport Box or a standard Transport Tray. The tray or box must be clearly labelled with the International BIOHAZARD label and contact details in case of accident. Specimens should be transported to the laboratory as rapidly as possible after collection to ensure that no significant deterioration occurs before processing. It is not acceptable to carry specimens by hand or in a pocket at any time. During working hours all specimens should be delivered to Pathology reception. Portering service Porters regularly collect samples from BNHFT wards during normal working hours Community units: A daily transport run is made to all of these for the collection of specimens. GP surgeries: A daily transport run is made to all surgeries. Patients transporting their own samples are exempt from transport regulations, however packing/labelling instructions must be followed. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 15 of 144 Transport of specimens from clinics and surgeries All pathology specimens must be placed in primary containers and labelled fully with three independent patient identifiers (Full name – Surname and Forename, DOB, and NHS number (see exceptions p13). If the NHS number is not available the Hospital number. In emergencies only the Patient’s first line of address may be utilised. Place the specimen into an approved sealed specimen bag with enough absorbent material to contain the entire sample should a leak occur. Place the request form into the side section of the bag if using ‘Ziplock bags’ (separate from the specimen - avoids contamination if spillage occurs). The patient details including all relevant clinical details must be written clearly onto the request form. Infection risk specimens must have a “Danger of Infection” sticker attached to the specimen(s) and the request form. Specimens should be transported to the laboratory as rapidly as possible after collection to ensure that no significant deterioration occurs before processing. All samples must be transported to the laboratory in a sealed Transport Box. The box must be clearly labelled with the International BIOHAZARD label, UN3373 Biological Substance Category B diamond and contact details in case of accident/incident. If initial risk assessments of a patient indicate possible TSE or Hazard Group 4 organisms i.e. Viral Haemorrhagic Fever the requesting doctor must contact the Consultant Microbiologist for advice before specimens are taken and dispatched. All transport drivers MUST carry ”instructions in writing” in accordance with the Transport of Dangerous Goods Regulations (ADR), Chapter 5 (section 5.4.3.4), within the vehicle while Pathology specimens are on board. NOTE: All van/car drivers must carry spill kits and gloves. (HSE “safe working and the prevention of infection in clinical laboratories and similar facilities” 2003 Appendix 4, section 22) Research and Development It is the Department's policy to encourage appropriate research and development and to promote personal, professional development. Many of the medical and scientific staff take an active part in medical education and research. Screening Programmes and other non-NHS work The Department is involved in health screening programmes and is happy to provide quotations for individually tailored schemes and private work. Please contact the Blood Sciences Manager. The department is also involved in several non-NHS schemes and performs pathology testing that includes: Private hospitals Education courses DVLA Health screening Quality Control Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 16 of 144 Availability of Results The Departments endeavour to process all specimens received in the most timely and accurate way possible. Urgent results may be available within the hour, following prior discussion with the laboratory. Results for routine haematology and biochemistry tests are available via the Pathology computer within 4 – 8 hours. Most tests are performed the same day but some take several days and are performed in batches. Special investigations may be sent to other centres and these results can take two weeks, sometimes longer. Turnaround Times A full table of representative turnaround times is in the Test Index. Turnaround times are routinely monitored as part of the Laboratory’s Continual Quality Improvement Programme. Reports Grossly abnormal results will be telephoned. All pathology results are available on the ward terminals through the ICE result reporting module, and in times of ICE failure through the ward enquiry programme, as soon as they have been authorised for release. Please look here first before phoning the laboratory. Hard copy print outs of Chemical Pathology, Haematology and Microbiology results can be generated from these terminals to minimise risk of transcription errors. Standard format reports are computer generated several times a day and can be viewed through the ICE results reporting system for all GP surgeries that have access. This includes access to Hospital generated results giving GP’s access to full patient histories. Surgeries that are linked to the NHS Net and have EDI links have the results automatically sent to them, EXCEPT Histology/Cytology reports. Hard copies are still sent for Histology/cytology and for other departments if electronic transfer is not possible. The reference/normal or therapeutic ranges are quoted on the report form for most assays. These are current ranges and may supersede other listed ranges. A Clinisys WinPath pathology computer system is in use covering all disciplines including microbiology, histology, haematology, blood transfusion and chemical pathology. Access to the system is available on ward and clinic areas through the hospital network. WinPath supports a unique password for each user. New members of hospital staff requiring access should contact Mr Alex Kelly, computer manager, on ext 3288 for password privileges and training. An individual password is needed by each person removing blood from the blood bank. This will be arranged when attending the blood bank training session. Contact Mr Roger Chant ext. 4756. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 17 of 144 All new house officers are given pathology computer training as part of the induction programme when password access will also be organised Out-of-hours service An 'on-call' service is provided by haematology, microbiology and chemical pathology staff outside routine laboratory hours and at weekends and bank holidays. The investigations provided by the 'on-call' service are limited to those shown below. Using the service Specimens for haematology and chemical pathology should be placed in the red box through the metal grille in pathology reception. Immediately results are available they will be entered on the computer so interrogate your VDU rather than telephoning the BMS. Please be tolerant in cases of delay as yours will not be the only patient requiring the service. All urgent microbiology specimens out of hours must be delivered to pathology reception as above but a doctor should always speak personally to the on-call microbiology BMS about the request. Service offered The work for Chemical Pathology and Haematology should be considered as two categories: Investigations that are required to make immediate clinical decisions about the patient's management. For such requests it is essential to contact the on call biomedical scientist but do not do so until the blood has been taken and the samples collected by the porters. Investigations that are required for less urgent clinical decision making/need to know within a few hours/should be available for next morning. For such requests there is no need to contact the biomedical scientist provided the samples are received in the laboratory before 2400 hrs. The on call staff remain in the department through the evening and weekend and will analyse all samples with tests on the list below whether they have been contacted or not. They also remain on site at night but may be resting so if tests are required after about 2400 hours but before next morning you should contact the relevant BMS on call. Ammonia, CSF and Troponin must always be notified For investigations other than those detailed below you may be asked to contact the appropriate Consultant Pathologist. The requesting doctor may also be asked to do this for listed tests if the request seems unreasonable. Non-urgent biochemistry requests may include other tests, but these will only be analysed: - if available on main analyser - if time permits otherwise samples will be secured and analysed next routine working day. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 18 of 144 Requests for work with no element of clinical urgency must not be made outside normal working hours unless the patient will not be available in routine hours. The following investigations are available as out-of-hours tests: Chemical Pathology Serum Troponin Sodium Creatinine Calcium Bilirubin CPK Paracetamol EDTA WB Ammonia * ** Amylase Potassium Urea Phosphate ALT DIG Salicylate Glucose Chloride* CRP Magnesium AST Lithium Osmolality Potassium Osmolality Urine Sodium CSF Glucose Protein Spectrophotometry ** Chloride available only for paediatrics, or for cases of poisoning. On call BMS will scan out of hours if urgent clinical decision needed but will reserve the right NOT to interpret scan if equivocal until seen by Consultant Biochemist Haematology and Blood Transfusion Haemoglobin White cell count Platelets Haematocrit Cross-match Blood group Issue of Blood Products DCT ESR (specific conditions only) Malarial parasites Sickle test Prothrombin time/INR APTT. Thrombin time Fibrinogen D-Dimer (specific conditions only) Factor assays at request of Consultant haematologist only Issue of appropriate blood products Microbiology CSF Examinations of fluids which are turbid or when meningitis is suspected and immediate treatment needs to be instigated. Microscopy Urgent microscopy of a specimen where it is considered necessary in order to attempt to make an immediate diagnosis of the bacterial cause, e.g. abscesses or septic arthritis. Blood culture Specimens should be collected by the medical staff and Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 19 of 144 placed in the incubator in the main pathology laboratory reception. NOTE: The collection site for Blood cultures MUST be cleaned using an alcohol wipe and allowed to dry immediately prior to specimen collection. The rubber bung on the top of the blood culture bottle MUST also be cleaned using an alcohol wipe prior to inoculation. On weekdays the majority of other specimens can be left overnight and cultured the next day. This does not significantly delay reports or decrease chances of pathogen isolation and enables clinicians to collect specimens before starting antibiotics. Such samples should be stored as follows: Urines Pus and other swabs Stools Sputum and exudates boric acid bottle room temperature out of direct sunlight transport medium room temperature refrigerator refrigerator At weekends and bank holidays a delay of several days can be avoided by inoculating non-urgent specimens. The on-call microbiology BMS will undertake this task but it is reasonable to allow such specimens to accumulate during the day and be dealt with as a batch in the evening. Please make it obvious that such specimens can be dealt with when convenient and differentiate them from any which require an immediate microscopy report and in the latter cases contact the BMS on call. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 20 of 144 DEPARTMENTAL SPECIFIC INFORMATION CHEMICAL PATHOLOGY Outline of service The Department of Chemical Pathology provides a comprehensive clinical advisory and analytical service including: routine biochemistry such as electrolytes and investigation of renal, hepatic, bone and lipid disorders specialised biochemistry including therapeutic drug monitoring and toxicology, endocrinology and paediatric biochemistry emergency investigations, rapidly available by prior arrangement on a 24-hour basis andrology (semen analysis) a limited andrology service, including a post vasectomy service. We participate in national and international external Quality Assurance Schemes encompassing the analytical work of the department. A Consultant Biochemist is available for advice during normal working hours and on a 24 hour basis through the hospital switchboard. General practitioners and clinicians are encouraged to contact the laboratory for advice on appropriate tests, abnormal results, or further investigations whenever required. Hours of Service The department is open routinely from 0800 to 1730 hours Monday to Friday with a limited, extended operation through to 2000 hrs weekdays. All other periods are covered by the on call service. For further details see “Out-of-hours service”. Laboratory Organisation The laboratory is divided into automated and manual sections, offering about one hundred and fifty tests in house, which covers over 99% of requests. We also have access to a network of specialist referral laboratories offering a further range of three hundred or so tests. A clinical justification must be given for all tests, especially in the case of referred tests. If adequate clinical information is not provided, the Consultant may decline to carry out the investigation. The laboratory is extensively equipped with state-of-the-art analysers, enabling a greater range of tests to be performed on a daily basis and making other tests more readily available for the emergency on-call service. A further advantage is that Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 21 of 144 smaller blood samples are required for most investigations. “Profile requesting” in which large groups of tests are performed routinely and uncritically has been clearly shown to be at best unhelpful and at worst to increase morbidity by prompting unnecessary invasive procedures. Tests should be requested individually and for a purpose. Patient preparation Gender, age, diet, time of day, exercise, posture and prolonged venous occlusion are all factors that may influence some investigations. If in doubt, ask. Many drugs can interfere with tests. If in doubt, state which drugs your patient is taking. Further information on factors affecting individual tests may be found in the Test Index. Samples See also 'Phlebotomy' Please give time of sample collection (especially important if urgent or in case of blood glucose, cortisol, dynamic function tests, therapeutic drugs etc.). Please avoid delays in getting the blood samples to the laboratory. Some special samples have to be separated within 10 minutes of collection, as they are unstable. Do not refrigerate unseparated specimens. Blood specimen tubes Please refer to the test index for the full list of sample requirements. In general: 1. Clotted blood is preferred for the majority of biochemistry investigations (gold topped vacuum tube) and is essential for lithium analysis. 2. Fluoride-oxalate blood is needed for glucose or lactate (grey top vacuum tube). Within the hospital, clotted blood is accepted for glucose except for glucose tolerance tests. Outlying sites must use grey top tubes. 3. EDTA blood is needed for HbA1c, ammonia, renin/aldosterone, ACTH and carbon monoxide (lavender top vacuum tube). 4. For most combinations of tests, 4ml of clotted blood (gold top) will suffice. Paediatric samples Special tubes are available for paediatric use. Heparinised blood is acceptable for most tests as it yields more plasma from very small samples than clotted blood. Where applicable, please clearly indicate order of priority among tests when several are requested on samples of small volume (e.g. 1-Na/K; 2-Creatinine; 3-LFT). Blood samples that must be taken in the phlebotomy suite at BNHFT or from in-patients at BNHFT and brought immediately to pathology reception: Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 ACTH Ammonia Carboxy/Met haemoglobin Cryoglobulin G-1-P UT Gut hormones IGF1 Lead/heavy metals PTH (Calcium at the same time) Renin/Aldosterone Tacrolimus, Everolimus, Serolimus Vitamins D Page 22 of 144 Aldosterone/Renin Calcitonin C Peptide Cyclosporin Growth Hormone Hydroxybutyrate Insulin (Glucose at the same time) Methotrexate Porphyrins Retinol binding Protein Tryptase 17 Hydroxyprogesterone Special tests and Dynamic Function Tests The above tests require special collection procedures. There are protocol sheets available from the laboratory for tests, some additional to those above, which may involve special patient preparation and/or the injection of hormones and serial specimen collections. Please contact the laboratory before taking a sample. The list is not exhaustive - if in doubt, ask Thyroid Function Testing For the routine assessment of thyroid function only TSH is performed as the first line test. Free T3 and/or free T4 will only be performed by the laboratory if the TSH concentration is outside the reference range or if specifically requested by the requesting clinician. It is therefore important that the requesting clinician specifically requests free T3 on all patients who are receiving or who have received treatment for thyrotoxicosis. Similarly, free T4 should always be specifically requested on patients with known or possible hypothalamic pituitary disease. Lithium Lithium has a narrow therapeutic range necessitating blood levels between 0.4 – 1.2 mmol/L. The lower end of this range is used for elderly and infirm patients and the upper end for younger patients, particularly those being treated for an episode of mania. It is entirely possible for an elderly patient at the upper limit to experience toxicity. The NICE guidance is that when initiating long-term treatment, clinicians should aim for levels of 0.6 – 0.8 mmol/L, with higher levels possibly being of benefit for patients with predominantly manic symptoms. Antibiotic levels – Gentamicin and Vancomycin Use Chemical Pathology request protocol. Requests out of hours will be referred to the Consultant Microbiologist on call. Fluids Pleural, ascitic or drain fluids should be sent in a white top universal container. Calculi Calculi should be sent in a white top universal container. Please do not use boric acid (red top) containers as the stone fragments may be difficult to locate amongst the boric acid crystals. Faeces Faecal samples should be sent in a plain wide-mouthed lab container. The minimum of a grape-sized sample is required but do not fill the container more than Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 23 of 144 two-thirds full. Urine samples Bottles for 24 hour urine collections are issued by the laboratory together with an instruction sheet relevant to the test requested. The following are best performed on 24-hour collections: Electrolytes Creatinine clearance* Phosphate*** Uric Acid Catecholamines/metabolites** Oxalate*** Cortisol Calcium*** Citrate*** * Ensure 5 ml of clotted blood is collected within the 24 hours of the urine collection. This should be sent to the laboratory attached to the urine container. Outpatients should bring their 24 hour urine sample to the laboratory on the morning of final collection and have blood taken from them before they leave the laboratory. ** Catecholamines/metabolites and 5HIAA should be collected into acetic acid. Special container available from laboratory as is a list of interfering drugs. *** Calcium, Phosphate, Citrate, Oxalate must be collected into hydrochloric acid. Special container available from laboratory, CARE required. Protein/creatinine ratios are a useful screen in place of 24 hour protein output and can give a rapid result in conditions such as pre-eclampsia. Most of these tests can also be performed on spot samples for paediatric patients when the ratio to creatinine will be reported. All other commonly requested urine investigations require random urine samples. A plain 'universal' container is required (white top), not one containing boric acid (red top). Reference Ranges and Turnaround Times Please refer to the test index. These are also available on the ward enquiry computer terminals alongside the results. Sample storage and Time Limit for requesting Additional Tests The laboratory stores blood samples for 48 hours after the final report has been issued. Requests for retrospective testing on blood samples is not recommended but will be considered if the request is made within 36 hours of sample collection. Samples that may be required for further investigations or forensic reasons can be stored for several months but it is important that a specific request is made by the doctor to the laboratory staff to keep such samples. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 24 of 144 Telephoned Results Results falling below the lower limit or above the upper limit given in table below will be telephoned. Analyte Lower action limit Upper action limit Sodium (mmol/L) 125 155 Potassium Glucose (mmol/L) (mmol/L) 2.8 2.5 Urea (mmol/L) Creatinine (umol/L) 6.0 (see below) 25.0 30.0 (OPD/GP or in-patient 1st result) 10.0 if patient less than 16yrs old 400 (OPD/GP or in-patient 1st result) 200 if patient less than 16 yrs old Calcium-corrected (mmol/L) 1.80 3.20 Phosphate (mmol/L) 0.30 Magnesium (mmol/L) 0.40 AST (IU/L) 800 ALT (IU/L) 800 Bilirubin (umol/L) 300 (Paediatric only) CK (IU/L) 3000 Amylase (IU/L) 500 (OPD/GP or in-patient 1st result) Digoxin (ug/L) 3.0 Phenytoin (mg/L) 25 Theophylline (mg/L) 25 Phenobarbitone (mg/L) 70 Carbamazepine (mg/L) 15 Lithium (mmol/L) 1.2 Triglycerides (mmol/L) 20.0 CRP 400 (OPD/GP or in-patient 1st result) (mg/L) Free T3 (pmol/L) Free T4 (pmol/L) Cortisol (When not post dex) (nmol/L) Troponin (ug/L) 30 5 100 0.05 (GP/OPD only) Ammonia (umol/L) 100 (Neonate 0 – 3 days 47 (> 3 days, 1st result) Bile Acids (umol/L) 14.0 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 25 of 144 Useful clinical information - Common causes of spurious results Please ensure that you follow instructions when collecting and storing samples. Inappropriate sample collection, storage and transport can interfere with a number of results. Some examples are given in the table below: Problem Common causes Effect Inappropriate collection Sample taken from drip arm Increased drip analyte site e.g. K , Glucose Dilution effect, low results Incorrect container or anticoagulant No fluoride oxalate Decreased glucose E.D.T.A. contamination Decreased Ca and Alk P Increased K Li sample collected into Li Heparin Incorrect tube fill/mixing Increased Li ALL analytes may be compromised Delay in separation of serum/plasma overnight storage delay in transit Labile analytes Not immediately separated Decreased ACTH, Insulin, and frozen C Peptide and Gastrin Storage Biochemistry samples in a Increased K fridge Haemolysis Expelling blood through a needle into the tube Increased K, PO4, AST, LDH, Iron, Par, CPK, TP, Trig Vigorous shaking Decreased AMY, ALP Extremes of temperature Increased K, PO4, LDH Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 26 of 144 Andrology The Andrology Laboratory is an integral part of the Fertility Service offered within this hospital. Andrology investigations include basic semen analysis and semen assessment following vasectomy. Reference values for semen assessment are defined by the World Health Organization: Manual for the Examination and processing of Human Semen (FIFTH EDITION) 2009 and have been generated from several prospective, crosssectional studies of semen quality and fertility. The attached table provides lower reference values of semen characteristics of recent fathers, whose partner became pregnant within 12 months of stopping use of contraception. Parameter Lower reference mean Semen volume (ml) >1.5 Total sperm number (106 per ejaculate) >39 Sperm concentration (106 per ml) >15 Total motility (PR+ NP, %) >40 Progressive motility (PR, %) >32 Sperm morphology (normal forms, %) >4 pH ≥ 7.2 *MAR test (motile spermatozoa with bound particles, %) <50% reported as < 50 negative >50% positive) **Vitality (live spermatozoa, %) >58 Cooper TG et al. (2009) World Health Organization reference values for human semen characteristics. Human Reproduction Update. High viscosity samples can interfere with sperm motility and concentration *The mixed anti-globulin reaction or MAR test uses IgG- coated latex particles and anti-serum to human IgG. In the presence of spermatozoa with IgG antibodies the spermatozoa adhere to the latex particles. WHO considers that testing for IgG antibodies is adequate, since IgA antibodies almost never occur with out IgG antibodies. Low sperm concentrations and / or reduced sperm motility can give unrepresentative results and will not be reported. **Test only performed if the number of immotile sperm is greater than 50% It is important to note that semen characteristics are highly variable, both within and among men, and are not the sole determinants of a couple’s fertility; the ranges therefore provide only a guide to a man’s fertility status. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 27 of 144 THE SERVICE: The Fertility laboratory has been a CPA enrolled laboratory since 2005 Member of the UK national NEQAS quality control scheme since 1998 Samples are received by appointment only, enabling prompt analysis within a limited time window Early morning appointments are available, offering as little disruption as possible in a friendly, relaxed surroundings The Fertility department is open between 08.30am and 15.00pm Monday to Thursday with a 24hr answering service to pick up messages Client confidentiality and wellbeing is paramount Samples are initially analysed within one hour of receipt and generally reported within 3 working days For further information, specimen requirements and request forms please contact: Denise Riddell MSc FIBMS Senior Biomedical Scientist Andrology Unit Tel: 01256 313352 E- mail: fertility.services@bnhft.nhs.uk Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 28 of 144 HAEMATOLOGY AND BLOOD TRANSFUSION Haematology Section The haematology section provides a clinical diagnostic and therapeutic monitoring service, covering haematology coagulation and anticoagulation services Coagulation services The laboratory provides a comprehensive diagnostic and therapeutic monitoring service for haemostasis and thrombotic disorders and services a designated haemophilia comprehensive care centre. Requests are examined to ensure appropriate tests are performed and additional specialised tests added when indicated. It is therefore essential that appropriate clinical details are provided on the request form to facilitate this. Please do not hesitate to contact the laboratory for scientific or clinical advice. Samples It is essential that the correct specimen container is used with correct volume of blood. This is to ensure the correct blood-to-anticoagulant ratio. The standard Vacuette bottle in use for coagulation tests requires the addition of 3.0 ml blood to give a final volume of 3.5 ml. Please only use Vacuette needles and let the tube fill until it stops naturally. Do not fill with needle and syringe. A special 1.0 ml bottle can be requested and made up in the laboratory for paediatric samples when the larger blood volume cannot be obtained; however, there may be insufficient volume to provide all necessary tests. Please note: tests for haemostasis or thrombosis WILL NOT be performed on under-filled, over-filled, haemolysed, clotted specimens or unlabelled or incorrectly labelled specimens. NB: Phlebotomy tuition and/or practice is available in the laboratory bleeding area by prior appointment. Routine samples should be transported to the laboratory as soon as possible, but within 4 hours at most. Requests for retrospective testing on blood samples is not recommended but will be considered if the request is made within 12 hours of sample collection. Patients for platelet function testing need to be bled in the laboratory. This test is performed by appointment. Samples for investigations of bleeding and thrombotic disorders should ideally be taken in the laboratory to enable rapid freezing and processing of sample as appropriate. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 29 of 144 Blood Transfusion Section Roger Chant Transfusion Specialist Practitioner Dr Sylwia Simpson Lead Consultant For Transfusion Transfusion laboratory Ext Ext Ext 4756 3296 3290 The Blood Transfusion Issue Blood Bank is located on B Floor in the Pathology Department. There is a locked door via the reception area. The code for this door will be found at each ward station. All blood issued for transfusion, Emergency O Rh D Negative Blood, Fresh Frozen Plasma and Cryo Precipitate will be found in this Blood Bank. Platelets need to be stored at room temperature and so will be found on the bench next to the Blood Bank Register. Blood and Blood Component Traceability From November 2005, the EU Directives have made it essential for all Trusts to be able to trace blood and blood component transfusions from vein to vein, ie donor to recipient. In this Trust the requirement is met by use of the Blood Transfusion Report which staff involved MUST complete and sign. Each unit must be checked at the bedside and report signed that the patient has received the unit of blood with the date and time of start and finish. All the essential observations must be documented on this sheet and the bottom copy returned to the Transfusion Department when the transfusion is complete. Failure to complete and record this information makes the Trust liable in criminal law. Please ensure that this confirmation of all blood and blood components transfused is recorded and the bottom sheet returned to the Transfusion Department immediately after the transfusion. Grouping and Crossmatching The laboratory has a fully automated analyser for processing Blood Group and Antibody Screens, on Trust Patients and antenatal requests. Crossmatches for operations are only performed according to the blood order schedule (see “Indications of blood transfusion requests”) otherwise the sample is held for a Group and Save. Deviations from the blood order schedule must be accompanied by a valid reason on the request form. Patients scheduled for major operations should have a group and screen sample taken at the pre-operative assessment clinic for testing, the request for crossmatch may then be taken on admission (usually the day before the operation) unless otherwise stated on the report. Failure to take a group and screen sample at pre-operative assessment may cause a delay in providing compatible blood to cover the operation, if the patient has atypical antibodies. Emergency crossmatches are performed as soon as the sample is received in the laboratory. It is essential to phone the laboratory when an emergency crossmatch is required. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 30 of 144 Emergency O Rh D Negative Blood Two units of emergency O Rh D Negative blood are held in the blood issues fridge in Pathology. When required they should be taken in the cool box provided. They must be returned to the blood bank immediately if they are not used. It is essential to complete the labels on these units of blood and return them to the Blood Transfusion Department if the blood is used, in order to complete the audit trail. The Blood Transfusion department MUST be informed when they are taken so that they can be replaced. The Blood Transfusion Department is served by the National Blood Service Centre at Southampton. There is a daily routine delivery of blood and blood products. The orders have to be placed by 09.30am on the date of delivery. Urgent deliveries will be made at any time by BTS if we run short of blood, however these will be generate an additional charge. If blood is required urgently it can be requested blood by “blue light” and it will be with us within 45 minutes. Orders for platelets should be in the laboratory by 09.30am each day so that the Transfusion Department can plan their workload effectively. For more details on blood transfusion in clinical practice see “Standards in Blood Transfusion Practice”, a copy of this document is held on each ward area. Sample Required for the Transfusion Department Group and Save Crossmatch (incl. Group & save) Ante-Natal Blood Group & antibodies Antibody Screen Direct Coombs Test Kleihauer Cold agglutinin titre Immune Haemolysins Warm auto antibodies (incl. Eluate) Drug related antibodies Donath Landsteiner Antibody titres Anti-D quantitation HLA antibodies Platelet antibodies HLA B27 HLA Typing HLA A,B,Cw HLA DR, DQ HLA B28 6 mL EDTA 6 mL EDTA 6 mL EDTA 6 mL EDTA 6 mL EDTA or 3 ml EDTA 3 mL EDTA 6 mL EDTA (to be kept at 37oC) 6 mL EDTA 6 mL EDTA and 3 x 3ml EDTA 6 mL EDTA 6 mL EDTA and 2 x 3ml EDTA 6 mL EDTA 6 mL EDTA 6 mL EDTA7-10ml clotted 20mL EDTA and 10ml clotted blood 6 mL EDTA 12 mL EDTA 12 mL EDTA 12 mLEDTA 6 mL EDTA Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 31 of 144 Useful clinical information - Common causes of spurious results Please ensure that you follow instructions when collecting and storing samples. Inappropriate sample collection, storage and transport can interfere with a number of results. Some examples are given in the table below: Problem Common causes Inappropriate collection Sample taken from drip site arm Effect Will dilute any antibody present which may be missed on the crossmatch Incorrect tube fill/mixing Failure to adequately mix May result in clots in the sample the sample making it invalid for crossmatching Delay in sending the overnight storage sample to the laboratory delay in transit Haemolysis May reduce some antibody activity, or cause haemolysis making the sample unsuitable for testing Expelling blood through a Haemolysed samples are needle into the tube unsuitable for crossmatching Vigorous shaking Extremes of temperature Incorrect container or anticoagulant Plain bottle, or any bottle Unsuitable for testing other than an EDTA sample Sample taken from wrong patient Bad phlebotomy technique, / patient identification Wrong blood which could lead to clinical incident Tests carried out -Full ABO cell and serum grouping and rapid ABO cell grouping -Full Rh D grouping with two anti D's and rapid spin Rh D grouping -Partial D testing and genotyping when appropriate, but not routinely -Antibody screening by gel column technology -Kleihauer tests -Direct Coombs test, broad spectrum and split fractions -Cross matching -Identification of atypical blood group antibodies. -Antibody titres -Cold agglutinin titres -Donath Landsteiner test Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 32 of 144 -Haemolysin tests -Preparation and examination of eluates -Examination and identification of drug related antibodies -Group A sub typing, i.e. A2, A3, Ax. -Autoabsorption tests for auto immune haemolytic anaemia Turnaround Times 24 hrs Emergency Crossmatch 20 minutes Full Crossmatch 60 minutes Full Crossmatch from a Group and Save 30 minutes The following tests are referred to the National Blood Service at Filton: -Difficult antibody investigations and rare blood group confirmations -Quantitation of Anti-D and Anti-c Allo absorbtion tests fro Auto immune haemolytic anaemia Routine Request Turnaround Times 10 days Urgent Request Turnaround Times 12 hours Sample Reception NHS Blood and Transplant – Filton FAO: Red Cell Immunology 500 North Bristol Park Filton Bristol RB34 7QH The Following Test is sent to the Blood Group Reference Laboratory -Foetal Grouping Turnaround Times 14 days Dr Peter Martin International Blood Group Reference Laboratory 500 North Bristol Park Filton Bristol RB34 7QH The following tests are referred to the Histocompatibility and Immunogenetics Laboratory at the National Blood Service Tooting -White cell and platelet antibodies -HLA B27 - Monday till Thursday -Other Specific HLAs – Monday - Thursday -HLA typing - only by prior arrangement. Turnaround times 21 days Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 33 of 144 Sample Reception National Blood Service - Tooting Centre FAO: Histocompatibility and Immunogenetics Cranmere Terrace Tooting London SW17 0RB Request card and sample requirements All request cards and samples submitted to the Blood Transfusion Department must be correctly filled in with three points of identification: full name date of birth hospital number/ NHS number/AE number and/or first line of address Also required is Collector's signature, date and time of collection and the signature of the requesting doctor All requests for the following tests must be made on the pink Blood Transfusion request card: -group and save serum -group and crossmatch -request for any blood products. All other requests may be made on the normal pathology request card. All specimens sent to the Blood Transfusion Department must be clearly identifiable and labelled with the following information: surname and forename date of birth date and time of sample hospital number/ NHS number/AE number and/or first line of address ward if applicable. see under 'The Request Card' on page 8 and Labelling of Samples on page 13 for further information. Incomplete request cards and/or samples will not be accepted. Addressograph labels are not acceptable on any samples. Unlabelled samples will not be accepted under any circumstances. They will be disposed of to protect patients. Inadequately labelled specimens will also not be accepted. Accident & Emergency “unknown” patients There is a numbering system in the Emergency Department to label samples from Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 34 of 144 any patients who are unable to be identified. The sex of the patient must be added to the request card and an approximate age if not known. This system must be used so that the patient can be clearly identified in the Emergency Department and when they get to theatres. Failure to use the system will result in confusion and delay. The Blood Transfusion Department staff will not add any information to request cards or specimens. If an unconscious patient is subsequently identified, the Department will continue to use the emergency number until a new request card and specimen of blood are received with the patient's full identification. All blood crossmatched using the emergency number will be withdrawn after 12 hours unless the patient is still not identified. Hospital Blood Bank All crossmatched blood is stored in the Blood Bank in the Pathology Department at 4 degrees centigrade which has special alarm systems to protect the blood. It is not permitted to store blood in any other fridge throughout the hospital. Only one unit of blood should be taken at a time unless two drips are being used. There is a cool box provided for theatre use only, when more than one unit of blood is required because of a difficult surgical procedure. Blood may be kept in this box for up to four hours. Any unused blood must be returned as soon as possible. This cool box MUST be used when taking emergency O Rh D Negative blood. Provision of Blood Products The Blood Transfusion laboratory provides the following blood products which must be requested using the pink Transfusion request card. Current guidelines must be adhered to. -fresh frozen plasma -cryoprecipitate -platelet concentrate -iv immunoglobulin -human albumin a) 4.5% 500 mL, 250 mL b) 20% 100 mL -Factor VIII and Factor IX. -other specialised factor products -C1 esterase inhibitor Immunoglobulin Anti-D Immunoglobulin Anti-D is issued by the Transfusion laboratory to all Rh negative women who give birth to a Rh positive infant. The following possible sensitisation events should also receive anti D in Rh D Negative women in the prevention of HDN, 250 IU before 20 weeks and 500 IU after 20 weeks: -still birth -APH -amniocentesis Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 35 of 144 -trauma in pregnancy -abruptio placentae -turning a breech -TOP -threatened abortion -miscarriage/Inevitable abortion (unless <12 weeks and spontaneous) -intrauterine death -post foetal blood sampling -pv bleed (unless <12 weeks) Prophylactic Anti-D The Trust offers prophylactic Anti-D to all Rh D Negative women during their pregnancy. They will receive 1500 IU Anti-D at 28 weeks gestation. Cord bloods are taken at delivery, and if a Rh D Positive child is born, a further dose of 500 IU Anti-D is given. After booking bloods are tested, all Rh D Negative women will receive a blood group card, an information pack on Anti-D Prophylaxis, and an invitation to take part. The midwife orders the Anti-D from the Transfusion Department on special forms and the Anti-D is sent out to the clinic the day before required. See Prophylactic Anti-D Guidelines. Crossmatch blood All blood held for operations will be reclaimed to stock the day after the operation. Any blood remaining 48 hours after the start of any blood transfusion will be reclaimed to stock. If further blood is required, a fresh specimen of blood is needed for a repeat crossmatch. Group and Save serum Specimens sent for Group and Save serum will be tested and are valid for 7 days providing the patient has not been transfused. If a crossmatch is subsequently required, the clinician only needs to phone the Transfusion laboratory to convert the Group and Save serum to a crossmatch. Standards in Blood Transfusion Practice All the Guidelines for Blood Transfusion and blood component therapy are contained in the document “Standards in Blood Transfusion Practice” which is available on each ward station and via the intranet. Blood Bank Training It is essential that all staff who remove blood from the Blood Bank have received training. Blood Bank training can be arranged to train staff in the hazards of blood transfusion and the procedure for removing blood from the Blood Bank. This is also accompanied by the NBA film, “The Strange Case of Penny Allison” which points out the dangers in Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 36 of 144 Blood Transfusion. All staff attending will receive a certificate of training, and a log on code for the computer system. Contact Mr Roger Chant for training information or book on the MLE website. Antenatal Antibody Clinic Pregnant ladies with antibodies should be referred to the Transfusion Specialist Practitioner Roger Chant who will discuss with them the nature and problems associated with the antibodies. Appointments can be made via ext 4756 or ext 3290 Indications for Blood Transfusion Requests General Surgery Patients to Group and Save: Abdominoplasty Amputation of Leg - Above and Below Knee Angiography Angioplasty Bowel Resection Breast Reduction Breast Excision Cholangiogram Cholecystectomy laparotomy/laparoscopy Common Bile Duct Exploration Closure of Colostomy / Revision Embolectomy Endoscopy Grafting of Burns Haemorrhoidectomy Hartmans/Reversal Hemicolectomy Hiatus Hernia Repair Ileostomy/Revision Ileostomy Laparoscopy Laparotomy Liver Biopsy Liver Resection Low Anterior Resection Mastectomy Myelogram Oesophageal Dilation Open Pleural / Lung Biopsy Parathyroidectomy Perforated Ulcer Pyeloplasty Radical Open Prostatectomy Rectopexy Polypectomies Sclerotherapy Tonsillectomy Thyroidectomy - Partial / Total Tracheotomy TUR Prostate TUR Bladder Tumour Ureterolithotomy Vagotomy/Highly Selective Vagotomy Varicose Vein Removal Patients to Crossmatch: Abdo Perineal Resection Adrenalectomy Anterior Resection Aortic Aneurysm Repair Aorto Femoral Bypass Axillo Femoral Bypass Bifemoral Bypass Colectomy Cystectomy Femoro Popliteal Bypass Gastrectomy / Partial 2 Units 3 Units 2 Units 4 Units 2 Units 2 Units 2 Units 2 Units 2 Units 2 Units 2 Units Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 37 of 144 Laryngectomy Lobectomy / Pnemonectomy Nephrectomy Oesophagectomy Oesophagogastrectectomy Patients to Crossmatch (cont’d): General Surgery 2 Units 2 Units 2 Units 4 Units 4 Units Panproctocolectomy Parks Pouch Pseudomyxoma Renal Transplant Splenectomy Whipples Operation 2 Units 2 Units 4 Units 2 Units 2 Units 4 Units Obstetrics Patients to Group and Save: APH Breech Foetal Distress Grand Multi Para PET / Hypertension Placenta Previa Standby Type minor Retained Placenta Twins / Triplets Patients to Crossmatch: LSCS with Hb Less Than 100 g/L LSCS with Rare Antibodies Placenta Previa Standby Type major Placenta Previa LSCS Type minor Placenta Previa LSCS Type major Abruption Caesarian Section Forceps Induction of Labour Previous PPH / APH Repeat LSCS Trial of Scar / Labour Unstable Lie 2 Units 2 Units 2 Units 2 Units 4 Units Gynaecology Patients to Group and Save: Aldridge Sling Colposuspension Dilation and Curettage Foetal Death Molar Pregnancy Oophorectomy Simple Pelvic Floor Repair Hysterectomy Tubal Surgery Ectopic Pregnancy Laparotomy Termination of Pregnancy Cone Biopsy ERPC Incomplete Miscarriage Myomectomy Ovarian Cyst / Mass Reversal of Sterilization Trans Cervical Endometrial Resection Vaginal Repair Salpingectomy Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Patients to Crossmatch: Oophorectomy Radical Pelvic Exenteration Ruptured Ectopic Vulvectomy Wertheims Hysterectomy Page 38 of 144 2 Units 4 Units 2 Units 2 Units 2 Units Orthopaedics Patients to Group and Save: ACL Arthroscopy Bone Grafting Discectomy Fracture Neck of Femur* Internal Fixation of Humerus Internal Fixation of Ankle Laminectomy Removal of Metalwork Spinal Decompression Total Hip Replacement Amputation Below Knee Austin Moore Decompression Dynamic Hip Screw* Internal Fixation of Tibia / Fibula Internal Fixation of Radius / Ulna Internal Fixation of Patella Osteotomy Tibial / Femoral Spinal Fusion Spinal Block Total Knee Replacement** *unless significantly anaemic **Autologous blood salvage technique available, see “Standards in Transfusion Practice document for details Patients to Crossmatch: Fracture Shaft of Femur Osteotomy Pelvic Bilat Hip Replacement Revision Hip Replacement Bilat Knee Replacement Revision Knee Replacement Traumatic Above Knee Amputation "Aggressive" Spinal Decompression 2 Units 2 Units 3 Units 3 Units 2 Units 2 Units 2 Units 2 Units Anticoagulant Services The Haematology Department provides a comprehensive anticoagulant outpatient monitoring service through a team of experienced Consultant, nursing and scientific staff. The laboratory utilises a computerised anticoagulant management programme, which facilitates warfarin dosing, makes appointments and records length of treatment and clinical and drug histories for all patients. The laboratory provides a report to patients GP on each visit with details of INR, current dosage and the next appointment. Patients receive their Anticoagulation letter with Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 39 of 144 recommended dosage by return of post. When results indicate (eg large dose changes or raised INR results), patients are contacted immediately by telephone if possible. Clinics All new patients attend the anticoagulant clinic at the Haemophilia Centre for their first INR check and are seen by the Nurse Practitioner who will also see GP referrals. Subsequently the patient may continue to attend a hospital-based clinic or be bled at their GP surgery, with their sample and warfarin request sent to the laboratory. If attending the hospital, patients only need to see the Nurse Practitioner when they have an anticoagulant related problem or if unstable. All other hospital and GP patients have their warfarin dosage returned by post. Referral for Out-patient Anticoagulant Monitoring To enable the department to provide safe and appropriate anticoagulant monitoring, it is MANDATORY that the following information is sent to the Anticoagulant Nurse Practitioners c/o Pathology Office, prior to the patients appointment date at the anticoagulant clinic. If patients have been started on anticoagulant therapy by their GP this information MUST accompany first sample sent to the laboratory. Please fill in anticoagulant chart or send letter providing ALL the following information: -Patients name, address, telephone number and hospital number, NHS number -Indication for anticoagulant therapy, history, previous thromboembolism episodes -Target INR -Duration of anticoagulation -Other medication -GP name and address -Intercurrent illnesses, e.g. ulcer, hypertension -Previous warfarin dosages up to date first seen in anticoagulant clinic Hospital Clinic times Basingstoke and North Hampshire Hospital Monday and Thursday 0900–1200 hrs Alton Community Hospital Wednesday 0900–1030 hrs GPs are encouraged to bleed anticoagulant patients on a Wednesday but if this is difficult, please avoid Fridays. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 40 of 144 HISTOPATHOLOGY Outline of service The Histopathology Department offers a routine histology service including immunohistochemistry, Her-2, non-gynaecological cytology and a rapid service for frozen sections. It also liaises with the mortuary service who perform post mortem examinations. Normal hours of service Histology - Monday to Friday 0900 to 1715 hrs Mortuary - Monday to Friday 0800 to 1600 hrs Samples and labelling Interpretation of a specimen is highly subjective and dependent upon the information supplied with the specimen. The request card must be completed fully and legibly. The absence of clinical details may prevent the issuing of a meaningful report. Incorrect or inadequate patient details will result in a delay as the specimen will be returned to the sender for verification or alteration. As part of obtaining informed consent for surgery and histology investigations, your patient must be aware that blocks and slides are archived for future review should this be necessary and may contribute to good laboratory practice procedures such as quality control, audit and teaching. It is an essential requirement for Histopathology investigations that the requesting clinician signs and dates the request card to indicate that informed consent has been given. Where several specimens are sent from one patient, the specimens must be clearly identified together with the request card. All specimen labelling MUST BE on the container, NOT on the lid. If there is a danger of infection, e.g. TB, hepatitis, HIV, the specimen and the request card must be clearly labelled. Routine Histology Specimens Specimens for routine histology should be placed in at least three times their volume of 10% buffered formalin. Routine Cytology Specimens Non-Gynae Cytology specimens including Joint fluids, urines and sputum should be collected in 30-60ml non sterile universal white top containers All cervical smears (Gynae Cytology) are examined at RHCH Winchester. Where there is a Danger of Infection (e.g. tuberculosis, hepatitis B, HIV positive), the specimen container and the request card must be so identified. Specimens and Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 41 of 144 request cards will normally be transported in the plastic bags provided, but special care to ensure that this is so will be needed where there is Danger of Infection. Please discuss such cases with the Consultant Pathologist before such specimens are sent - a risk assessment will need to be made before the work is carried out. Pleural, ascitic fluid and cyst aspirates:A small amount (20 to 30 mL of the fluid) should be sent to the laboratory as quickly as possible. Please do not send the whole drain bag to the laboratory. Where delay is likely, e.g. over the week-end, store in a 4o C refrigerator. FNA sample requirements:Slides – Slides MUST be labelled with TWO points of patient identification as a minimum (Full name and NHS/Hospital number or DOB). This should be written on the slide in pencil prior to applying fixative. Aspirates – 30/60ml non-sterile universal container with patient information written in pen as above. Training in FNA slide preparation is available by contacting the Histopathology Department manager on ext 3280. Urgent Specimens Urgent specimens should be clearly marked as URGENT and delivered to the laboratory as soon as possible. For small specimens a report will normally be issued the next working day. The sample must arrive in the laboratory by 5pm at the latest for next day results. Same-day reporting may be possible on small biopsies provided this is discussed with the Consultant Pathologist prior to sending the specimen and the specimen is received in the laboratory before 1100 hrs. Frozen Sections Specimens for frozen sections must be placed into a suitable container without formalin or any other preservative or liquid. Frozen sections must be booked at least 24 hours in advance to ensure a Consultant Histopathologist is available. The nature of the clinical problem should be discussed with the Pathologist at the time of booking to ensure optimum interpretation. The case should be first on the operating list and the laboratory MUST be informed if the frozen section is cancelled. Where possible, unplanned frozen sections will be accommodated, but the laboratory must be telephoned prior to sending the specimen. The Consultant Histopathologist may wish to discuss the nature of the problem briefly with the surgeon/anaesthetist concerned at this time. The specimen MUST be handed to a member of staff within the Histology Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 42 of 144 Laboratory. It must not be left at Pathology Reception or elsewhere within the laboratory. Please write the extension number to which the report is to be phoned clearly on the request card. Where there is a danger of infection, frozen sections will not normally be performed in order to reduce the risk of exposure of laboratory staff to infectious material and to avoid the withdrawal of the frozen section service for 24 hours whilst the cryostat is decontaminated. Direct Immunofluorescence (Skin Biopsies) A fixative solution is available from the laboratory for these samples. Once collected they should be sent to the laboratory as soon as possible. Post Mortems See 'Mortuary'. Reports Reports are available from the Ward Enquiry System. Printed reports, where necessary, are sent out on the same day that the report is available on the computer. The Consultants preliminary findings may be discussed prior to the issue of the final report if clinically required. Turnaround times The departments Turnaround time targets are as follows: Diagnostic Biopsies – 90% in 5 days All other Histology – 90% in 10 days FNA Cytology – 90% in 5 days All other Cytology – 90% in 5 days Specimens requiring decalcification will take longer, possibly up to several weeks. Larger or more complex specimens may take longer. HISTOLOGY routine reference laboratories HER2, EGFR and KRAS testing are referred to Source Bioscience, 1 Orchard Place, Nottingham Business Park, Nottingham. NG8 6PX. TAT 14 DAYS Lymphoma referrals are sent to Cellular Pathology, Level E, Southampton General Hospital, Tremona Road, Southampton. SO16 6YD. TAT 28 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 43 of 144 MORTUARY Deaths in hospital You will normally be asked to certify death promptly, whether by day or night. If relatives are present you should see them with the nurse in charge who will support you and will then know what has been said. The body is then laid out, with hands placed by the patients’ sides, eyes and mouth closed where possible and all drains, catheters lines and cannulas left in situ. The Notification of Death form is then filled out with the blue copy attached to the patients shroud and the green to the sheet they are wrapped in. A wristband with the patients details must be placed on both the wrist and the ankle. Where there is a danger of infection (Hepatitis B, HIV, Tuberculosis etc.) the body is placed in a leak-proof body-bag, and marked with a 'Danger of Infection' label attached to the outside of the body-bag. For a list of infections that require body-bags please see the trust infection control policies. Please note that both MRSA and C. Difficile Patients DO NOT require body-bags. For reasons of confidentiality the nature of the infection is not stated. On receipt of the patient in the Mortuary, the Pathology Technicians will contact the ward to ascertain the nature of the infection, this is necessary as Exposure Prone Procedures may need to be undertaken. The precise nature of the infection is not passed to the Funeral Director; however they are informed a danger of infection is present and that embalming should not be carried out. Having recorded the fact of death you must decide whether you can accept "jurisdiction" over the death and can complete a Death Certificate. This means that you have treated the patient within the last fourteen days, that death has not been from an industrial cause, from an accident or overdose or is unexpected as from unknown causes or has occurred during an operation or before recovery from an anaesthetic. Such deaths must be referred to the Coroner. See Deaths to be reported to the Coroner (p45). Death Certificates Please deal with death certificates before you start on other work in the morning. It is the policy of the Hospital that when relatives arrive following a death, all personal items, together with the Death Certificate are ready and waiting. Relatives will normally be seen by the Patients & Relative Support Manager, extension 4777, bleep 1100. Relatives must not be asked to return later to collect the death certificate. Death Certificates for infants dying within 28 days of birth are to be issued from the book entitled "Medical Certificate of the Cause of Death of Live born Children Dying within the First 28 days of Life". Cremation Papers The Patient & Relative Support Managers also handle cremation papers. Please complete promptly and do not leave them in the Information Room. It should be remembered that the forms have to be at the Crematorium 24 hours before the Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 44 of 144 actual cremation takes place. For a Cremation paper to be completed, two parts must be filled out by two different Doctors. The first doctor will need to be one who treated the patient during their last illness. This will usually, but not always, be the doctor completing the death certificate. The second doctor must be on a different team to the first and have at least five years registration with the GMC. Both Doctors will need to have performed an external examination of the patient after death. This usually takes place within the Mortuary but can be undertaken on the ward. To make an external examination in the Mortuary, the department must be contacted on ext.4749 to arrange a suitable time. Pacemakers Should a pacemaker be fitted, this must be removed before cremation. This will be done at the Funeral Directors. If you are completing a Cremation Paper it must be indicated that a Pacemaker is in situ but that it has not been removed. Please ask The Patients & Relative Support Manager (ext 4777, bleep 1100) or the Mortuary (ext.4749) for further advice if necessary. Routine Post Mortems For a Routine Post Mortem to be requested you must be able to certify the death. If not the case should be referred to the Coroner for a Coroners Post Mortem. Should a routine Post Mortem be requested, a signed appropriate consent will be required (normally obtained by your consultant). The Patients' & Relative Support Manager, (ext 4777, bleep 1100) will arrange for the relatives to be spoken to in the office on B level (normally between 0900 to 1200 hr). Wherever possible we avoid relatives having to return to the ward. They deal with patient’s personal possessions and advising relatives about registering the death with the Registrar, the death certificate, funeral and cremation arrangements. The Patients & Relative Support Manager will always be willing to advise you. The patient's notes together with the completed request form and signed permission from the next of kin are forwarded by the Patient & Relative Support Manager to the Mortuary. It is the responsibility of the Doctor to ensure prompt transfer of the patient notes etc. to the Patient & Relative Support Manager to avoid delay and distress to relatives anxious to proceed with funeral arrangements. Please put the signed consent form attached to the front of the patient's notes with the PM request form in an envelope and "post" through the letter box provided in the Patient & Relative Support Manager office outside normal working hours. Failure to carry out this procedure may result in the request being overlooked or delayed, leading to added distress to the relatives. Post mortems will normally be performed the morning of the next working day after the paper work is received in the mortuary. The Death Certificate must be completed before the Post Mortem so that relatives are not delayed organising the funeral. Provided the box on the death certificate is marked, the OPCS will write to the Pathologist at a later date asking whether the PM findings alter the certified cause(s) of death. This information is then used for statistical purposes only. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 45 of 144 Please write your name and bleep number clearly so that you can be invited to attend. If it is not possible for you to attend, the Pathologist will normally bleep you with the findings later. A written report is sent to the consultant with a copy to the patient's GP, provided this information is given on the request form. Danger of Infection Please contact the Consultant Histopathologist where there is a known or suspected infection (e.g. Hepatitis B, C, HIV, and Tuberculosis). A Post Mortem will not normally be carried out. A risk assessment will be made and a modified procedure may be possible. The request form should be clearly marked. Deaths to be reported to the Coroner You cannot accept jurisdiction (i.e. cannot complete a death certificate) for deaths resulting from: - Fractures or other injury resulting from road traffic accidents or other accidents. - Drugs, toxins, or alcohol poisoning. - Privation or neglect. - Recovery from anaesthetic. - Prisoners or patients held under Sections of the Mental Health Act. - Occupational disease e.g. asbestosis - Intra-operative deaths. - Suicides These cases must be referred to the Coroner (Mr. A. Bradley, 01256 478119), or the Coroner's Officer at Basingstoke Police Station (01256 405015). There is no rule that deaths within 24 hours of admission must be reported to the Coroner provided you are sure of the cause of death. If in doubt please do not be afraid to contact the Coroner, he will be only too happy to advise you. Please do not delay - contact the Coroner as soon as possible after 9 a.m. Once the death has been accepted by the Coroner he has jurisdiction over the death and he writes the Death Certificate. He may ask for a Post Mortem to be performed and for which consent from relatives is not required. Once the Coroner has ordered a Post Mortem this is then required by law and the relatives are unable to intervene. Form G28 is then completed by the Coroner's Officer. The information needed by the Officer is obtained from the patient's notes and interviews with relatives etc. conducted normally from the Patients & Relative Support Manager on B. Level. There should be no need for police officers to come to the ward except occasionally at weekends. Post mortems for the Coroner are normally performed the morning after receipt of the G28. Unless it is likely that there will be an inquest, the consultant and/or GP will be sent a copy of the report. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 46 of 144 An inquest is usually held where death is from unnatural causes (e.g. trauma). You may be asked for a statement (through the Patient & Relative Support Officer). On rare occasions you may be asked to attend the inquest; if so always inform your consultant. Foetuses Foetuses All Foetuses under 14 weeks must be taken to Histology. Foetuses delivered out of normal hours should be refrigerated at 4 degrees Celsius in the department and sent to Histopathology at 09:00hr the next working day. The Mortuary at the Basingstoke and North Hampshire Hospital will be the receiving area for all specimens over 14 weeks. Foetuses will not be accepted without a pregnancy loss and infant death form, Infant Release form, Notification Plan and a completed Pathology request form if it is required for Histology. All foetuses must be sent fresh without formalin. If private burial is required it MUST be noted on the request card. Parental consent is required before Histological examination can be carried out and a completed Post Mortem consent form must be sent with the request card with any other documents according to the current protocols. The placenta should accompany (also sent fresh). If the foetus needs a Post Mortem examination it will be sent to Southampton General University Hospital. Results will usually be known two weeks after the foetus has been sent. Viewings During Core hours Viewings can be arranged between the hours of 10:00am and 16:00pm and should be arranged via the Patient & Relative Support Manager (ext.4777 Bleep 1100). They will then contact the Mortuary to arrange a specific time for the relatives to attend. Viewings are assigned 45 minute sessions in the Mortuary to attempt to accommodate all requests. The 45 minute session is when the relatives may be within the viewing area and does not start from when they arrive on site. Late arrivals may be allowed an extra 15 minutes depending on workload. The last available time for a viewing will be at 15:15. Allowance is made for the Maternal and Child Health Division and times may be booked outside these hours with prior arrangement with the Mortuary (ext. 4749) Outside of Core Hours An out of hours viewing service operates on weekends and Bank Holidays between 11:00 and 16:00. Monday to Friday all viewing arrangements must be made within the core hours. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 47 of 144 Viewing arrangements discussed outside of these times will be solely at the discretion of the on call Pathology Technician due to other essential Trust commitments provided by the Mortuary department. A minimum of 1 hours notice must be given before any arrangement can take place out of hours. To arrange a viewing out of hours the on call Pathology Technician must be contacted through the Hospital Bleep Holder on bleep 1436. Once a time has been arranged the relatives should make themselves known to the receptionist at the Hospital main entrance on B floor. The On call Pathology Technician will then meet the relatives at the main entrance and escort them to the Mortuary. When arranging a viewing you must clearly indicate that the time agreed is the time that the relatives should be at the main entrance, and that the appointment is for 45 minutes. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 48 of 144 MEDICAL MICROBIOLOGY Medical Microbiology and Control of Infection contact details For consultant clinical advice and interpretation of results or laboratory technical advice, microbiology results, to arrange urgent investigations or for control of infection matters. Dr Nicki Hutchinson, Consultant Medical Microbiologist, infection control lead (bleep 2305), ext 3310 Dr Fatima El Bakri, Consultant Medical Microbiologist ext 3305 Dr Jorge Cepeeda, Consultant Medical Microbiologist ext 3308 (Consultant on call available through switchboard out of hours) Mr Dave Thomas, Laboratory Manager ext 3311 Laboratory enquiries ext 4904 Senior Control of Infection Nurse (bleep 2364), ext 6774 or 3734 Outline of Service The medical microbiology department offers a full range of investigations in bacteriology, mycology, serology, parasitology, virology and PCR based testing through its in-house facilities and links to referral centres. It provides a 24 hour, 7 day urgent service for rapid clinical decision making. Normal working hours are 0900 – 1730hrs Monday - Friday The department is headed by three Consultant Microbiologists who are always available for clinical advice. A Consultant Microbiologist also leads the Infection Control service with a senior and two junior infection control nurses. 'Mass Screening' should not be instituted without prior discussion with the Senior Nurse Infection Control or a Consultant Medical Microbiologist. Control of Infection The infection control team provide a pro-active ward based service for the Basingstoke and North Hampshire Hospitals NHS Trust and are also available to give advice on all infection control issues, such as screening for MRSA, isolation of infectious patients. The nurses are available on bleeps 2364, 2365 and 2366 between the 0700 and 1700 hours. At other times contact the on-call Consultant Microbiologist for advice Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 49 of 144 On-call services Monday – Friday 5.30pm – 9.00am Telephone: 07721881673 Saturday – Sunday 9.00am Telephone: 07721881673 Sunday – Monday 9.00am Telephone: 07887794673 Sample requirements - Microbiology If reliable results are to be obtained, the following points should be observed when taking specimens: All specimens must be labelled with the patient's full name, date of birth and date and time of collection. They must be accompanied by properly completed request cards which state the NHS number/hospital number, name and date of birth of the patient, the ward or surgery, the name of requesting medical officer, the nature of the specimen and the site from which it was taken, the clinical diagnosis and duration of illness, the nature of any antibiotic therapy (including recent or intended treatment) and finally the investigation required. Separate specimens must have separate request cards. Specimens for microbiological investigations must never be in contact with any antiseptics or disinfectants, e.g. Hibitane, or preservatives, e.g. Formalin. All specimens for culture must be sent to the laboratory immediately after collection. Whenever possible specimens should be sent early in the day so that there is time to examine them during normal working hours. The laboratory must be notified when urgent specimens are being sent. All specimens and request cards from patients who are HIV-antibody positive, suffering from Hepatitis B or C or Tuberculosis, or patients who may have these conditions, must be labelled with 'Danger of Infection' stickers. These specimens must be sent in a sealed plastic bag. Specimens must be sent in proper laboratory containers which are available from Pathology Reception. The laboratory will refuse to investigate any pecimens received in improper containers or hazardous conditions. If there is any doubt about an investigation, or an investigation not listed below is required, please consult the laboratory before obtaining a sample. Specimen Collection/Sample Requirements Best results are obtained when an appropriate, well taken specimen, in the correct container, is delivered to the laboratory promptly with the relevant clinical information on the request form. Further information regarding the collection of specimens can be found in the test index. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 50 of 144 Microbiology samples MUST be accompanied by a request form stating the following information: o Clinical details including travel history o Any antimicrobial therapy o Date of onset and duration of illness o The anatomical site of any wound o Useful epidemiological information e.g. In cases of diarrhoea, occupation of adults, nursery or school of children, any occupational or recreational risks Leaking samples will not normally be processed Requesting Extra tests Extra tests on samples maybe requested within 48hrs of the sample collection, however, additional investigations will only be carried out as deemed appropriate by the Clinical Microbiologist. Individual test details For full test details see test index. Actinomycosis Blood culture Pus in a sterile container is essential. Swabs are extremely unreliable Reports usually ready within 2weeks. Use only BacT-Alert bottles. Clean the collection site and the rubber bungs of the blood culture bottles with alcohol wipes prior to specimen collection and allow to dry. Blood from adults should be split into aerobic and anaerobic bottles. NOTE – fill anaerobic bottle first unless using safety collection sets/butterfly needles then fill aerobic bottle first due to air in the tubing. A single Paediatric bottle should always be used for children. Do not remove the bar codes from the bottles nor obscure them with labels. Reports usually ready within 24 hours but some organisms take longer Cerebro-spinal fluid Collect 0.3 mL into a fluoride oxalate tube (for glucose) and 0.5 mL into 3 or 4 separate sterile plastic universal containers. Universals No. 2 and 3 are sent to us for the bacterial and viral studies. The fluoride oxalate sample and universal No. 1 (which may be contaminated with skin organisms) should be sent directly to Chemical Pathology. NOTE – if spectrophotometry for xanthochromia required, collect a fourth universal containing 1 mL CSF and send to Chemical Pathology. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 51 of 144 Always contact the laboratory when sending a CSF Microscopy will be phoned as soon as possible. Culture usually ready within 24-48hr. Faeces (for microscopy and/or culture) For ova, cysts and parasites, hot stools are not necessary. The specimens for both microscopy and culture must be sent in a standard screw-capped container, available from Pathology reception. Select a sample of stool not contaminated with urine. Make sure the top is screwed on tightly to prevent leakage. Place container in self-sealing plastic bag and deliver to the laboratory. For threadworm ova - see separate entry. Rectal swabs should only be sent if faeces are unobtainable. Relevant information required: - the age of the patient - whether the patient has been abroad and where? - date of onset of illness - antibiotic therapy especially if Cl. difficile is suspected Unless otherwise indicated, specimens will only be cultured for Salmonella, Shigella, Campylobacter and E. coli 0157. The investigation of Rotavirus, Norovirus and Adenovirus will be carried out on appropriate stools. Cl. difficile toxin will only be investigated after Microbiology Consultant/Infection Control review. Microscopy reports usually ready same day. Culture up to 3 days Fungi Scrapings of the skin, nail clippings, plucked hair, etc. should be placed in folded clean black paper and sent to the laboratory in a labelled paper envelope. Reports usually ready: Microscopy 1 week. Culture 2-3 weeks Genital Specimens Gonorrhoea Female: Cervical and urethral (NOT high vaginal) swabs should be sent. Suspicion of gonorrhoea must be indicated on the request cards. Reports usually ready within 2 days Male: Urethral swabs should be sent. Suspicion of gonorrhoea must be indicated on the request cards. Reports usually ready within 2 days Trichomonas vaginalis High vaginal swabs. Diagnosed microscopically. Reports usually ready within 1 – 2 days Gardnerella vaginalis/ bacterial vaginosis High vaginal swabs. Diagnosed microscopically. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 52 of 144 Reports usually ready within 1 – 2 days Candida High vaginal swabs. Diagnosed microscopically and on culture Reports usually ready within 1 – 2 days Chlamydia Endocervical swabs for female patients and urethral swabs from males. The swabs must be “Chlamydia swab” and placed into the correct transport medium. A NAAT test performed on the first void urine is now the standard test. Reports usually ready within 4 days Antibiotic levels – Gentamicin, Tobramycin, Teicoplanin and Vancomycin Gentamicin and Vancomycin levels are performed by Blood Sciences. Tobramycin and Teicoplanin are referred by Microbiology. Use microbiology request card. Samples must reach the laboratory by 1100 hr. Requests out of hours will be referred to the Consultant Microbiologist on call. Reports usually ready by 1400hr. Respiratory Syncytial Virus Nasopharyngeal aspirates should be sent. Do not send mucoid specimens as these give uninterpretable results. Please consult the laboratory before sending specimens for investigation. This test is only available during late autumn and winter. Reports usually ready within same day Serous fluids These should be sent in sterile laboratory container e.g. universals and NOT histology pots (these are not sterile, may contain formalin and are not leakproof). Reports usually ready within 2 days Sputum (for tuberculosis see below) For routine microscopy, culture and sensitivity, collect sputum sample, the result of deep cough (preferably early morning) into a plastic screw-capped container available from Pathology reception for this purpose. Non-purulent, salivary specimens will not be examined, nor will specimens which are more than 12 hours old. NOTE – to exclude TB, three consecutive early morning sputa must be sent for testing In patients with a severe pneumonia, consider sending urine for pneumococcal and legionella antigen testing. Reports usually ready within 2 days Surgical (eg biopsies and tissue samples) These should be sent in sterile laboratory containers. If the specimen is small and in danger of drying out, add a little Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 53 of 144 normal saline to it. DO NOT send specimens for microbiological investigation in formalin. Reports usually ready within 2 days Swabs NOTE - if pus is available, send this in a sterile laboratory container rather than a swab. Transwabs should always be used but special ear, nose and throat swabs are available if a small swab is needed. All these swabs are available from Pathology reception. Inoculated swabs should be kept at room temperature out of direct sunlight. Note: swabs have expiry dates; please use oldest stock first. With ‘ wound’ swabs it is very important to state the site and nature of the wound, be it a cut, bite, operation wound etc. and also the type of operation that has been performed as this will help us differentiate between commensals and pathogens. A commensal in one site could well be a pathogen in another. Reports usually ready within 2 days Threadworm ova (Sellotape slide) If threadworms are suspected, a sellotape slide should be obtained as follows. Obtain a glass slide. Apply a single strip of sellotape (2 inches long) to the anal area first thing in the morning before washing or passing faeces. Stick sellotape FLAT on the slide without folds and label the end of the slide. Place the slide in a slide box (available from the laboratory) and send to the laboratory. Reports usually ready within 24 hours Tuberculosis Sputum - The result of a deep cough (preferably early morning) should be collected in a sterile plastic screw-capped container, available from Pathology reception. Reports usually ready within 3-8 weeks. Antimicrobial sensitivities take another 4-8 weeks. Microscopy 1-2 days. Urine Culture - Three consecutive early-morning specimens of 200ml each are required. Bottles available from Pathology reception. Reports usually ready within 3-8 weeks. Antimicrobial sensitivities take another 4-8 weeks Other specimens - e.g. bronchial brushes, serous, (pleural) and peritoneal fluid CSF and pus. These should be collected in sterile containers, e.g. universals. Reports usually ready within 3-8 weeks. Antimicrobial sensitivities take another 4-8 weeks Body Tissues - Again in sterile containers and if in danger of drying out, add a little sterile normal saline. Reports usually ready within 3-8 weeks. Antimicrobial sensitivities take another 4-8 weeks Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 54 of 144 NOTE – samples can be fast tracked for TB PCR when clinically indicated. Urines (for TB see above) A clean urine specimen, if possible midstream, should be collected directly into a sterile plastic boric acid bottle marked 'For Bacteriological Use Only'. This bottle contains boric acid crystals as a preservative - DO NOT WASH THESE OUT. These bottles MUST ALWAYS and ONLY be used for the diagnosis of urinary tract infections Details of antibiotic therapy is vital for correct interpretation of results. After collection the sample should be kept at room temperature and out of direct sunlight until arrival at the laboratory. Reports usually ready within 1-2 days Viral cultures Viral swabs for Herpes (HSV) investigations are conducted in house, whilst other viral investigations are conducted at a reference laboratory Whooping cough Special culture medium is used for the culture of Bordetella. Therefore it is very important to give prior warning to the laboratory so that such medium can be prepared. Pernasal swabs (available from the laboratory) should be taken and inoculated directly onto culture medium. This should then be returned to the laboratory as soon as possible. Culture is of little value if symptoms have been present for more than one week or if erythromycin has been given. Reports usually ready within – at least 3 days Worms Whole worms or segments should be sent in a glass or plastic container. Reports usually ready within 24 hours Sample requirements - Serology For all serological investigations send 10 ml of clotted blood i.e. in a plain bottle with no anticoagulant). The following tests are performed at The Basingstoke and North Hampshire Hospital. Hepatitis A IgM For diagnosis of acute illness. State date of onset of hepatitis /jaundice. Reports usually ready within 1 day Hepatitis A Total Post vaccination or for confirmation of past infection Reports usually ready within 2-3 days Hepatitis B Surface Antigen State risk factors (unless routine screening in pregnancy) Reports usually ready within 1 day Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 55 of 144 Hepatitis B Surface Antibody State date and number of immunisations. Reports usually ready within 1 week unless needle stick injuries which will be ready within 48 hours Hepatitis B Core Antibody For detection of previous infection or natural immunity Reports usually ready within 1 week Hepatitis B e Antigen To determine level of infectivity Reports usually ready within 1 week Hepatitis B e Antibody To determine level of infectivity Reports usually ready within 1 week Hepatitis C Antibody State risk factors (otherwise test will not be done) Reports usually ready within 1 week HIV Antibody State risk factors (unless routine screening in pregnancy) Reports usually ready within 1 day Rubella Screening Only used for evidence of past infection Reports usually ready within 1 week Syphilis Serology State symptoms and whether there is a past history of Treponemal infection. Reports usually ready within 1 week Lyme Disease Serology (screen only) State whether history of tick bite and date of onset of rash or other symptoms. Reports usually ready within 1 day Influenza Rapid Diagnostic Test Only available after discussion with Consultant Microbiologist Toxoplasma Serology (screen only) There is no value in routine screening in pregnancy. Reports usually ready within 1 day Varicella/ZosterVirus antibody Used only for pregnant women and immunosuppressed patients who have been exposed to infection. Reports usually ready within 1 day Helicobacter Faecal Antigen Testing Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 56 of 144 Reports usually ready within 1 week CMV IgG Antibody As clinically indicated Reports usually ready within 1 week CMV IgM Antibody As clinically indicated Reports usually ready within 1 week Norovirus EBV Capsid For use in outbreaks Reports usually ready within 1 week For clinical diagnosis of acute disease Reports usually ready within 2 weeks EBV Nuclear As above Other tests All other serological test are performed at reference laboratories. 10mL clotted blood should be sent and must be accompanied by a separate request card for each test requested. Request cards must have full clinical details. Especially important is the date of onset of the illness. Any specimen without full detailed history of illness or the date of onset will not be forwarded. If possible, acute and convalescent sera should be sent. (Convalescent sera should not be collected earlier than 10 days after the onset of the illness.) Special note on Meningococcal Serology and PCR In order to confirm the diagnosis of meningococcal disease in patients who have already received antibiotics the following are necessary: - An acute specimen of clotted blood taken around the time of admission. - An EDTA sample of blood taken on admission. - A convalescent specimen of clotted blood taken about seven days after the onset of symptoms. These tests are carried out at Manchester PHL Communicable Diseases The following diseases (or suspicion of) are notifiable by law to the Consultant in Communicable Disease Control; the clinician who considers or diagnoses the infection is responsible for the notification. Persistent carriers of typhoid bacilli and other Salmonellae should also be reported. For optimal in-hospital infection control, the Infection Control Team must also be informed. Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 57 of 144 List of Notifiable Diseases (2010) Acute Encephalitis - bacterial and viral Acute Meningitis Acute Poliomyelitis Acute Infectious Hepatitis Anthrax Botulism Brucellosis Cholera Diphtheria Enteric fever Food Poisoning (or suspected food poisoning) Haemolytic Uraemic Syndrome (HUS) Infectious bloody diarrhoea Invasive Group A Streptococcal disease and Scarlet Fever Legionnaires’ Disease Leprosy Malaria Measles Meningococcal septicaemia Mumps Plague Rabies Rubella SARS Smallpox Tetanus Tuberculosis - pulmonary and non-pulmonary Typhus Viral Haemorrhagic Fevers (VHF) Viral hepatitis Whooping Cough Yellow Fever As of April 2010, it is no longer a requirement to notify the following diseases: dysentery, ophthalmia neonatorum, leptospirosis and relapsing fever. Notification should be made by telephone in the first instance followed by notification on the official form to: Hampshire & Isle of Wight HPU Unit 8 Fulcrum 2 Solent Way Whiteley Farham PO15 7FN Tel: 0845 055 2022 Fax: 0845 504 0448 Email: hiowhpu@hpa.org.uk Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 58 of 144 To contact a public health doctor in an emergency out of hours; in the evenings, at weekends or during bank holidays, please call: 02380 77 72 22 Notification by phone only must also be made to the Infection Control Department (Ext. 6774). Out of hours contact the on-call Medical Microbiologist. The Infection Control Department should also be informed of any diseases/pathogens not listed here which present a risk of hospital acquired infection e.g. MRSA, Group A Streptococcus in a wound etc. Reports Reports on all specimens are issued to the requesting medical officer immediately the investigations are completed. They can also be seen on the hospital computer system as soon as they have been authorised. Telephone the Department only in cases of urgency. Results thought to be important will be telephoned to the requesting doctor, usually by a Consultant Microbiologist. Under no circumstances will results be given directly to patients. In addition to final results, the following can be found on the computer as soon as they have been processed: -CSF microscopy -the status of blood cultures Please use this facility as it saves time for both you and the laboratory. Availability of Results Please refer to the test index for individual turnaround times. Urgent microscopy results Rapid antigen detection tests Some urgent blood tests with prior arrangement Routine investigations Non routine investigations Referral tests 2 hours 4 hours Same day 2-3 days 3-7 days 14days Results of urgent clinical or public health significance will be telephoned to the requesting clinician. These include: • • • • • • • • • Positive blood cultures Microscopy of non routine cerebrospinal fluids Detection of AFB Significant isolates from faeces samples Positive CD tests Isolates of Group A streptococci Isolates of Group B streptococci from neonates, pre and post delivery HVS Gentamicin assay results MRSA on initial isolation Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 59 of 144 Common causes of spurious results Please ensure that you follow instructions when collecting and storing samples. Inappropriate sample collection, storage and transport can interfere with a number of results. Some examples are given in the table below: Bacteriology Problem Delay in transport/ incorrect post collection storage Incorrect container Unsterile container Leaking samples Lack of appropriate clinical details Common causes Samples not refrigerated Effect Overgrowth of growing bacteria Blue trans swab for virus/chlamydia Overgrowth of bacteria Virus/chlamydia swab for bacteria Household jars medicine containers camera film pots Bacteria killed by container ingredients Contamination or bacteria killed by previous contents. These containers are also unsafe due to potential breakages/leakage in transport Non laboratory approved container Health hazard to all surgery, transport and pathology staff No reference to foreign travel. Appropriate tests not performed. No reference to pregnancy. In complete/misleading No reference to antibiotic results and comments allergies. No reference to past/current/intended antibiotics Serology Problem Haemolysis Incorrect container Lipaemic Common causes Expelling blood through needle into the tube Effect Inaccuracy in many tests. Unable to perform tests Inaccuracy in many tests Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 60 of 144 MICROBIOLOGY ROUTINE REFERENCE LABORATORIES Cambridge PHL Box 26 Addenbrookes Hospital Hills Road Cambridge C42 2QW HPA Virus Reference Division Central Public Health Laboratory 61 Colindale Avenue London NW9 5HT Laboratory of Enteric Pathogens Central Public Health Laboratory 61 Colindale Avenue London NW9 5HT CPA Ref. 1071 CPA Ref. 1883 HPA Microbiology Lab, Level B Southampton General Hospital Southampton SO16 6YD Manchester Medical Microbiology Partnership, PO Box 209 Manchester Royal Infirmary Manchester M13 9WZ CPA Ref. 1683 Birmingham Heartlands Hospital Bordesley Green East Birmingham B9 5ST CPA Ref. 2838 Leptospira Reference Unit Public Health Laboratory County Hospital Hereford HR1 2ER CPA Ref. 0635 Centre for applied Microbiology & Research, Porton Down Salisbury Wiltshire SP4 0JG CPA Ref. 0818 Department of Clinical Microbiology Queen Alexandra Hospital Cosham Portsmouth CPA Ref. 1180 Singleton Hospital Sgeti Swansea SA2 8QA CPA Ref. 1612 Dept. of Microbiology Leeds General Infirmary Great George Street Leeds LS1 3EX CPA Ref. 0989 CPA Ref. 2913 CPA Ref: 0061 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 61 of 144 PHONED RESULTS SHEET: please photocopy and use Patient’s name ................................. DOB ............ NHS/Hospital No: ....................... Consultant/GP…………….. Ward ……………… Date................... Time...................... Signed/Received by ……………………………. HAEMATOLOGY BIOCHEMISTRY MICROBIOLOGY Haemoglobin g/d White cell count 109/lL Platelet count x109/L ESR mm/hr Neutrophils %109/L Lymphocytes %109/L Monocytes %109/L Eosinophils %109/L Glandular Fever MCV fl Haematocrit 109/L Reticulocytes 109/L Sickle test COAGULATION: PT secs PTT secs Fibrinogen g/l D-Dimer Warfarin dose Next appointment TRANSFUSION: Group Rhesus DCT Kleihauer Other tests Sodium mmol/L Potassium mmol/L Urea mmol/L Creatinine umol/L Alk Phos IU/L Bilirubin umol/L ALT (SGPT) IU/L Calcium mmol/L Phosphate mmol/L Magnesium mmol/L CRP mg/L Glucose mmol/L Iron umol/L Uric Acid mmol/L Cholesterol mmol/L HDL Chol mmol/L Triglyceride mmol/L CK IU/L Amylase IU/L LDH IU/L GGT IU/L Tot Protein g/L Albumin g/L Globulin g/L TSH mu/L Specimen: Troponin Gentamicin MICROSCOPY: White cells Red cells Epithelial cells Casts Organisms: CULTURE: ANTIBIOTIC Sensitivity: Penicillin Erythromycin Flucloxacillin Amoxycillin Augmentin Cefalexin Nitrofurantoin Trimethoprim Other tests: ug/l Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 62 of 144 How to get to Basingstoke & North Hampshire Hospital The hospital is located on the A340, Aldermaston Road in Basingstoke: follow the Hospital signs from the Ring Road. By car: There are a number of parking areas available: there is a drop off point and a number of disabled parking spaces available outside the main entrance. Please allow extra time on arrival, as parking is sometimes difficult. Public car parks are now barrier controlled and a pay on exit scheme has been introduced. 0 to 1 hour - £1.00 1 hour 1 min to 2 hours - £2.00 2 hours 1 min to 4 hours - £3.00 4 hours 1 min to 6 hours - £4.00 6 hours 1 min to 24 hours - £5.00 maximum fee There is no charge for disabled parking in the bays marked for this purpose. Please ensure you display your Blue Badge. Cars that ‘enter’ between 19:50 and 05:59 inclusive stay free (regardless of time of exit).This is to ensure that night shift workers and visitors can park safely next to the buildings. The Foundation Trust is serviced by regular buses from Basingstoke town centre: Bus numbers 32 and 32a from Newbury calls at Newbury Bus Station; Chandos Road; Wendan Road; Sandleford Rise; Newbury Tesco; Newtown,A339,A34 Junct.; Greenham Park East; Headley The Harrow Public House; Kingsclere Square; Wolverton Pond; Rooksdown cross roads and Basingstoke and North Hampshire NHS Foundation Trust. Bus number 45 from Sherfield calls at Bramley Station; Post Office; Bramley Church; The Vyne; Sherborne St. John and Basingstoke and North Hampshire Foundation Trust. See www.stagecoachbus.com for up to date timetables. Click here for Basingstoke bus routes Need any help getting to hospital? Neighbourcare: www.neighbourcare.org.uk Basingstoke Community Transport: 01256 320501 or www.bct.me.uk www.hants.gov.uk/passengertransport Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 63 of 144 Traveline is a service which allows you to plan your journey by giving you all the times and routes you need to get to the hospital without using your car. You can access the information by going to www.traveline.info Alternatively, if you prefer to speak to someone, call 0871 200 22 33. Calls cost 10p per minute (plus network extra if calling from a mobile). Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Site Map Date of issue: 23 June 2011 Page 64 of 144 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 65 of 144 TEST INDEX BACTERIOLOGY TEST SAMPLE & COLLECTION INSTRUCTIONS Adenovirus and Rotavirus Liquid stool in 60ml sterile container Aspirates and fluids 25ml sterile universal container (white top). from normally sterile sites Venous blood is collected aseptically into blood culture bottles. Take Blood cultures before antimicrobials are given if possible. Clean site and bungs of bottle(s) with alcohol wipe and allow to dry before collection. Adult: approx. 5-10ml blood into each bottle. Child: approx. 0.5- 4.0ml blood into one paediatric bottle. Bronchial washings 60ml sterile container or 25ml sterile universal container (white top). 60ml sterile container or 25ml sterile universal container (white top). Broncho-alveolar lavage Cerebrospinal fluid For cell count, gram staining and culture send 0.5 -1mL CSF in each of four 25ml sterile universal containers (white top). If meningitis is (CSF) suspected contact the laboratory and send the specimens immediately. Send specimens 2 and 3 to micro and 1 and 4 to biochemistry for protein (including SAH examination if appropriate). Endocervical swabs are required for gonococcal or chlamydial Cervical swab investigations. For gonorrhoea use a bacterial swab (blue top). Urethral, rectal and throat swabs may also be collected. COMMON INDICATIONS Diarrhoea in children under 3 years TURNAROUND (working days) 2 2 Septicaemia, pneumonia, endocarditis, meningitis, pyrexia. Preliminary report: 2 Full report 6 2 2 Meningitis, subarachnoid haemorrhage (SAH), encephalitis. Pelvic inflammatory disease, vaginal discharge, suspected STD. Microscopy: 0.5 Culture: 2 2 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 66 of 144 TEST SAMPLE & COLLECTION INSTRUCTIONS Chlamydia Males: >20ml urine sample in a 25ml sterile universal container. The patient should not have passed urine in the hour prior to collection or Urethral swab in Chlamydia transport medium. Females: urethral/endocervical swabs in chlamydia transport medium or urine in a 25ml sterile universal container. Clostridium difficile toxin Contact lens and lens fluid Ear swab Eye swab Faeces Hair High vaginal swab COMMON INDICATIONS Pelvic inflammatory disease, urethritis. TURNAROUND (working days) 5 Liquid stool in 60ml sterile container Testing performed on in-patient samples and community patients over 60 years of age ONLY. 25ml sterile universal container (white top) or lens case. Diarrhoea 1 A bacterial swab (blue top). Ear infection, otitis media, otitis externa. Conjunctivitis Diarrhoea, gastroenteritis and outbreaks. 2 Vaginal discharge, SROM. 2 Routine culture: a bacterial swab (blue top). For bacteriology, parasitology and virology: with the wooden spatula provided transfer a grape sized portion or equivalent volume of fluid into a 60ml sterile container. Clostridium difficile toxin detection is only performed on semi solid and liquid samples. Follow up testing is rarely required. Refer to mycology. Collect a swab (blue top) for candida, trichomonas vaginalis, bacterial vaginosis and bacterial pathogens. For PID, chlamydia and gonorrhoea investigations see cervical swab. 14 2 3 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 TEST SAMPLE & COLLECTION INSTRUCTIONS Intrauterine device (IUCD) IV line tips Send in a 60ml sterile container. Joint fluid Legionella antigen Legionella culture (sputum) Mouth swab MRSA screening swabs Mycology Nail Page 67 of 144 Aseptically place the terminal 5-10cm of the tip into a 25ml sterile universal container. For microscopy and culture. Send in a 25ml sterile universal container (white top). Crystals performed by Histopathology. 25ml sterile universal container. Sputum from deep expectoration and not saliva is required. Saliva will not be processed. Collect into a 60ml sterile container. A bacterial swab (blue top). A bacterial swab (blue top). For hospital patients refer to the Hospital Infection Control Policy. For community patients, screening is only normally required for known positive patients prior to elective surgery. For skin, hair and nail clippings use black card or paper. Skin: Scrape skin with a blunt scalpel from the active edge of the lesion. Nail: Cut small pieces of the nail using clippers. Hair: Forceps may be needed to remove body hairs. Infected hair stumps are easily removed by scraping with a scalpel. A bacterial swab (blue top).is used for candida infections. Refer to mycology. COMMON INDICATIONS TURNAROUND (working days) 2 Line infection, septicaemia. Arthritis, infection, gout. 2 Atypical pneumonia Atypical pneumonia. Oral candidiasis. 1 Dermatophyte infections. Microsocopy: 2 Culture: 21 2 5 2 2 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 68 of 144 TEST SAMPLE & COLLECTION INSTRUCTIONS Nasal swab A bacterial swab (blue top). Nasopharyngeal aspirate Pleural fluid Pneumococcal antigen (urine). Pus Traps containing a specimen should be sealed using a loop of tubing alternatively use a 25ml sterile universal. 25ml sterile universal container (white top). 25ml sterile universal container (white top). By prior arrangement with the laboratory. Transfer into a sterile universal container. Only use a bacterial swab in charcoal transport medium when pus cannot be obtained. RSV Saliva testing (for Measles, Mumps and Rubella) Schistosoma parasites (Urine) Nasopharyngeal aspirate into a 60ml sterile container. Please contact the Microbiology laboratory on 01256 313309/13 Sellotape slide Seminal fluid for culture Recommended method: Collect the last few drops of urine from each micturition over a 24 hour period in a plain 25ml sterile universal container. Acceptable alternative: Collect a random specimen ideally between 12.00 and 15.00 hours after light exercise (e.g. 20 rapid knee bends) to maximise the release of eggs. Refer to Threadworm. 25ml sterile universal container (white top). COMMON INDICATIONS Specific organism screen, eg MRSA, Staph aureus. Respiratory tract infection Atypical pneumonia. Infected site Rash (Bilharzia) Travel to endemic area Blood in seminal fluid TURNAROUND (working days) 2 2 2 0.5 2 (culture for anaerobes 5 days) 0.5 Referred specimen 21 Days 1 2 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 69 of 144 TEST SAMPLE & COLLECTION INSTRUCTIONS Sputum Sputum samples are best collected in the morning. It is important that the specimens submitted for examination are true sputum and not saliva, or contaminated with food. Sputum from deep expectoration is required. Saliva will not be processed. Collect into a 60ml sterile container. Collect the sample in the morning before the patient has washed. Press the sellotape onto the peri-anal skin firmly. Remove and stick the sellotape flat onto a clean microscope slide (sticky side down) keeping as flat as possible . Place this in a slide box. For bacterial investigation send a bacterial swab (blue top). Threadworm Throat swab COMMON INDICATIONS Chest infection, pneumonia. TURNAROUND (working days) 2 Anal irritation/itching. 1 Pharyngitis 2 Infected site Virology referred sample 21 Days 7 Night sweats, low grade fever. Renal TB. Microscopy: 1 Culture: up to 40 days For virology investigations send a viral swab (green top) Tissue and biopsies Sterile container. If the sample is small add sterile saline to prevent it drying out. The best samples are early morning sputum, pus or tissue in a 60ml Tuberculosis sterile container. Only collect urine when renal tuberculosis is suspected; collect the complete early morning specimen in 250ml containers on three consecutive days. For the investigation of gonorrhoea use a bacterial (blue top). and Urethral swab transport to the laboratory immediately. For the investigation of Chlamydia use a Chlamydia swab in Chlamydia transport medium. 2 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 70 of 144 TEST SAMPLE & COLLECTION INSTRUCTIONS Urine MSU, CSU, supra pubic aspirate, ileal conduit specimens are all collected into red top 20ml sterile universal containers containing the preservative boric acid (red top). To collect an MSU allow the first part of the urine to be voided. Collect the mid-part of the sample then void the remainder of the specimen. CSU’s are only appropriate when clinical indication of fever, rigors or supra pubic pain are present. CSU’s will NOT be processed without these clinical indications given on the request card. Viral swab (green top) Viral Wound and ulcer swabs COMMON INDICATIONS UTI, haematuria, fever, inflammatory response. TURNAROUND (working days) 1 HSV In-house 5 days PCR tests are now used. Each test is specific for each virus. Please state clinical details and/or virus suspected. Referred specimens 21 days A bacterial swab (blue top). Collect as much material from the infected site as possible avoiding contamination from surrounding areas. Ulcer swabs are only appropriate when signs of severe clinical infections are present. Infection at local site. 2 (culture for anaerobes 5 days) Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 71 of 144 CHEMICAL PATHOLOGY TEST SPECIMEN CONTAINER VOLUME NEEDED SAMPLE TYPE REFERENCE RANGES UNITS SPECIAL PRECAUTIONS KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) 0M-6M 0.8 - 1.8 Alpha 1 Antitrypsin (AAT) 7M-5Y 1.1 - 2.2 Gold Top Vacuette 4mL Serum 6Y-10Y 1.4 - 2.3 g/L 24 HOURS 11Y-15Y 1.2 - 2.0 >16Y 1.1 - 2.1 Angiotensin converting enzyme Gold Top Vacuette 4mL Serum 20 - 95 IU/L (ACE) Acetylcholine receptor Abs Lab Note: SAS -20°C Gold Top Vacuette 4mL Serum 0-5 nmol/L Lab Note: SAS -20°C MGAB Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 10 DAYS Immunology Churchill Hospital Headington Oxford OX3 7LJ 01865 225995 18 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Adrenocorticotrophic Hormone (ACTH) SPECIMEN CONTAINER Lavender Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 3mL SAMPLE TYPE EDTA Plasma Page 72 of 144 REFERENCE RANGES 0 - 40 UNITS ng/L SPECIAL PRECAUTIONS TO LAB AT ONCE - SAMPLE MUST BE FROZEN WITHIN 30 MINUTES Lab Note: SAS -20°C Acylcarnitines KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) Plasma ACTH concentrations may be affected by stress / acute illness and reduced in patients on corticosteroid therapy Specialist Biochemistry Mail Point 8 Level C South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 798717 14 DAYS (see Carnitines) Acetylcholinesterase Lavender Top Vacuette 3mL EDTA Whole Blood >160 dau/L Adrenal antibodies Gold Top Vacuette 4mL Serum _ _ Lab Note: SAS -20°C ADAB Health and Safety Laboratory Harper Hill Buxton Derbyshire SK17 9JN 01298 218099 Sheffield Protein Department of Immunology Protein Reference Unit PO Box 894 Sheffield S5 7YT 01142 715552 14 DAYS 14 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 TEST SPECIMEN CONTAINER Alphafoetoprotein (AFP) Gold Top Vacuette 4mL Serum Auto Immune Profile (AIP) Gold Top Vacuette 4mL Serum Albumin Gold Top Vacuette 4mL Serum Albumin - urine (micro albumin Albumin Creatinine Ratio) Plain (white top) Universal 10 mL Urine Alcohol - blood Gold Top Vacuette 4mL Serum Alcohol - urine Plain (white top)Universal 10mL Urine Aldosterone Lavender Top Vacuette VOLUME NEEDED SAMPLE TYPE Page 73 of 144 REFERENCE RANGES 0 - 10 UNITS SPECIAL PRECAUTIONS KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) Serum AFP levels are raised during pregnancy and in the neonatal patient kU/L TURN – AROUND (working days) 24 HOURS 10 DAYS 32 - 48 g/L 4 HOURS Lab Note: Spin & Rack 3mL EDTA Plasma 0 - 3.0 Legal driving limit < 800 mg/L mg/L mg/L Adult: Supine <160 Ambulant 40 – 310 Aldosterone/ Renin ratio 0 - 25 ng/L 24 HOURS Discuss with Consultant Biochemist Discuss with Consultant Biochemist TO LAB AT ONCE - SAMPLE MUST BE FROZEN WITHIN 30 MINUTES ng/mu Lab Note: SAS -20°C 12 HOURS 12 HOURS Plasma Aldosterone concentrations may be affected by patients’ antihypertension or mineralosteroid drug therapy and may be reduced in patients with hypokalaemia Specialist Biochemistry Mail Point 8 Level C South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 798717 14 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED SAMPLE TYPE Page 74 of 144 REFERENCE RANGES UNITS SPECIAL PRECAUTIONS KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) Children: Alkaline Phosphatase Gold Top Vacuette 4mL Serum 0 - 3yr 145-320 4 - 6yr 150-380 7 - 9yr 175-420 10 -11yr 135-530 12-13yr (M) 200-495 12-13 yr (F) 105-420 14-15yr (M) 130-525 14-15yr (F) 70-230 16-19yr (M) 65-260 16-19yr (F) 50-130 Adult: 20 - 59yr (M) 40 - 105 20 - 59yr(F) 35 - 110 60 - 79yr (M) 40 - 105 60 - 79yr (F) 40 - 115 80 - 89yr (M) 40 - 120 80 - 89yr (F) 40 - 125 >89yr (M) 40 - 140 >89yr (F) 40 - 130 IU/L Alk Phos levels are physically increased in neonates, children, adolescents and pregnancy. In vitro haemolysis will falsely decrease results 4 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST SPECIMEN CONTAINER Alkaline phosphatase - bone see Alk Phos Isoenzyme Alk Phos Isoenzymes Gold Top Vacuette Alpha 1 antitrypsin phenotype Gold Top Vacuette ALT Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED SAMPLE TYPE 4mL Serum 4mL REFERENCE RANGES Page 75 of 144 UNITS SPECIAL PRECAUTIONS Serum Aluminium Gold Top Vacuette 4mL Serum Serum 0 – 12yr 0 - 40 >12yrs 0 - 60 < 0.4 Gold Top Vacuette 4mL Sheffield Protein Department of Immunology Protein Reference Unit PO Box 894 Sheffield S5 7YT 01142 715552 IU/L 14 DAYS 4 HOURS umol/L Lab Note: SAS -20°C Amino acids - serum quantitative TURN – AROUND (working days) 10 DAYS Lab Note: Load tray AND SAS -20°C Lab Note: SAS -20°C 4mL KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) Serum Lab Note: SAS -20°C Trace Metals Unit Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796237 10 DAYS Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 14 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Amino acids urine quantitative SPECIMEN CONTAINER Plain (white top) Universal Date of issue: 23 June 2011 VOLUME NEEDED SAMPLE TYPE REFERENCE RANGES Page 76 of 144 UNITS SPECIAL PRECAUTIONS KEY FACTORS Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 Chemical Pathology Royal Hampshire County Hospital Romsey Rd Winchester SO22 5DG 01962 824287 01962824288 Random sample 20 mL Urine Lab Note: Univ -20ºC Amiodarone Gold Top Vacuette 4mL Serum 0.6 - 2.5 mg/L Lab Note: SAS -20°C Ammonia Lavender Top Vacuette 3mL EDTA Whole blood 0 - 47 3D 0 - 100 umol/L REFERRAL LABORATORY (INC ADDRESS) MUST BE IN LAB WITHIN 30 MINUTES TURN – AROUND (working days) 14 DAYS 14 DAYS 1 HOUR Lab Note:Manual BMS Amniocentesis Plain (white top) Universal 10mL Wessex Regional Genetics Laboratory Salisbury District Hospital Odstock Salisbury SP2 8BJ 01722 429080 Results returned direct to requesting physician Amniotic fluid Lab Note: Univ 4ºC Amylase - serum Gold Top Vacuette Amylase - urine Plain (white top) Universal 4mL Serum 0 - 104 IU/L Urine 0 - 650 IU/L There is assay interference from haemolysis Random sample 21 days Results returned direct to requesting physician 4 HOURS 4 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Amyloid A SPECIMEN CONTAINER Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMPLE TYPE Serum REFERENCE RANGES < 20 Page 77 of 144 UNITS SPECIAL PRECAUTIONS mg/L Lab Note: SAS -20°C Anaphylactic reaction (Serum Tryptase) Androstenedione Anti Mullerian Hormone Antinuclear Antibodies (ANA) Antineutrophil Cytoplasm Antibody (ANCA) Gold Top Vacuette or Lavender Top Vacuette Serum 4mL or 3mL Gold Top Vacuette Gold Top Vacuette 2 - 14 ug/L EDTA Plasma Gold Top Vacuette Gold Top Vacuette or Serum 4mL 4mL Serum TO LAB AT ONCE SAMPLE MUST BE FROZEN WITHIN 30 MINUTES Take first sample at once, repeat at 3 & 24 hrs KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) Sheffield Protein Department of Immunology Protein Reference Unit PO Box 894 Sheffield S5 7YT 01142 715552 14 DAYS Sheffield Protein Department of Immunology Protein Reference Unit PO Box 894 Sheffield S5 7YT 01142 715552 14 DAYS Lab Note : SAS -20ºC M 2.1 - 10.8 F 1.0 - 11.5 nmol/L discuss with Consultant Biochemist 10 DAYS Lab Note : SAS -20ºC Dept of Clinical Biochemistry Macewen Building Glasgow Royal Infirmary Glasgow, G4 0SF 0141 211 4638 Serum 21 DAYS 10 DAYS Lab Note: Imm 4°C ANAE 4mL Serum _ _ Lab Note: SAS 4°C ANCA Southampton Immunology Level C Mailpoint 8 Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 10 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Antinuclear Factor (ANF) Antimitochondrial Antibodies Date of issue: 23 June 2011 SPECIMEN CONTAINER VOLUME NEEDED SAMPLE TYPE Gold Top Vacuette 4mL Serum Gold Top Vacuette 4mL Serum REFERENCE RANGES Page 78 of 144 UNITS SPECIAL PRECAUTIONS KEY FACTORS Lab Note: Imm 4°C ANAE 0-5 Gold Top Vacuette 4mL u/mL Serum Lab Note: SAS - 20°C Asialotransferrin Southampton Immunology Level C Mailpoint 8 Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 10 DAYS Immunology Churchill Hospital Headington Oxford OX3 7LJ 01865 225995 28 DAYS see Beta-2 transferrin AST Serum 0 - 40 aTPO Serum see Thyroid Antibodies Bence Jones Protein TURN – AROUND (working days) 10 DAYS Lab Note: SAS 4°C LIV Aquaporin-4 Antibodies REFERRAL LABORATORY (INC ADDRESS) Plain (white top) Universal In vitro haemolysis will falsely elevate results IU/L 4 HOURS Early morning urine preferred 10mL Urine 10 DAYS Lab Note: White top Vacuette, Advia 2. Univ to Manual Lab Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Beta-2 Microglobulin Beta-2 Transferrin Date of issue: 23 June 2011 Page 79 of 144 SPECIMEN CONTAINER VOLUME NEEDED SAMPLE TYPE REFERENCE RANGES UNITS Gold Top Vacuette 4mL Serum 0.0 -1.7 ug/mL Plain (white top) Universal SPECIAL PRECAUTIONS KEY FACTORS Bile acids Bile Pigments Gold Top Vacuette Gold Top Vacuette Plain (white top) Universal Neuroimmunology Room 917 Institute of Neurology Queen Square London WC1N 3BG 02078 373611 extn 3814 Nasal fluid 14 DAYS 4mL Serum 22 - 31 mmol/L To lab same day 24 HOURS 4mL Serum 0 - 14 umol/L To lab same day 24 HOURS 10 mL Urine 24 HOURS Bilirubin - adult Gold Top Vacuette 4mL Serum 0 - 17 umol/L Bilirubin – direct or conjugated Gold Top Vacuette 4mL Serum 0-3 umol/L Bilirubin paediatric Gold Top Vacuette 4mL Serum 0 - 17 umol/L Bilirubin - urine TURN – AROUND (working days) 14 DAYS Lab Note: Univ 4ºC Bicarbonate REFERRAL LABORATORY (INC ADDRESS) see Bile Pigments Haemolysis will falsely elevate results Haemolysis will falsely elevate results Haemolysis will falsely elevate results 4 HOURS 4 HOURS 4 HOURS 24 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Biotinidase SPECIMEN CONTAINER Green Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMPLE TYPE Plasma Page 80 of 144 REFERENCE RANGES 2.0 – 6.0 UNITS SPECIAL PRECAUTIONS umol /L / min Consultant confirmation required – contact lab Lab Note : SAS -20ºC BNP BJP Bone alkaline phosphatase Bone Turnover B-Type Natriuretic Peptide C Peptide KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) Clinical Biochemistry Bristol Royal Infirmary Marlborough Street BRISTOL BS2 8HW 0117 928 2590 14 DAYS see B-Type Natriuretic Peptide See Bence Jones Protein See Alk Phos Iso enzymes See UDPD Lavender Top Vacuette Gold Top Vacuette plus Grey Top Vacuette 3mL 1 x 4 mL plus 1 x 4 mL EDTA plasma Serum plus Fluoride oxalate plasma for glucose M < 45 F < 45 M 45 - 54 F 45 - 54 M 55 - 64 F 55 - 64 M 65 - 74 F 65 - 74 M 75Y + F 75Y + < 480 0 – 29 0 – 36 0 – 33 0 – 57 0 – 39 0 – 76 0 – 68 0 – 76 0 – 121 0 – 167 pg/mL 10 DAYS To lab same day Note : Centaur-20ºC ug/mL TO LAB AT ONCE SAMPLE MUST BE FROZEN WITHIN 1 HOUR Lab Note: SAS -20°C Lab Note: FLOX to track Specialist Biochemistry Mail Point 8 Level C South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 798717 14 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST C1 esterase inhibitor SPECIMEN CONTAINER Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMPLE TYPE Serum REFERENCE RANGES 0.15 – 0.35 Page 81 of 144 UNITS SPECIAL PRECAUTIONS g/L Lab Note: C 3 & C4 first KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) Not indicated if C4 is within normal limits Southampton Immunology Level C Mailpoint 8 Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 14 DAYS Lab Note: SAS 4°C C3 C4 CA 125 Gold Top Vacuette Gold Top Vacuette Gold Top Vacuette CA 15-3 Gold Top Vacuette CA 19-9 Gold Top Vacuette 4mL Serum 0.9 - 1.5 g/L 24 HOURS 4mL Serum 0.14 - 0.45 g/L 24 HOURS 4mL Serum 0 - 35 kU/L 4mL Serum 0 - 28 levels may be increased during menstruation kU/L Lab Note: SAS -20°C Cadmium - urine Plain (white top) universal 4mL 10mL Serum Urine 0 - 33 < 1.3 24 HOURS Medical Oncology Charing Cross Hospital Fulham Palace Road London W6 8RF 0208 8461468 kU/L 10 DAYS 14 DAYS nmol / mmolCr Lab Note: Univ 4ºC Trace Metals Unit Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796237 14 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Cadmium blood SPECIMEN CONTAINER Lavender top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 3mL SAMPLE TYPE EDTA Whole Blood REFERENCE RANGES < 1.3 Page 82 of 144 UNITS SPECIAL PRECAUTIONS KEY FACTORS nmol/L Lab Note: WB 4ºC Caeruloplasmin Calcitonin Gold Top Vacuette Gold Top Vacuette 4mL 4mL Serum Serum 0 – 4M 0.08 – 0.23 5M – 1Y 0.12 – 0.35 2Y – 10Y 0.20 – 0.40 11Y – 13Y 0.15 – 0.23 >13Y - Adult 0.2 - 0.45 Male 0 - 8.4 Female 0 - 5.0 Gold Top Vacuette 4mL Serum 2.12 - 2.62 TURN – AROUND (working days) Trace Metals Unit Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796237 14 DAYS g/L ng/L 24 HOURS Specialist Biochemistry Mail Point 8 Level C South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 798717 A.M. FASTING TO LAB AT ONCE SAMPLE MUST BE FROZEN IN 20 MINUTES Lab: 2 x SAS -20°C Calcium (as Corrected Calcium) REFERRAL LABORATORY (INC ADDRESS) mmol/L Levels may be artifactually increased by torniquet during venesection 21 DAYS 4 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Calcium – 24hr urine Calcium – random urine Calculus SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED Plain 24h container Plain (white top) universal 4mL Plain (white top) universal Page 83 of 144 SAMPLE TYPE REFERENCE RANGES UNITS Urine (24h) 2.5 - 7.5 mmol/d Urine mmol/L SPECIAL PRECAUTIONS KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) 24 hour collection 24 HOURS Lab: White top vacuette,Advia tray Lab: White top vacuette,Advia tray TURN – AROUND (working days) Measure Creatinine as well 24 HOURS Chemical Pathology Royal Hampshire County Hospital Romsey Rd Winchester SO22 5DG 01962 824287 01962824288 Stone 21 DAYS Lab:Dry,Univ 4ºC Carbamazepine Carbon Monoxide Carboxyhaemoglobin Gold Top Vacuette Sample should be taken pre dose 4mL Serum 3mL EDTA Whole Blood 4.0 - 12.0 mg/L 24 HOURS Smokers may have levels up to and greater than 10% 4 HOURS see Carboxyhaemoglobin Lavender Top Vacuette 1-5 % TO LAB AT ONCE Take sample before oxygen is given Lab Note: Manual BMS Cardiac enzymes If not possible to obtain a pre-dose sample, standardise sample times for comparison purposes See Troponin 4 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Carnitine SPECIMEN CONTAINER Green Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMPLE TYPE Page 84 of 144 REFERENCE RANGES UNITS SPECIAL PRECAUTIONS KEY FACTORS Plasma Lab Note: SAS -20°C Carnitines Blood spot form Catecholamines see VMA Blood spot Do not fold or refrigerate Lab Note: SAS Desk CCP antibodies Gold Top Vacuette Cell-Sept Centromere Gold Top Vacuette see MMF Gold Top Vacuette TURN – AROUND (working days) Clinical Chemistry and Molecular Genetics Children's Hospital Western Bank Sheffield S10 2TH 0114 2717445 4 WEEKS Clinical Chemistry and Molecular Genetics Children's Hospital Western Bank Sheffield S10 2TH 0114 2717445 4 WEEKS 10 DAYS 4mL Serum 0-7 U/mL Lab Note : SAS 4ºC CCP CEA REFERRAL LABORATORY (INC ADDRESS) 4mL 4mL Serum Serum 0-5 _ Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 ug/L 10 DAYS 24 HOURS _ Lab Note: SAS 4°C CENT Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 10 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Chloride VOLUME NEEDED SAMPLE TYPE REFERENCE RANGES UNITS Gold Top Vacuette 4mL Serum 96 - 106 mmol/L Sweat < 40 mmol/L CONTACT LAB TO BOOK APPOINTMENT mmol/L Lab Note: White top vacuette, Advia tray Plain 2mL Tube Chloride - urine Plain (white top) Universal Cholesterol: HDL Ratio Cholinesterase Cholinesterase (for toxicology) Chorionic gonadotrophin Chromogranin A Chromium Page 85 of 144 SPECIMEN CONTAINER Chloride - sweat Cholesterol Date of issue: 23 June 2011 Gold Top Vacuette Gold Top Vacuette see Pseudocholinesterase see Acetylcholinesterase 10mL Urine 4mL Serum < 5.0 4mL Serum < 4.0 SPECIAL PRECAUTIONS TURN – AROUND (working days) 4 HOURS 24 HOURS 4 HOURS mmol/L 4 HOURS 4HOURS 28 DAYS see HCG 24 HOURS see Gut Hormones 5 WEEKS Dark Blue Vacuette 6mL Whole Blood MHRA Action Limit > 135 nmol/L Lab NB: HIP screen Whole Blood 4ºC Chromosomes KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) Green Top Vacuette 4mL Whole Blood Lithium Heparin Results returned direct to requesting physician Lab Note: WB 4ºC Trace Metals Unit Chemical Pathology Level D South Block Southampton Gen Hosp Tremona Road Southampton SO16 6YD 02380 796237 Wessex Regional Genetics Laboratory Salisbury District Hospital Odstock Salisbury SP2 8BJ 01722 429080 14 DAYS 28 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Citrate SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED Acid 24h Bottle SAMPLE TYPE Urine Page 86 of 144 REFERENCE RANGES M 0.6 – 4.8 F 1.3 – 6.0 UNITS SPECIAL PRECAUTIONS 24 hour collection mmol/d Lab Note: Univ 4ºC CK Clobazam Gold Top Vacuette Gold Top Vacuette 4mL 4mL Gold Top Vacuette 4mL TURN – AROUND (working days) Chemical Pathology UCL Hospitals 3rd Floor 60 Whitfield Street London W1T 4EU 0845 1555000 Ext 9405 10 DAYS See Creatine Kinase Serum 4 HOURS < 200 ug/L Lab Note: SAS -20°C Clozapine KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) Serum 0.35 – 0.60 Medical Toxicology Unit 4th Floor North Wing St Thomas’ Hospital London SE1 7EH 02071 888689 Dept. of Clinical Biochemistry Kings College Hospital Denmark Hill London SE5 9RS 020 3299 5881 mg/L 10 DAYS 10 DAYS Lab Note: SAS -20°C Cobalt Dark Blue Vacuette 6mL Whole Blood MHRA Action Limit >120 nmol/L Lab NB: HIP Screen Whole Blood SAS 4ºC Trace Metals Unit Chemical Pathology Level D South Block Southampton Gen Hosp Tremona Road Southampton SO16 6YD 02380 796237 14 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Coeliac screen Coeliac screen (Follow up) Date of issue: 23 June 2011 SPECIMEN CONTAINER VOLUME NEEDED SAMPLE TYPE Gold Top Vacuette 4mL Serum Gold Top Vacuette 4mL Page 87 of 144 REFERENCE RANGES UNITS SPECIAL PRECAUTIONS KEY FACTORS Connective Tissue Antibodies Complement Plain 2mL Tube Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 Serum Gold Top Vacuette Sweat 4mL < 80 mmol/L Serum 24 HOURS Lab Note: ANAE 4°C 10 DAYS see C3 & C4 Trace Metals Unit Chemical Pathology Level D South Block So’ton General Hosp Tremona Road Southampton SO16 6YD 02380 796237 Trace Metals Unit Chemical Pathology Level D South Block So’ton General Hosp Tremona Road Southampton SO16 6YD 02380 796237 Dark Blue Vacuette 6mL Plasma 12 – 26 umol/L Lab NB: Teklab -20ºC Li Hep may be used for Paeds Copper - urine 24 hour collection Plain 24h bottle Urine < 0.9 umol/d Lab Note: Univ 4ºC Cortisol serum 21 DAYS CONTACT LAB TO BOOK APPOINTMENT Must be bled in Phlebotomy Copper serum TURN – AROUND (working days) 10 DAYS Lab Note: COEL 4°C Lab Note: if positive SAS 4°C Conductivity REFERRAL LABORATORY (INC ADDRESS) Gold Top Vacuette 4mL Serum 119 – 619 nmol/L Levels may be affected by stress, diurnal rhythm and corticosteroid therapy 14 DAYS 14 DAYS 24 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Cortisol urine SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED Plain 24h bottle SAMPLE TYPE Urine Page 88 of 144 REFERENCE RANGES 55 - 250 UNITS SPECIAL PRECAUTIONS nmol/d KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) Levels may be affected by stress and corticosteroid therapy Chemical Pathology West Park Hospital Epsom Surrey KT19 8PB 01372 734724 10 DAYS Dept of Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 10 DAYS Lab Note: Univ 4ºC Cotinine Plain (white top) Universal 10mL Urine Lab Note: Univ -20ºC CPK Creatine kinase See Creatine Kinase Gold Top Vacuette Creatinine Gold Top Vacuette Creatinine Plain 24h bottle 0 -1mth 0 - 244 2mth-15Y 0-220 4mL Serum IU/L Strong interference from haemolysis 4 HOURS umol/L Adult males with increased muscle mass may have slightly elevated serum concentrations without underlying renal pathology 4 HOURS Adult M 0 – 195 Adult F 0 – 170 4mL Serum Urine <2 days 2d - 30d 1m – 1y 2y - 12y 13y - 16y 17y – 18y >18y(adult) 40 - 100 40 - 80 30 - 60 30 - 80 40 - 120 40 - 120 62 - 124 9 - 27 mmol/d Lab Note: White top universal 24 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Creatinine Clearance SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED Plain 24h bottle SAMPLE TYPE REFERENCE RANGES UNITS SPECIAL PRECAUTIONS Urine 90 - 120 mLs/min Serum sample also needed 0-5 mg/L KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) 24 HOURS See UDPD Cross Links CRP Page 89 of 144 Gold Top Vacuette Cryoglobulins Gold Top Vacuette & Lavender Top Vacuette CSF Protein Plain (white top) universal 4mL 4mL & 3mL Serum 4 HOURS COLLECT WARMED TUBES IN WARMED FLASK FROM LAB. IMMEDIATELY TAKE SAMPLES. RETURN SAMPLES TO LAB IN FLASK IMMEDIATELY. Serum & EDTA Plasma May be referred as follow up to in-house findings Protein Reference Unit 2nd Floor, Jenner Wing St George's Hospital Medical School Cranmer Terrace LONDON SW17 0NH 02087250025 4 DAYS or 21days if referred Lab NB: Manual BMS Cyclosporin A: Lavender Top Vacuette 1mL 3mL CSF EDTA Whole blood 0.1 - 0.4 g/L 4 HOURS ug/L Lab Note: WB 4ºC Cystic fibrosis gene screen C-reactive protein Lavender Top Vacuette 3mL EDTA Whole Blood see CRP Results returned direct to requesting physician Lab Note: WB 4ºC Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 Wessex Regional Genetics Laboratoy Salisbury District Hospital Odstock Salisbury SP2 8BJ 01722 429080 7 DAYS 6 WEEKS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Dehydrocholesterol SPECIMEN CONTAINER Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMPLE TYPE Page 90 of 144 REFERENCE RANGES UNITS SPECIAL PRECAUTIONS Serum Lab Note: SAS -20°C Desmethylclobazam Gold Top Vacuette 4mL Serum < 2000 ug/L Lab Note: SAS -20°C 0 – 30d 1m – 5m 6m – 5y 6y – 9y 10y – 39y 40y – 59y >60y Female 0 – 30d 1m – 5m 6m – 5y 6y – 9y 10y – 39y 40y – 59y >60y Male DHEAS: Gold Top Vacuette 4mL Serum 1.0 – 10.2 0.1 – 2.8 0.1 – 2.2 0.2 – 2.7 3.3 – 17.4 1.9 – 14.4 0.8 – 7.9 1.0 – 10.2 0.1 – 2.8 0.1 – 2.2 0.2 – 2.7 1.0 – 11.7 1.0 – 11.7 0.8 – 7.0 umol/L KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) Newborn Screening & Biochemical Genetics Dept Southmead Hospital Westbury-on-Trym Bristol BS10 5NB 0117 3235556 Medical Toxicology Lab 3rd Floor, Block 7 South Wing St Thomas’ Hospital London SE1 7EH 02071 888689 TURN – AROUND (working days) 5 WEEKS 10 DAYS 14 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Diuretic screen SPECIMEN CONTAINER Plain (white top) Universal Date of issue: 23 June 2011 VOLUME NEEDED 10mL SAMPLE TYPE Page 91 of 144 REFERENCE RANGES UNITS SPECIAL PRECAUTIONS Urine Lab Note: Univ 4ºC Digoxin DNA antibodies DNA binding DNA Genetics Gold Top Vacuette Gold Top Vacuette Gold Top Vacuette Lavender Top Vacuette 4mL 4mL 4mL 3mL Serum Serum 0.6 - 2.0 0 – 15 ug/L Gold Top Vacuette 4mL 14 DAYS 24 HOURS 10 DAYS Lab Note: SAS 4°C DNA 10 DAYS Lab Note: SAS 4°C DNA Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 Wessex Regional Genetics Laboratory Salisbury District Hospital Odstock Salisbury SP2 8BJ 01722 429080 6 WEEKS Results returned direct to requesting physician Serum Serum Regional Laboratory for Toxicology Dudley Road Winson Green Birmingham B18 7QH 0121 507 6029 Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 Results returned direct to requesting physician Lab Note: WB 4ºC Dothiepin TURN – AROUND (working days) Take sample 6 Hours post dose iu/mL EDTA Whole Blood KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) ug/L Lab Note: SAS -20°C Contact Consultatnt Biochemsit Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Down's Syndrome Drugs of abuse screen Effusion screen eGFR: Kidney Damage Stage 1 Kidney Damage Stage 2 Kidney Damage Stage 3 Kidney Damage Stage 4 Kidney Damage Stage 5 Elastase SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED SAMPLE TYPE Page 92 of 144 REFERENCE RANGES UNITS SPECIAL PRECAUTIONS KEY FACTORS TURN – AROUND (working days) See Triple Test Plain (white top) Universal Plain (white top) Universal 10mL Urine 10 DAYS 4mL Effusion 4 HOURS 90+ 60-89 Serum 30-59 mLs/min calculated 15-29 Multiply result by 1.212 for AfroCaribbean patients. See local guidelines for interpretation of results. 4 HOURS < 15 Plain (orange top) specimen pot Faeces > 200 Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 ug/g Lab Note: -20ºC Electrolytes serum REFERRAL LABORATORY (INC ADDRESS) Gold Top Vacuette 4mL Serum Na K Urea Creat 134 - 147 3.5 - 5.0 2.6 - 6.0 62 -124 mmol/L Potassium levels are significantly increased by invitro haemolysis and delayed sample centrifugation. Levels may also be significantly raised in patients with high platelet count 10 DAYS 4 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 TEST SPECIMEN CONTAINER Electrolytes urine Plain 24h bottle or Plain (white top) Universal for Random sample 10mL Electrophoresis Gold Top Vacuette 4mL Serum Electrophoresis - urine Plain (white top) Universal 10mL Urine Extractable Nuclear Antibodies (ENA) Gold Top Vacuette Endomyseal antibodies Epanutin see Coeliac screen see Phenytoin Epidermal antibodies VOLUME NEEDED 4mL Page 93 of 144 SAMPLE TYPE REFERENCE RANGES Urine Na 130 – 220 K 25 – 100 Urea 199 - 332 Serum UNITS SPECIAL PRECAUTIONS mmol/d 24 HOURS Lab: White top vacuette,Advia tray Serum only see Valproate 5 DAYS 5 DAYS NEGATIVE Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 10 DAYS Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 10 DAYS Lab Note: COEL 4°C 4mL Serum Lab Note: SAS 4°C PEMP Epilim TURN – AROUND (working days) 24 h collection Lab Note : SAS 4ºC ENAS Gold Top Vacuette KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Erythropoietin SPECIMEN CONTAINER Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMPLE TYPE Serum Page 94 of 144 REFERENCE RANGES 5.0 - 25.0 UNITS SPECIAL PRECAUTIONS mu/mL Lab Note: SAS -20°C Everolimus Executive screen Ferritin Flecainide FOB Folate Free light chains: Kappa Lambda Ratio Lavender Top Vacuette Gold Top Vacuette Gold Top Vacuette Gold Top Vacuette see Occult blood Gold Top Vacuette Gold Top Vacuette 3mL EDTA Whole Blood 4mL Serum 4mL Serum ng/mL Lab Note: WB 4ºC KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) Department of Clinical Biochemistry King's College School of Medicine Denmark Hill London SE5 9RS 020 3299 3856 Analytical Unit St. Georges Hospital London SW17 0RE 0208 725 5345 TURN – AROUND (working days) 14 DAYS 10 Days 4 HOURS 22 - 332 ug/L 3 DAYS Analytical Unit St. Georges Hospital London SW17 0RE 0208 725 5345 4mL Serum 400 - 700 ug/L 4mL Serum 2.9 - 16.9 ug/L 3 DAYS Serum (Diagnostic Range) 3.3 - 19.4 5.7 - 26.3 0.26 - 1.65 mg/L 10 DAYS 4mL Lab Note : SAS -20ºC 14 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED SAMPLE TYPE Page 95 of 144 REFERENCE RANGES 10-18% Low diagnostic value Free PSA Free PSA % Gold Top Vacuette 4mL Serum <10% Higher risk UNITS SPECIAL PRECAUTIONS KEY FACTORS ug/L % Lab Note : SAS -20ºC REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) Medical Oncology Charing Cross Hospital Fulham Palace Road London W6 8RF 0208 8461468 10 DAYS >18% Lower risk Free Fatty Acids Grey top Vacuette 4mL Clinical Chemistry and Molecular Genetics Children's Hospital Western Bank Sheffield S10 2TH 0114 2717445 Clinical Biochemistry Royal United Hospital Area Central Laboratory Combe Park Bath BA1 3NG 01225 824711 TO LAB AT ONCE - SAMPLE MUST BE FROZEN IN 20 MINUTES Fluoride Oxalate plasma Lab Note : SAS -20ºC Fructosamine Gold Top Vacuette 4mL Serum 205 - 285 umol/L Lab Note : SAS -20ºC 21 DAYS 14 DAYS FSH <8.0 Pre pubertal 1.4 - 11.0 Male Female: Follicular Mid cycle Luteal Post Menopausal Post GnRH at 20 minutes Gold Top Vacuette 4mL Serum Follicular 2.5 - 10.2 Mid cycle 3.4 - 33.4 Luteal 1.5 - 9.1 Post m’pause 23 – 116 FSH rises by 100 - 200% IU/L Levels are reduced in patients on HRT / oral contraceptive and during pregnancy. Early follicular phase FSH levels above 15IU/L suggestive of perimenopausal transition 72 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 96 of 144 TEST SPECIMEN CONTAINER VOLUME NEEDED SAMPLE TYPE REFERENCE RANGES UNITS FT3 Gold Top Vacuette 4mL Serum 3.5 - 6.5 pmol/L FT4 Gold Top Vacuette 4mL Serum 10 - 19 pmol/L GAD antibodies Galactitol Gold Top Vacuette Plain (white top) Universal 4mL Serum <1 SPECIAL PRECAUTIONS KEY FACTORS Levels may be reduced in nonthyroidal illness Levels may be reduced in nonthyroidal illness u/mL Urine Lab Note: Univ 4ºC Galactosaemia - enzyme studies Green Top Vacuette Galactosaemia - enzyme studies Blood Spot card 4mL Lithium Heparin – Whole blood Lab Note: SAS 4°C Blood spot Lab Note: SAS Desk Galactose 1 phosphate Green Top Vacuette 4mL Lithium Heparin – Whole Blood Lab Note : SAS 4ºC Results may be affected by recent blood transfusions TURN – AROUND (working days) 24 HOURS 24 HOURS Sheffield Protein Department of Immunology Protein Reference Unit PO Box 894 Sheffield S5 7YT 01142 715552 Lab Note: SAS -20°C GAD 10mL REFERRAL LABORATORY (INC ADDRESS) Newborn Screening & Biochemical Genetics Southmead Hospital Westbury-on-Trym Bristol BS10 5NB 0117 3235556 Newborn Screening & Biochemical Genetics Southmead Hospital Westbury-on-Trym Bristol BS10 5NB 0117 3235556 Newborn Screening & Biochemical Genetics Southmead Hospital Westbury-on-Trym Bristol BS10 5NB 0117 3235556 Newborn Screening & Biochemical Genetics Southmead Hospital Westbury-on-Trym Bristol BS10 5NB 0117 3235556 14 DAYS 21 DAYS 5 WEEKS 10 DAYS 5 WEEKS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST SPECIMEN CONTAINER Gammaglutamyl transpeptidase see GGT Ganglioside antibodies Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED SAMPLE TYPE Page 97 of 144 REFERENCE RANGES UNITS SPECIAL PRECAUTIONS KEY FACTORS Gold Top Vacuette 4mL Neuroimmunology Room 917 Institute of Neurology Queen Square London WC1N 3BG 02078 373611 extn 3814 Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 Serum 4mL Serum _ _ Lab Note: SAS 4°C GPCA Gastrin GAWK GBM antibodies GGT GH Gliadin antibodies 4 WEEKS 10 DAYS see Gut Hormones see Gut Hormones Gold Top Vacuette 4mL Serum Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 0 – 7.0 Lab Note: SAS 4°C GBM Gentamycin TURN – AROUND (working days) 4 HOURS Lab Note: SAS -20°C GANG Gastric parietal cell Abs REFERRAL LABORATORY (INC ADDRESS) Gold Top Vacuette Gold Top Vacuette see Growth hormone see Coeliac screen 4mL Serum 4mL Serum 24 HOURS mg/L M 0 - 60 F 0 - 40 10 DAYS IU/L May be affected by invitro haemolyis Lab Note: SAS 4°C COEL 4 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 98 of 144 TURN – AROUND (working days) TEST VOLUME NEEDED SAMPLE TYPE REFERENCE RANGES UNITS Globulin Gold Top Vacuette 4mL Serum 23 - 40 g/L 4 HOURS 60% Plasma level mmol/L 4 HOURS Glomerular basement membrane Abs see GBM Glucagon see Gut Hormones Glucose - CSF Glucose - fluid Glucose - plasma Grey top Vacuette Grey Top Vacuette Grey Top Vacuette 0.5mL CSF 4mL Fluoride oxalate plasma 4 HOURS 3.8 - 6.0 Fasting: <6.0 2h post: <7.8 Impaired fasting glycaemia Fasting: 6.1-6.9 2h post: <7.8 Impaired glucose tolerance Diabetic Post 50g load in pregnancy KEY FACTORS Fluid OGTT (Oral Glucose Tolerance Test) post 75g load Grey Top Vacuette SPECIAL PRECAUTIONS REFERRAL LABORATORY (INC ADDRESS) SPECIMEN CONTAINER 4mL Fluoride oxalate plasma Fasting: <7.0 2h post:7.8-11.1 Fasting: >7.0 and/or 2h post: >11.1 Fasting: <6.0 2h post: <7.8 mmol/L mmol/L Patient should be fasting 4 HOURS 24 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 99 of 144 TEST SPECIMEN CONTAINER VOLUME NEEDED SAMPLE TYPE REFERENCE RANGES Glucose serum (BNHFT) Gold Top Vacuette 4mL Serum 3.8 - 6.0 Glycated haemoglobin Glycosamino glycans Growth hormone UNITS SPECIAL PRECAUTIONS KEY FACTORS mmol/L Sample MUST be in lab within 2 hours Patient should be fasting Gut Hormones Gastrin GAWK Glucagon Somatostatin Pancreatic Polypeptide Vaso. Int. Pep Chromogranin A TURN – AROUND (working days) 4 HOURS see HbA1 24 HOURS see Mucopolysaccharides Gold Top Vacuette 4mL Serum <5 mu/L TO LAB AT ONCE - SAMPLE MUST BE FROZEN IN 1 HOUR Lab Note: SAS -20°C GTT (Glucose Tolerance Test) REFERRAL LABORATORY (INC ADDRESS) Two Grey Top Vacuettes Large Pink Top Vacuette 2 x 4mL Timed 6 mL Fluoride Oxalate EDTA Plasma Two samples: Fasting and 2h post oral glucose contact lab to make an appointment see glucose 0 - 40 0 -150 0 - 50 0 - 150 0 - 300 1.5 - 4.2 < 60 levels may be increased by stress or exercise Specialist Biochemistry Mail Point 8 Level C South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 798717 pmol/L SAMPLES MUST BE COLLECTED FASTING . TRANSFER TO LAB IMMEDIATELY Lab Note: 2 x SAS -20°C 14 DAYS 24 HOURS Medical Oncology Dept. Charing Cross Hospital Fulham Palace Road London W6 8RF 0208 846 1468 Via Hammersmith Hospital 02083833949 28 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Haptoglobin SPECIMEN CONTAINER Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMPLE TYPE Serum Page 100 of 144 REFERENCE RANGES Male 0.5 – 2.0 Female 0.4– 1.6 UNITS SPECIAL PRECAUTIONS KEY FACTORS g/L Lab Note: SAS -20°C HbA1 HCG 2d - 1w 8d - 2w 15d - 3w 22d - 4w 29d - 5w 36d - 6w 7w - 8w 9w - 3m Lavender Top Vacuette Gold Top Vacuette 3mL 4mL HCGx Gold Top Vacuette 4mL HDLcholesterol Gold Top Vacuette 4mL Heart muscle antibodies EDTA Whole Blood Serum Serum 6.5 - 7.5 % 48 - 59 mmol/mol <5 5 - 50 50 - 500 100 - 5000 500 - 10000 1000 - 50000 10000 - 100000 15000 - 200000 10000 - 100000 IU/L 0-4 Male >1.0 Female >1.2 TURN – AROUND (working days) Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 10 DAYS levels may be affected in patients with Hb variants or altered red cell turnover 48 HOURS 24 HOURS pregnancy IU/L Male patients Lab Note : SAS -20ºC Serum REFERRAL LABORATORY (INC ADDRESS) Medical Oncology Charing Cross Hospital Fulham Palace Road London W6 8RF 0208 8461468 mmol/L 14 DAYS 4 HOURS Lab Note: SAS -20°C HMAB Sheffield Protein Department of Immunology Protein Reference Unit PO Box 894 Sheffield S5 7YT 01142 715552 14 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Haemochromatosis (HFE Gene) SPECIMEN CONTAINER Lavender Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 3mL SAMPLE TYPE Page 101 of 144 REFERENCE RANGES UNITS SPECIAL PRECAUTIONS Results returned direct to requesting physician EDTA Whole Blood Lab Note: WB 4ºC Histone antibodies Gold Top Vacuette 4mL Serum 0-5 u/mL Lab Note : SAS -20ºC ANAE 24 hour collection 5HIAA 24 hr Acidified 24h bottle Urine 5 - 35 umol/d Lab Note: Univ 4ºC HLA antibodies HLA A,B,C phenotype Red Top Vacuette + Pink Top Vacuette Pink Top Vacuette 4mL + 6mL 3 x 6mL Plain Whole Blood + EDTA WB EDTA Whole Blood Results returned direct to requesting physician Lab Note: WB 4ºC Results returned direct to requesting physician Lab Note: WB 4ºC KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) Wessex Regional Genetics Lab Salisbury District Hospital Odstock Salisbury SP2 8BJ 01722 429080 Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 H&I Laboratory National Blood Service South Thames Centre 75 Cranmer Terrace Tooting London WS17 0RB 0208 258300 H&I Laboratory National Blood Service South Thames Centre 75 Cranmer Terrace Tooting London WS17 0RB 0208 258301 TURN – AROUND (working days) 6 WEEKS Results returned direct to requesting physician 8 WEEKS 10 DAYS Results returned direct to requesting physician Results returned direct to requesting physician Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST HLA B27 SPECIMEN CONTAINER PinkTop Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 6mL SAMPLE TYPE EDTA Whole Blood REFERENCE RANGES Page 102 of 144 UNITS SPECIAL PRECAUTIONS Results returned direct to requesting physician Lab Note: WB 4ºC HLA DP Pink Top Vacuette 6mL EDTA Whole Blood Results returned direct to requesting physician Lab Note: WB 4ºC HLA DR,DQ Pink Top Vacuette 3 x 6mL EDTA Whole Blood Results returned direct to requesting physician Lab Note: WB 4ºC Homovanillic acid H&I Laboratory National Blood Service South Thames Centre 75 Cranmer Terrace Tooting London WS17 0RB 0208 258302 H&I Laboratory National Blood Service South Thames Centre 75 Cranmer Terrace Tooting London WS17 0RB 0208 258303 H&I Laboratory National Blood Service South Thames Centre 75 Cranmer Terrace Tooting London WS17 0RB 0208 258304 TURN – AROUND (working days) Results returned direct to requesting physician Results returned direct to requesting physician Results returned direct to requesting physician see VMA Hormone Profile Gold Top Vacuette Hu antibodies see Purkinje HVA See VMA Hydroxybutyrate KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) Grey Top Vacuette 4mL Serum 72 HOURS Lab Note: SAS -20°C NEUR 4mL Fluoride Oxalate Plasma TO LAB AT ONCE SAMPLE MUST BE FROZEN IN 20 MINUTES Lab Note : SAS -20ºC Clinical Chemistry and Molecular Genetics Childrens Hospital Western Bank Sheffield S10 2TH 0114 271 7445 21 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Hydroxy carbamazepine SPECIMEN CONTAINER Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMPLE TYPE Serum Page 103 of 144 REFERENCE RANGES 15 - 35 UNITS SPECIAL PRECAUTIONS mg/L Lab Note: SAS -20°C 18 Hydroxycortisol Gold Top Vacuette 4mL Serum 1.6 - 10.7 (Ambulant) nmol/L Lab Note: SAS -20°C 17 Hydroxy progesterone Blood Spot card Blood spot Lab Note: SAS Desk 17 Hydroxy – progesterone Gold Top Vacuette 4mL Serum <5 days 0 – 30 >5 days 0 - 14 nmol/L Lab Note: SAS -20°C KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) Medical Toxicology Unit 4th Floor North Wing St Thomas’ Hospital London SE1 7EH 02071 888689 Specialist Biochemistry Mail Pint 8 Level C South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 798717 Specialist Biochemistry Mail Pont 8 Level C South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 798717 Specialist Biochemistry Mail Pint 8 Level C South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 798717 TURN – AROUND (working days) 10 DAYS 10 DAYS 21 DAYS 21 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST IgA: cord blood 0 – 14days 2 - 6wks 7 - 11wks 3 - 6mths 7 - 9mths 10mths – 1yr 2yrs 3yrs 4 - 6yrs 7 - 9yrs 10 - 12yrs 13 - 15yrs 16 - 45yrs >45yrs IgD SPECIMEN CONTAINER Gold Top Vacuette Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL 4mL SAMPLE TYPE Serum Serum Page 104 of 144 REFERENCE RANGES <0.02 0.01 - 0.08 0.02 - 0.15 0.05 - 0.4 0.1 - 0.5 0.15 - 0.7 0.2 - 0.7 0.3 - 1.2 0.3 - 1.3 0.4 - 2.0 0.5 - 2.4 0.7 - 2.5 0.8 - 2.8 0.8 - 2.8 0.8 - 4.0 2 - 100 UNITS SPECIAL PRECAUTIONS g/L Gold Top Vacuette 4mL Serum 0 - 11 0 - 29 0 - 43 0 - 52 0 - 56 0 - 63 0 - 65 0 - 70 0 - 81 kU/L IU/L TURN – AROUND (working days) 24 HOURS Lab Note: SAS -20°C IgE: 0 – 12mths 1y 2 - 3y 4 - 5y 6 - 7y 8 - 10y 11 - 12y 13 - 14y >15y KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) Sheffield Protein Department of Immunology Protein Reference Unit PO Box 894 Sheffield S5 7YT 01142 715552 21 DAYS 24 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST IGF1 SPECIMEN CONTAINER Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMPLE TYPE Serum Page 105 of 144 REFERENCE RANGES Age related reference ranges apply UNITS ug/L SPECIAL PRECAUTIONS TO LAB AT ONCE - SAMPLE MUST BE FROZEN IN 30 MINUTES Lab Note: SAS -20°C IGF2 Green Top Vacuette 4mL Plasma nmol/L Discuss with Consultant Biochemist Lab Note: SAS -20°C IGFBP3 Gold Top Vacuette 4mL Serum 0.7 – 4.4 mg/L Lab Note: SAS -20°C KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) Specialist Biochemistry Mail Pont 8 Level C South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 798717 14 DAYS Peptide Laboratory Royal Surrey County Hospital Egerton Rd Guildford GU2 5XX 01483 406715 Peptide Laboratory Royal Surrey County Hospital Egerton Rd Guildford GU2 5XX 01483 406715 14 DAYS 14 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED SAMPLE TYPE Page 106 of 144 REFERENCE RANGES UNITS SPECIAL PRECAUTIONS KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) IgG cord blood 0 – 14days 2 - 6wks 7 - 11wks 3 - 6mths 7 - 9mths 10mths – 1yr 2yrs 3yrs 4 - 6yrs 7 - 9yrs 10 - 12yrs 13 - 15yrs 16 - 45yrs >45yrs IgG subclasses Gold Top Vacuette 4mL Serum Gold Top Vacuette 4mL Serum 5.2 - 18.0 5.0 - 17.0 3.9 - 13.0 2.1 - 7.7 2.4 - 8.8 3.0 - 9.0 3.0 - 10.9 3.1 - 13.8 3.7 - 15.8 4.9 - 16.1 5.4 - 16.1 5.4 - 16.1 5.4 - 16.1 6.0 - 16.0 6.0 - 16.0 g/L 24 HOURS 10 DAYS IgG1 cord blood <5mths 5m – 1yr 2 – 4yrs 5 – 9yrs 10 – 14yrs >15yrs (adult) IgG2 cord blood <5mths 5m – 1yr 2 – 4yrs 5 – 9yrs 10 – 14yrs >15yrs (adult) Gold Top Vacuette 4mL Serum 3.6 - 8.4 1.5 - 3.0 2.3 - 5.8 2.3 - 6.4 3.6 - 7.3 3.8 - 7.7 3.2 - 10.2 1.2 - 4.0 0.3 - 0.5 0.3 - 2.9 0.7 - 4.5 1.4 - 4.5 1.3 - 4.6 1.2 - 6.6 g/L Lab Note: SAS -20°C Lab Note: SAS -20°C Protein Reference Unit 2nd Floor, Jenner Wing St George's Hospital Medical School Cranmer Terrace LONDON SW17 0NH 02087250025 14 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED SAMPLE TYPE Page 107 of 144 REFERENCE RANGES UNITS SPECIAL PRECAUTIONS IgG3 cord blood <5mths 5m – 1yr 2 – 4yrs 5 – 9yrs 10 – 14yrs >15yrs (adult) Gold Top Vacuette 4mL Serum 0.3 - 1.5 0.1 - 0.6 0.1 - 0.8 0.1 - 1.1 0.3 - 1.1 0.2 - 1.2 0.2 - 1.9 g/L Lab Note: SAS -20°C KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) Protein Reference Unit 2nd Floor, Jenner Wing St George's Hospital Medical School Cranmer Terrace LONDON SW17 0NH 02087250025 28 DAYS Protein Reference Unit 2nd Floor, Jenner Wing St George's Hospital Medical School Cranmer Terrace LONDON SW17 0NH 02087250025 28 DAYS IgG4 cord blood <5mths 5m – 1yr 2 – 4yrs 5 – 9yrs 10 – 14yrs Gold Top Vacuette 4mL Serum >15yrs (adult) 0 - 0.5 0 - 0.1 0 - 0.5 0 - 0.8 0 - 1.2 0 - 1.1 g/L Lab Note: SAS -20°C 0 - 1.3 IgM cord blood 0 – 14days 2 - 6wks 7 - 11wks 3 - 6mths 7 - 9mths 10mths – 1yr 2yrs 3yrs 4 - 6yrs 7 - 9yrs 10 - 12yrs 13 - 15yrs 16 - 45yrs >45yrs Igs Gold Top Vacuette Gold Top Vacuette 4mL Serum Serum 0.02 - 0.2 0.05 - 2.0 0.08 - 0.4 0.15 - 0.7 0.2 - 1.0 0.4 - 1.6 0.6 - 2.1 0.5 - 2.2 0.5 - 2.2 0.5 - 2.0 0.5 - 1.8 0.5 - 1.8 0.5 - 1.9 0.5 - 1.9 0.5 - 2.0 g/L g/L 4 HOURS 4 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Immunoglobulins Indirect immunofluorescence Inhibin B Insulin SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED SAMPLE TYPE Insulin like growth factor 1 REFERENCE RANGES UNITS SPECIAL PRECAUTIONS KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) Medical Oncology Charing Cross Hospital Fulham Palace Road London W6 8RF 0208 8461468 28 DAYS Specialist Biochemistry Mail Pint 8 Level C South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 798717 18 DAYS Sheffield Protein Department of Immunology Protein Reference Unit PO Box 894 Sheffield S5 7YT 01142 715552 10 DAYS see Igs Lab Note: SAS 4°C PEMP see Epidermal antibodies Gold Top Vacuette Gold Top Vacuette and Grey Top Vacuette 4mL Serum Male 25 - 325; Female <341, Day 3 of cycle <273, Post menopause <5 2 x 4mL and Fluoride Oxalate Plasma < 10 see IGF1 Lab Note: SAS -20°C 4mL Serum mu/L TO LAB AT ONCE SAMPLE MUST BE FROZEN WITHIN 1 HOUR Lab: Serum SAS -20°C Lab Note: FLOX to track > 0.25 Gold Top Vacuette ng/L Serum Glucose / Insulin Ratio Insulin antibodies Page 108 of 144 _ Patient MUST be fasting mmol/mu _ Lab Note: SAS -20°C INSA Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Intrinsic factor antibodies SPECIMEN CONTAINER Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMPLE TYPE Serum Page 109 of 144 REFERENCE RANGES 0 - 6.0 UNITS SPECIAL PRECAUTIONS KEY FACTORS u/mL Lab Note: SAS 4°C IFAB Iron Gold Top Vacuette 4mL Serum M 14.3 - 28.6 F 12.5 - 25.0 Plain 24h bottle Urine 0.2 – 1.0 umol/L umol/d Lab Note: Univ 4ºC Islet cell antibodies Gold Top Vacuette Jo-1 antibodies see AIP K see Potassium 4mL Serum 0 - 100 TURN – AROUND (working days) Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 18 DAYS Levels are artefactually increased by in vitro haemolysis 24 hour collection Iron - urine REFERRAL LABORATORY (INC ADDRESS) IU/L Lab Note: SAS -20°C ICAB 4 HOURS Trace Metals Unit Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796237 Sheffield Protein Department of Immunology Protein Reference Unit PO Box 894 Sheffield S5 7YT 01142 715552 10 DAYS 14 DAYS Lab Note: SAS 4°C ANAE 4 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Karyotype SPECIMEN CONTAINER Green Top Vacutte La antibodies see ENA Lactate Grey Top Vacuette Lactate dehydrogenase see LDH Lamotrigine Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL 4mL SAMPLE TYPE Page 110 of 144 REFERENCE RANGES UNITS Lithium Heparin Whole Blood Fluoride Oxalate Plasma SPECIAL PRECAUTIONS Lab Note: WB 4ºC 0.6 - 2.4 1 Day 0.0 - 3.7 2 Days 0.0 - 2.7 mmol/L KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) Results returned direct to requesting physician Wessex Regional Genetics Laboratory Salisbury District Hospital Odstock Salisbury SP2 8BJ 01722 429080 28 DAYS TO LAB AT ONCE 24 HOURS Lab NB: Advia BMS 4 HOURS 4mL Serum 1 - 15 Medical Toxicology Unit 4th Floor North Wing St Thomas’ Hospital London SE1 7EH 02071 888689 Chemical Pathology West Park Hospital Epsom Surrey KT19 8PB 01372 734724 mg/L Lab Note: SAS -20°C Laxative screen Plain (white top) Universal 3 x 10mL Take 3 samples over 3 consecutive days Urine Lab Note: Univ -20ºC LDH LDL LE Screen (SLE Screen) Gold Top Vacuette Gold Top Vacuette Gold Top Vacuette 4mL Serum 230 - 460 IU/L 4mL Serum < 3.0 mmol/L 4mL Serum Levels are reduced in patients on hrt/ocp and during pregnancy 10 DAYS 28 DAYS 4 HOURS Fasting sample 4 HOURS Lab Note: 4°C ANAE 10 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Lead SPECIMEN CONTAINER Lavender Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 3mL SAMPLE TYPE EDTA Whole blood Page 111 of 144 REFERENCE RANGES < 0.5 UNITS SPECIAL PRECAUTIONS umol/L Lab Note: WB 4ºC Levetiracetam LFT LH: Pre pubertal Male Female: Follicular Mid cycle Luteal post menopausal Gold Top Vacuette Gold Top Vacuette 4mL Serum Lab Note: SAS 20°C 4mL Serum REFERRAL LABORATORY (INC ADDRESS) Trace Metals Unit Dept of Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796237 Medical Toxicology Unit 4th Floor North Wing St Thomas’ Hospital London SE1 7EH 02071 888689 TURN – AROUND (working days) 14 DAYS 10 DAYS g/L IU/L IU/L Umol/L 4 HOURS IU/L 72 HOURS <2.0 1.5 - 9.3 Gold Top Vacuette 4mL Serum post GnRH at 20 mins Lipids ALB 32-48 ALP 35 -140 ALT 0 - 49 BILI 0 - 17 KEY FACTORS 1.9 - 12.5 8.7 - 76.3 0.5 - 16.9 15.9 - 54.0 LH rises by 400 - 800% Gold Top Vacuette 4mL Serum see cholesterol, triglyceride, HDL & LDL 4 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 112 of 144 TEST SPECIMEN CONTAINER VOLUME NEEDED SAMPLE TYPE REFERENCE RANGES UNITS Lithium Gold Top Vacuette 4mL Serum 0.4 - 1.2 mmol/L Liver Antibody Screen Gold Top Vacuette 4mL Serum _ SPECIAL PRECAUTIONS Gold Top Vacuette 4mL Serum _ _ _ Lab Note: SAS 4°C LIV Lysosomal enzymes M2 antibodies Lavender Top Vacuette or Green Top Vacuette Gold Top Vacuette 3mL or 4mL 4mL EDTA Whole Blood or Lith Hep Whole Blood Serum Lab Note: WB 4ºC Must be sent within 24hrs _ _ Lab Note: SAS 4°C AMM2 Magnesium Gold Top Vacuette 4mL Serum 066 - 1.08 mmol/L REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) 4 HOURS Lab Note: SAS 4°C LIV Liver/Kidney Microsomal Abs (LKM Abs) KEY FACTORS Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796229 or 02380 796650 10 DAYS 10 DAYS Clinical Biochemistry Bristol Royal Infirmary Marlborough Street BRISTOL BS2 8HW 0117 928 2590 14 DAYS Southampton Immunology Level C Mailpoint 8 Soutthampton General Tremona Road Southampton SO16 4YD 02380 796615 10 DAYS 4 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Mercury SPECIMEN CONTAINER Lavender Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 3mL SAMPLE TYPE Page 113 of 144 REFERENCE RANGES EDTA Whole Blood UNITS SPECIAL PRECAUTIONS KEY FACTORS Trace Metals Unit Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796237 Trace Metals Unit Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796237 nmol/L Lab Note: WB 4ºC Random Sample Mercury Plain (white top) universal 10mL Urine 3mL EDTA Whole Blood nmol / mmolCr Lab Note: Univ 4ºC Methaemoglobin Methotrexate Gold Top Vacuette 4mL Serum TO LAB AT ONCE 0.0 - 1.5 umol/L BY ARRANGMENT ONLY - PLEASE CONTACT THE LAB BEFORE TAKING Gold Top Vacuette 4mL Serum Lab Note: SAS 4°C LIV TURN – AROUND (working days) 18 DAYS 18 DAYS 24 HOURS Lab NB: Manual BMS Lab Note: SAS -20°C Microsomal antibodies REFERRAL LABORATORY (INC ADDRESS) ONLY available for high dose infusions Dept of Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 6 HOURS if URGENT 10 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED Mitochondrial antibodies Gold Top Vacuette 4mL Mycophenolate (MMF) Lavender Top Vacuette 3mL SAMPLE TYPE Serum Page 114 of 144 REFERENCE RANGES _ UNITS SPECIAL PRECAUTIONS KEY FACTORS Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796229 or 02380 796650 Immunosuppressive Drug Monitoring Institute of Liver Studies King's College Hospital Denmark Hill London SE5 9RS 0203 2993147 Clinical Biochemistry Bristol Royal Infirmary Marlborough Street BRISTOL BS2 8HW 0117 928 2590 _ Lab Note: SAS 4°C LIV EDTA WB mg/L Lab Note: SAS 4°C Random Sample Mucopolysaccharides Plain (white top) universal 10mL Urine mg/mmol Lab Note: Univ 4ºC Mycophenolate TURN – AROUND (working days) 10 DAYS 10 DAYS 14 DAYS see MMF Myeloperoxidase antibodies see ANCA Myoglobin Plain (white top) universal Na see Sodium Neurotensin REFERRAL LABORATORY (INC ADDRESS) Large Pink Top Vacuette Lab Note: SAS 4°C ANCA U random Random Sample 24 HOURS 4 HOURS 1 x 6 mL EDTA Plasma 0 - 100 pmol/L Contact Lab. Special request ONLY Lab NB : 2 xSAS -20ºC Patient must be fasting. Transfer sample to Lab immediately Medical Oncology Dept. Charing Cross Hospital Fulham Palace Road London W6 8RF 0208 846 1468 28 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Neuronal Antibodies SPECIMEN CONTAINER Gold Top Vacuette NMDA Antibodies Gold Top Vacuette Occult Blood Plain (orange top) specimen pot Oestradiol Male Female: Prepubertal Follicular Ovulatory Luteal post menpausal Olanzapine Oligoclonal bands Date of issue: 23 June 2011 VOLUME NEEDED 4mL 4mL SAMPLE TYPE Serum Page 115 of 144 REFERENCE RANGES _ UNITS _ Serum SPECIAL PRECAUTIONS Lab Note: SAS -20°C NEUR Lab Note: SAS -20°C KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) Sheffield Protein Department of Immunology Protein Reference Unit PO Box 894 Sheffield S5 7YT 01142 715552 14 DAYS Immunology Churchill Hospital Headington Oxford OX3 7LJ 01865 225995 21 DAYS Faeces 48 HOURS < 191 Gold Top Vacuette Gold Top Vacuette Plain (white top) universal and Gold Top Vacuette 4mL 4mL Serum Serum <40 40 - 253 536 - 1930 121 - 551 < 136 pmol/L 72 HOURS ug/L Lab Note: SAS -20°C 4mL (serum) CSF and serum Blood and CSF required Lab Note: CSF SAS -20ºC + Serum SAS -20ºC Clinical Biochemistry Kings College Hospital Denmark Hill London SE5 9RS 0203 299 5882 14 DAYS Neuroimmunology Room 917 Institute of Neurology Queen Square London WC1N 3BG 02078 373611 extn 3814 18 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED SAMPLE TYPE Page 116 of 144 REFERENCE RANGES UNITS SPECIAL PRECAUTIONS Random Sample Organic Acids Plain (white top) universal 10mL Urine Lab Note: Univ -20ºC Osmolality serum Osmolality - urine Gold Top Vacuette Plain (white top) universal 4mL 10mL Serum Urine 280 - 295 40 - 1040 KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 mosm / kg mosm / kg TURN – AROUND (working days) 18 DAYS 24 HOURS Random Sample. For Water Deprivation Test contact Lab in advance 24 HOURS Lab NB: Manual BMS Ovarian antibodies Gold Top Vacuette 4mL Serum _ _ Lab Note: SAS -20°C OVAR 24h Sample M 80 – 490 Oxalate - urine Acidified 24h container Urine umol/d F 40 - 320 Lab Note: Univ 4ºC Sheffield Protein Dept of Immunology Protein Reference Unit PO Box 894 Sheffield S5 7YT 14 DAYS 01142 715552 Clinical Biochemistry UCL Hospitals 3rd Floor, 60 Whitfield St London W1T 4EU 0845 155 5000 Ext 9405 10 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST P1NP SPECIMEN CONTAINER Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMPLE TYPE Page 117 of 144 REFERENCE RANGES Serum UNITS SPECIAL PRECAUTIONS ug/L Lab Note : SAS -20ºC Pancreatic Polypeptide see Gut hormones Paracetamol Gold Top Vacuette Parathormone, parathyroid hormone see PTH Parietal cell antibodies Gold Top Vacuette PBG see Porphyrins - urine PCNP III Gold Top Vacuette 4mL Serum Normal <10 Therapeutic 10 – 20 Toxic risk at 4hr >.200 Toxic risk at 12hr >50 Gold Top Vacuette REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) Dept. of Clinical Biochemistry 4th Floor Duncan Building Royal Liverpool University Hospital Prescott Street Liverpool L7 8XP 0151 706 4230 14 DAYS mg/L 4 HOURS 24 HOURS 4mL Serum Lab Note: SAS 4°C GPCA 4mL Serum 1.7 - 4.2 ug/L Lab Note : SAS -20ºC Pemphigus/ Pemphigoid Antibodies KEY FACTORS 4mL Serum Lab Note: SAS 4°C PEMP Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796229 or 02380 796650 Dept of Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796615 14 DAYS 18 DAYS 18 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 118 of 144 TEST SPECIMEN CONTAINER VOLUME NEEDED SAMPLE TYPE REFERENCE RANGES Phenobarbitone Gold Top Vacuette 4mL Serum 15 - 40 Phenytoin Free phenytoin Phosphate serum Gold Top Vacuette Gold Top Vacuette Gold Top Vacuette 4mL 4mL 4mL Serum 10 - 20 Serum 1.0 – 2.0 Serum <1m 1.30 -3.00 1-2m 1.00-2.10 2m-12y 1.00-1.90 12y + Phosphate - urine Acidified 24h container Phytanate Pipecolic acid see VLCFA see VLCFA Placental alkaline phosphatase (PLAP) Gold Top Vacuette Urine REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) UNITS SPECIAL PRECAUTIONS KEY FACTORS mg/L Take before next dose ideal sampling times are not indicated due to long half life. 24 HOURS mg/L Ideal sampling times are not indicated due to long half life of phenytoin during long term administration 24 HOURS µg/mL Ideal sampling times are not indicated due to long half life of phenytoin during long term administration mmol/L Levels are artefactully increased by invitro haemolysis and delayed sample centrifugation 0.80-1.40 Therapeutic Drug Monitoring Unit. National Society for Epilepsy. Chalfont St Peter. Chesham Lane. BUCKS 01494 601423 4 HOURS 24h collection 4.0 - 70.0 10 DAYS 24 HOURS Lab Note: White top Vacuette, Advia tray 28 DAYS 28 DAYS 4mL Serum < 100 mu/mL Lab Note : SAS -20ºC Medical Oncology Charing Cross Hospital Fulham Palace Road London W6 8RF 0208 846 1468 5 WEEKS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST SPECIMEN CONTAINER Porphobilinogen see Porphyrins - urine Porphyrins blood Lavender Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED SAMPLE TYPE Page 119 of 144 REFERENCE RANGES UNITS SPECIAL PRECAUTIONS KEY FACTORS 3mL Plain (orange top) specimen pot EDTA Whole blood Faeces Lab Note : -20ºC Porphyrins - urine Potassium Plain (white top) universal Gold Top Vacuette TURN – AROUND (working days) 24 HOURS Lab Note: WB 4ºC Porphyrins faeces REFERRAL LABORATORY (INC ADDRESS) 10mL 4mL Random SAMPLES MUST BE KEPT IN THE DARK PRIOR TO ANALYSIS Urine Serum 3.5 - 5.0 mmol/L May be referred as follow up to inhouse findings Levels artefactully increased by invitro haemolysis and delayed sample centrifugation. Levels may also be artefactually raised in patients with high platelet count. Porphyria Service Department of Medical Biochemistry University Hospital of Wales Neath Park Cardiff, CF14 4XW 0292 0743565 Porphyria Service Department of Medical Biochemistry University Hospital of Wales Neath Park Cardiff, CF14 4XW 0292 0743565 Porphyria Service Department of Medical Biochemistry University Hospital of Wales Neath Park Cardiff, CF14 4XW 0292 0743565 14 DAYS 21 DAYS 24 HOURS or 10 days if referred 4 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST SPECIMEN CONTAINER Potassium - urine Plain 24h container Potassium - urine Plain (white top) universal PR3 antibodies Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 10mL 4mL Page 120 of 144 SAMPLE TYPE REFERENCE RANGES UNITS Urine 25 - 100 mmol/d Urine Serum mmol/L 0 - 9.0 SPECIAL PRECAUTIONS KEY FACTORS 24h collection Pristanate Procollagen III Npeptide Progesterone: Female mid luteal phase: Not lutenised Anovulatory ?Inadequate luteal function Adequate luteal function Proinsulin TURN – AROUND (working days) 24 HOURS Lab Note: White top Vacuette, Advia tray Random Sample 24 HOURS Lab Note: White top Vacuette, Advia tray Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796229 or 02380 796650 u/mL Lab Note: SAS 4°C ANCA Primidone REFERRAL LABORATORY (INC ADDRESS) 10 DAYS see Phenobarbitone See VLCFA 28 DAYS see PCNP 10 DAYS Gold Top Vacuette 4mL Serum <10 10 - 20 nmol/L 72 HOURS 20 - 30 >30 Gold Top Vacuette plus Grey Top Vacuette 4mL plus 4mL Serum plus Fluoride Oxalate Plasma TO LAB AT ONCE SAMPLE MUST BE FROZEN WITHIN 1 HOUR Lab Note: SAS -20°C Take sample for glucose at the same time Contact Consultant Biochemist Peptide Laboratory Royal Surrey County Hospital Egerton Rd Guildford GU2 5XX 01483 406715 21 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED SAMPLE TYPE Gold Top Vacuette 4mL Serum In Pregnancy Protein - CSF Protein - fluid Protein - serum total Protein - urine 24h Protein Creatinine Ratio Protein - urine random REFERENCE RANGES KEY FACTORS Levels may be physiologically elevated by stress, during pregnancy and in patients on anti psychotic drug therapy µg/L 206 - 2240 see PSA see CSF protein Plain (white top) universal 0.1 - 0.4 5mL Gold Top Vacuette g/L TURN – AROUND (working days) 72 HOURS 24 HOURS see Total Protein Urine 0 - 0.15 10mL Urine 7 - 23 10mL Urine 0 - 0.10 g/d g/L 0-3.5 Serum ug/L >60 Yr 0-5.5 24h collection 24 HOURS Lab Note: White top universal 24 HOURS 51-60Yr 0-4.5 4mL 4 HOURS Fluid Serum plain 24h bottle Plain (white top) universal Plain (white top) universal REFERRAL LABORATORY (INC ADDRESS) 24 HOURS <51Yr PSA UNITS SPECIAL PRECAUTIONS 50 - 350 Prolactin Prostate specific antigen Page 121 of 144 Random Sample 24 HOURS Levels may be elevated in UTI, acute retention, post ejaculation (up to 48h) and post DRE (up to 14 d) 24 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST PSA - free Pseudocholinesterase SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED SAMPLE TYPE Page 122 of 144 REFERENCE RANGES UNITS SPECIAL PRECAUTIONS KEY FACTORS see Free PSA Gold Top Vacuette 4mL Serum 600 – 1400 Chemical Pathology Dept Royal Hampshire County Hospital Romsey Rd Winchester SO22 5DG 01962 824287/8 U/L Lab Note: SAS -20°C PTH REFERRAL LABORATORY (INC ADDRESS) Gold Top Vacuette 4mL Serum 1.48 - 7.63 pmol/L TO LAB AT ONCE - SAMPLE MUST BE FROZEN WITHIN 1 HOUR TURN – AROUND (working days) 21 DAYS 21 DAYS 24 HOURS Lab Note : SAS -20ºC PTH-related peptide SPECIAL SPECIAL 0.7 - 1.8 pmol/L CONTACT LAB SPECIAL TUBE REQUIRED - BY ARRANGEMENT ONLY! Lab Note : SAS -20ºC Purkinje antibodies Gold Top Vacuette Rapamune see Sirolimus RAST Gold Top Vacuette 4mL Serum _ _ Lab Note: SAS -20°C NEUR 4mL Serum Lab Note: SAS -20°C 100uL + 40uL each test Specific RAST allergens MUST be stated on request form Clinical Biochemistry 4th Floor Duncan Building Royal Liverpool University Hospital Prescott Street LIVERPOOL L7 8XP 0151 706 4230 5 WEEKS Sheffield Protein Department of Immunology Protein Reference Unit PO Box 894 Sheffield S5 7YT 01142 715552 10 DAYS Department of Immunology Clinical Laboratory Royal Surrey County Hospital Egerton Road Guildford GU2 5XX 01483 464029 10 DAYS (RARE ALLERGENS 28 DAYS) Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Red cell acetyl cholinesterase SPECIMEN CONTAINER Lavender Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 3mL SAMPLE TYPE EDTA Whole blood Page 123 of 144 REFERENCE RANGES >97 UNITS SPECIAL PRECAUTIONS KEY FACTORS Biomedical Sciences Group Health & Safety Lab Harper Hill Buxton Derbyshire SK17 9JN 01298 218099 hu/L Lab Note: WB 4ºC Reducing substances faecal Reducing substances urine Renin: Supine Ambulant Children: < 7d 1wk - 1yr 1 - 11yrs Reticulin antibodies Ri antibodies REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) 28 DAYS see Sugars 10 DAYS see Sugars 10 DAYS 2 - 30 3 - 40 Lavender Top Vacuette 3mL EDTA Plasma see Coeliac screen 4 - 340 4 - 100 4 - 85 mu/L TO LAB AT ONCE - SAMPLE MUST BE FROZEN IN 30 MINUTES Lab Note: SAS -20°C Lab Note: COEL 4°C see Purkinje Lab Note: SAS -20°C NEUR Ro antibodies see ENA Lab Note: SAS 4°C ANAE RNP antibodies see ENA Lab Note: SAS 4°C ANAE Levels may be affected by posture, and antihypotensive or mineralosteroid drug therapy Specialist Biochemistry Mail Pont 8 Level C South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 798717 14 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST SPECIMEN CONTAINER SAA see Amyloid A Salicylate Gold Top Vacuette Scl 70 antibodies see AIP Selenium Dark Blue Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMPLE TYPE Serum Page 124 of 144 REFERENCE RANGES Analgesic 120 – 300 Toxic Risk >400 UNITS SPECIAL PRECAUTIONS Sirolimus Skin antibodies Gold Top Vacuette Lab Note: SAS 4°C ANAE 6mL 4mL Lavender Top Vacuette 3mL Gold Top Vacuette 4mL see Theophylline TURN – AROUND (working days) 4 HOURS Serum 0.8 - 2.0 umol/L Serum M 10 - 70 F 30 - 120 Trace Metals Unit Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796237 nmol/L 14 DAYS 7 DAYS EDTA WB Lab Note: WB 4ºC Serum Lab Note: SAS 4°C PEMP Slophylline REFERRAL LABORATORY (INC ADDRESS) mg/L Lab NB: Teklab -20ºC Sex hormone binding globulin (SHBG) KEY FACTORS Analytical Unit St. Georges Hospital London SW17 0RE 0208 725 5345 Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796229 or 02380 796650 14 DAYS 10 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Sm antibodies Smooth muscle antibodies Sodium SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED SAMPLE TYPE Page 125 of 144 REFERENCE RANGES UNITS see Liver antibodies see Liver antibodies Gold Top Vacuette 4mL Serum 134 - 147 mmol/L Sweat < 40 mmol/L Sodium - urine 24h Plain 24h bottle Urine 130 - 220 mmol/d Sodium - urine Plain (white top) universal Specific IgE SSA antibodies (Ro) 10mL Urine mmol/L CONTACT LAB TO BOOK APPOINTMENT 24h Collection 24 HOURS 24 HOURS Lab Note: White top Vacuette, Advia tray Random Sample 24 HOURS Lab Note: White top Vacuette, Advia tray see IGF1 see Gut Hormones see RAST Gold Top Vacuette Gold Top Vacuette TURN – AROUND (working days) 4 HOURS 10 DAYS 4mL Serum _ _ Lab Note: SAS 4°C ANAE SSB antibodies (La) REFERRAL LABORATORY (INC ADDRESS) Lab Note: SAS 4°C LIV Plain 2mL Tube Somatostatin KEY FACTORS Lab Note: SAS 4°C LIV Sodium - sweat Somatomedin C SPECIAL PRECAUTIONS 4mL Serum _ _ Lab Note: SAS 4°C ANAE Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796229 or 02380 796650 Southampton Immunology Mailpoint 8 Level C Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796229 or 02380 796650 10 DAYS 10 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST SPECIMEN CONTAINER Steroid profile Plain (white top) universal or 24hr plain bottle Sugars - faecal Plain (orange top) specimen pot Sugars - urine Plain (white top) universal Tacrolimus Tau protein Lavender Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 10mL SAMPLE TYPE Page 126 of 144 REFERENCE RANGES UNITS SPECIAL PRECAUTIONS Random Sample or 24hr collection Urine Lab Note: Univ 4ºC 3mL Suggested therapeutic range 1.0 – 12.0 ug/L Lab Note: WB 4ºC TURN – AROUND (working days) 28 DAYS 10 DAYS Deliver immediately Urine EDTA Whole Blood Dept. of Clinical Biochemistry Kings College Hospital Denmark Hill London SE5 9RS 0203 299 3856 Deliver to lab immediately Faeces 10mL KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) 10 DAYS Immunosuppressive Drug Monitoring Insitute of Liver Studies King's College Hospital Denmark Hill London SE5 9RS 0203 2993147 10 DAYS see Beta-2 transferrin Tegretol see Carbamazepine Testosterone Gold Top Vacuette 4mL Serum M 10.0 - 35.0 F 0.5 - 2.6 24 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED SAMPLE TYPE Thyroglobulin & Anti Thyroglobulin antibodies TFT Theophylline Thyroid peroxidase antibodies Tissue transglutaminase antibodies Gold Top Vacuette Page 127 of 144 REFERENCE RANGES <1.0 post thyroid ablation 4mL 4mL KEY FACTORS ug/L Serum TSH 0.35 - 4.50 IU/L Lab Note:SAS -20°C TGAB mu/L Gold Top Vacuette 4mL Serum 7.5 - 20.0 mg/L Gold Top Vacuette 4mL Serum 0 - 60 u/mL Gold Top Vacuette 4mL Serum 0-4 u/mL Ideal sampling times: 1)oral: 8-12h post dose 2) IV: 6-8h after start of IV. Stop infusion for 15 minutes before taking sample REFERRAL LABORATORY (INC ADDRESS) Chemical Pathology Lab Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 Serum 0-40 Gold Top Vacuette UNITS SPECIAL PRECAUTIONS TURN – AROUND (working days) 14 DAYS TSH, FT3 and FT4 levels may all be affected by non-thyroidal illness 24 HOURS Adult levels only 24 HOURS 24 HOURS Lab Note: COEL 4°C Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST TMPG Tubular Reabsorption of Phosphate Topiramate SPECIMEN CONTAINER Plain (white top) Universal Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 10mL 4mL SAMPLE TYPE Urine Serum Page 128 of 144 REFERENCE RANGES UNITS Birth 1.43–3.43 3-5m 1.48-3.30 6-23m 1.15-2.60 2-15y 1.15-2.44 Adult 0.80-1.35 mmol/L glomerular fluid 5 - 20 SPECIAL PRECAUTIONS KEY FACTORS Must have paired blood sample for Phosphate and creatinine Gold Top Vacuette 4mL Toxicology General Screen Plain (white top) universalplus Lavender Top Vacuette plus Gold Top Vacuette 10mL plus 1 x 3mL TPMT Thiopurine methyl transferase Lavender Top Vacuette plus 1 x 4mL 3mL Serum 63 - 79 Lab Note: Urine - white top vacuette , Advia tray Medical Toxicology Unit 4th Floor North Wing St Thomas’ Hospital London SE1 7EH 02071 888689 mg/L EDTA Whole Blood Results may be increased by haemolysis g/L Random Sample Urine plus EDTA Whole Blood plus Serum TURN – AROUND (working days) 4 DAYS Lab Note: SAS -20°C Total Protein REFERRAL LABORATORY (INC ADDRESS) Lab Note: Univ 4ºC Plus WB 4ºC Plus SAS 4ºC Normal 26 - 50. Carrier 10 - 25. Deficiency <10 Lab Note: WB 4ºC 10 DAYS 4 HOURS Medical Toxicology Unit 4th Floor North Wing St Thomas’ Hospital London SE1 7EH 02071 888689 Purine Lab 4th Floor, Block 7 North Wing St Thomas’ Hospital London SE1 7EH 02071 881265 14 DAYS 21 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST SPECIMEN CONTAINER Trace Metals See Cu, Zn and Selenium Transferrin Transglutaminase antibodies Triglycerides 1st or 2nd Trimester Screening Triple Test Trimethylamine Gold Top Vacuette see Coeliac screen Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMPLE TYPE Serum Page 129 of 144 REFERENCE RANGES 1.8 - 3.2 UNITS SPECIAL PRECAUTIONS g/L 10 DAYS Lab Note: COEL 4°C 4mL Serum 0.28 - 2.20 TURN – AROUND (working days) 4 HOURS Patients must be fasting. There is some interference from haemolysis. mmol/L 4 HOURS See Triple Test Red Top Vacuette Plain (white top) universal 4mL Serum Lab Note: SAS -20°C plus Stored -20°C (unless small sample when all sent to QAH) 10mL Random Sample (Early morning urine preferred) Urine Lab Note: Univ 4ºC Troponin I KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) Gold Top Vacuette 4mL Serum < 0.05 ug/L Chemical Pathology Queen Alexandra Hospital Cosham Portsmouth PO6 3LY 02392 286903 10 DAYS Clinical Chemistry and Molecular Genetics, Children's Hospital Western Bank Sheffield S10 2TH 0114 2 71 7445 6 WEEKS 4 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Tryptase SPECIMEN CONTAINER Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMP LE TYPE Serum Page 130 of 144 REFERENCE RANGES 2 - 14 UNITS SPECIAL PRECAUTIONS KEY FACTORS Sheffield Protein Department of Immunology Protein Reference Unit PO Box 894 Sheffield S5 7YT 0114 2 715552 ug/L Lab Note: SAS -20ºC TSH TSH receptor Antibodies TRAB Gold Top Vacuette Plain (white top) universal 4mL Serum Firs Laboratories RSR Ltd Parc Ty Glas Llanishen Cardiff CF14 5DU 029 2076 5550 Specialist Biochemistry Mail Point 8 Level C South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 798717 Lab Note: SAS -20°C TRAB 10mL Urine 3.0 - 7.4 Lab Note: Univ -20ºC Uniphylline Urea 14 DAYS 24 HOURS see TFT Random Sample UDPD REFERRAL LABORATORY (INC ADDRESS) TURN – AROUND (working days) 14 DAYS 18 DAYS see Theophylline Gold Top Vacuette 4mL Serum 2.6 - 6.0 mmol/L Levels are greatly reduced during pregnancy 4 HOURS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Urea - urine Uric acid - joint Uric acid - serum Uric acid - urine SPECIMEN CONTAINER Date of issue: 23 June 2011 VOLUME NEEDED Plain 24h bottle Urine Plain (white top) universal Gold Top Vacuette Joint Fluid 4mL Plain 24h bottle Urine Steroid Profile (USP) See steroid profile U&E - serum Gold Top Vacuette U&E - urine Plain 24h bottle 4mL 199 - 332 UNITS mmol/d SPECIAL PRECAUTIONS KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) 24h collection 24 HOURS Lab Note: White top Vacuette, Advia tray 24 HOURS 4 HOURS 0.12 - 0.42 mmol/L Urine 1.48 - 4.43 mmol/d Valproate 4mL Vancomycin Gold Top Vacuette 4mL Gold Top Vacuette Serum 4mL Serum Serum TURN – AROUND (working days) mmol/L Serum Urine Gold Top Vacuette Phytanic acid REFERENCE RANGES 24h collection 24 HOURS Lab Note: White top Vacuette, Advia tray see Bile Pigments Urobilinogen Very long chain fatty acids Pristinic acid SAMPLE TYPE Page 131 of 144 4 HOURS Na 134 - 147 K 3.5 - 5.0 Urea 2.6 - 6.0 Creat 62 -124 Na 130 – 220 K 25 – 100 Urea 199 -332 50 - 100 4 HOURS 1 Hour for urgent mmol/L mmol/d mg/L 24h collection 24 HOURS Lab Note: White top Vacuette, Advia tray Take sample before next dose. Standardise sampling times if possible as levels may vary during the day 24 HOURS 24 HOURS mg/L Serum Lab Note: SAS 20°C Newborn Screening & Biochem Genetics Southmead Hospital Westbury-on-Trym Bristol BS10 5NB 0117 3235556 21 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Vigabatrin SPECIMEN CONTAINER Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMPLE TYPE Serum Page 132 of 144 REFERENCE RANGES 5-35 UNITS SPECIAL PRECAUTIONS mg/L Lab Note: SAS -20°C VIP Vitamin A Vitamin D TURN – AROUND (working days) Medical Toxicology Unit 4th Floor North Wing St Thomas’ Hospital London SE1 7EH 02071 888689 28 DAYS Chemical Pathology Lab Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 14 DAYS see Gut Hormones Green Top Vacuette 4mL Li Heparin Plasma 1.07 – 3.55 umol/L Lab Note: SAS -20°C Vitamin B12 KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) Gold Top Vacuette Gold Top Vacuette 4mL 4mL Serum 161 - 531 Serum See report for interpretive comments ng/L 3 DAYS nmoL/L Lab Note: SAS -20°C Homerton University Hospital Homerton Row London E9 6SR 0208 510 7887 10 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Vitamin D – 1,25 di(OH) DHVD SPECIMEN CONTAINER Gold Top Vacuette Date of issue: 23 June 2011 VOLUME NEEDED 4mL SAMPLE TYPE Serum Page 133 of 144 REFERENCE RANGES 72 - 125 UNITS pmol/L SPECIAL PRECAUTIONS KEY FACTORS Specialist Biochemistry Mail Point 8 Level C South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 798717 Chemical Pathology Lab Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 MUST BE RECEIVED IN LAB WITHIN 30 MINUTES Lab Note: SAS -20°C Vitamin E Green Top Vacuette 4mL Plasma 11.6 – 37.1 umol/L Lab Note: SAS -20°C VLCFA VMA/Metadrenalins (adult) Adrenaline Dopamine Metadrenaline Noradrenaline see Very long chain fatty acids Acidified 24h Urine bottle . Urine 0 – 0.1 0.49 – 2.85 < 1.4 0.07 – 0.48 < 3.0 TURN – AROUND (working days) 10 DAYS 14 DAYS 21 DAYS 24h collection umol/d Lab Note: Univ 4ºC Normetadrenaline REFERRAL LABORATORY (INC ADDRESS) Levels may be affected by antihyperte nsive and antiprophyl atic drug therapy and stress Dept of Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 14 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST VMA (child) + HVA SPECIMEN CONTAINER Plain (white top) universal Date of issue: 23 June 2011 VOLUME NEEDED 10mL SAMPL E TYPE Urine REFERENCE RANGES Age related Page 134 of 144 UNITS umol/mmolCr SPECIAL PRECAUTIONS Random sample MUST BE RECEIVED IN LAB WITHIN 1 HOUR Lab Note: Univ 4ºC Voltage-gated Ca antibodies Gold Top Vacuette 4mL Voltage-gated K antibodies Gold Top Vacuette 4mL White cell enzymes Yo antibodies Xanthochromia Serum Lab Note: SAS -20°C VGCC Serum Lab Note: SAS -20°C VKAB KEY FACTORS REFERRAL LABORATORY (INC ADDRESS) Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796427 Immunology Churchill Hospital Headington Oxford OX3 7LJ 01865 225995 Immunology Churchill Hospital Headington Oxford OX3 7LJ 01865 225995 TURN – AROUND (working days) 14 DAYS 28 DAYS 18 DAYS see Lysosomal enzymes see Purkinje Universal Lab Note: SAS -20°C NEUR 1 mL CSF See Clinical procedure Lab Note: Special 4ºC Zinc Dark Blue Vacuette Must be bled in Phlebotomy 6mL Plasma 11.0 – 24.0 umol/L Lab NB: Teklab -20ºC Li Hep may be used for Paeds Trace Metals Unit Chemical Pathology Level D South Block Southampton General Hospital Tremona Road Southampton SO16 6YD 02380 796237 14 DAYS Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 135 of 144 HAEMATOLOGY TEST Antenatal screen (Group and antibody screen) Antibodies (specific identification) Blood Group and save serum Bone marrow film (with Trephine biopsy) Cold Agglutinins Direct Antiglobulin Test (Coombes Test) Donath Landsteiner (PCH) Genotypes and Phenotypes HLA B27 SAMPLE & COLLECTION INSTRUCTIONS REFERENCE RANGE COMMON INDICATIONS Pink top 6ml Transfusion tube Pink top 6ml Transfusion tube Pink top 6ml Transfusion tube Please contact Clinical Haematologist for patient review for potential bone marrow Pink top 6ml Transfusion tube (keep sample < 1/32 at 37oC) Lavender 3ml EDTA tube Pink top 6ml Transfusion tube - Contact Consultant Pink top 6ml Transfusion tube 1 x large 6ml Lavender top EDTA tube or 2 x 3ml Lavender topped EDTA tubes (HLA B27 samples received Monday to Thursday only; to reach BNHFT Haematology Dept. by 12 noon the same day the sample is collected, as it is sent to the Regional Centre in Southampton). Kleihauer test Pink top 6ml Transfusion tube and lavender top EDTA tube Anti Xa assay Light Blue citrate tube Beta 2 Microglobulin Bleeding time UNITS Yellow SST gel tube 0.0 – 1.7 Appointment required - please ring Principal 3.5 – 9.5 BMS Jane Needham Turnaround time (working days) 1 Haematological malignant disorders 2 1 2 Cold agglutinin disease; Raynaud’s 7 2 Haemolysis - antibody mediated 4 hours 2 iu/mL ug/mL min Ankylosing spondylitis 1 21 Trans-placental bleed 4 hours Sub cutaeous Heparin monitoring On request or 4 10 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Date of issue: 23 June 2011 SAMPLE & COLLECTION INSTRUCTIONS Page 136 of 144 REFERENCE RANGE UNITS COMMON INDICATIONS Turnaround time (working days) 14 Bleeding; bruising Pre operation Warfarin control Heparin monitoring 3 hours Fibrinolysis; DIC; DVT Temporal arteritis; Inflammatory marker Investigation of abnormal coagulation 3 hours 4 hours Investigation of abnormal coagulation Not response to factor therapy On request or 14 Chromosomes Refer - please speak to laboratory (samples received Monday to Thursday only; to reach the Department by 4.00 pm the same day the sample is collected, as it is sent to the Regional Centre in Salisbury) CSF Cerebal Spinal fluid Coagulation screen Prothrombin Time INR Therapeutic APTT APTT Therapeutic Thrombin time Fibrinogen Fibrinogen Antigen D-Dimer ESR Light Blue top citrate tube Light Blue citrate tube Lavender top 3ml EDTA tube Factor assays 2 x Light Blue top citrate tubes Factors 2, 5, 7, 9, 10,11,12 Factor 13 Factor 13 antigen Factor Inhibitor 2 x Light Blue top citrate tubes Factors VIII, IX, porcine inhibitors, screens FBC (Full Blood Count) Lavender top 3ml EDTA tube [includes blood film if required] 10.9 – 13.9 2-4 25.4 – 34.6 75.0 – 125.0 11.2 – 13.6 1.5 – 4.0 1.43 – 3.55 <0.0 – 0.5 Male < 20 Female < 20 secs 50 – 150 >2 10.0 – 17.3 iu/dL iu/dL mg/L Bethesda Male Hb 130 - 180 Female Hb 110 - 165 secs secs secs g/L mg/L mm/hr 14 4 hours g/L g/L WBC 4.0 - 11.0 10*9/L Platelets 150 - 500 10*9/L [With blood film 3 -5 days] Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST G6PD Glandular Fever screen Hb HPLC Hb electrophoresis HbA2 HbF HbS, HbC, HbD, HbE Abnormal Haemoglobins Sample for reference Centre Haptoglobin assay Heparin Induced Thrombocytopenia HITS INR (International normalised ratio) and warfarin dosing NAP test Lupus inhibitor Silca clot time Dilute Russel Viper Venom time IgM Cardiolipin IgG Cardiolipin Red cell Parasities Malaria film Malaria antigens Microfilariae Trypanosomes Leishmaniasis Date of issue: 23 June 2011 SAMPLE & COLLECTION INSTRUCTIONS Lavender top 3ml EDTA tube Lavender top 3ml EDTA tube Page 137 of 144 REFERENCE RANGE UNITS COMMON INDICATIONS 4.6 – 13.5 Jaundice; Haemolysis post infection Infectious mononucleosis; EBV May be positive in lymphoma & others Haemoglobinopathy Thalassaemia Antenatel and newborn screening programme u/g Hb Lavender top 3ml EDTA tube 1.6 – 3.1 0.1 – 1.0 2x Lavender top 3ml EDTA tube Sent to Haemoglobin reference centre Oxford Yellow top SST gel tube To arrive at BHNFT Haematology by 12 noon on day sample is taken as sample sent to Southampton Yellow top SST gel tube 0.7 - 3.8 Light Blue citrate Tube Therapeutic 2.0 - 4.0 Lavender top EDTA tube - Discuss with laboratory 4 x Light Blue citrate tubes 30 - 100 g/L Haemolysis marker 3 Dependant on abnormality.Up to 3 months 4 Platelet count dropping by 50% in 24 On request or hours when heparin infusion started 7 Warfarin control 4 hours 2 14 0.8 – 1.2 0.8 – 1.2 0 – 12 0 – 13 Lavender top EDTA tube to Haematology for Film. Positive results sent to Hospital for Tropical Diseases % % % Turnaround time 2 4 hours MPL GPL 4 hours Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Date of issue: 23 June 2011 SAMPLE & COLLECTION INSTRUCTIONS Page 138 of 144 REFERENCE RANGE UNITS COMMON INDICATIONS PK (Pyruvate kinase - red cell enzyme) Paroxysmal Noctural Haemoglobinuria Platelet Function Analysis Collagen / EPI Collagen / ADP Lavender top EDTA tube - Contact haematology Lavender top EDTA tube. Platelet Aggregation Red cell survival studies Red cell membrane studies Special tubes and by appointment only; please contact the Principal BMS Jane Needham Special tubes and by appointment only; please contact the Consultant Haematologist Sent to Bristol Lavender top EDTA tube 0.5 - 2.5% 109/l Red cell production; Aplasia; Bleeding haemolysis Yellow top gel tube RA Lavender top EDTA tube 2 x Light Blue citrate tubes Test need to be done ASAP after collection. Please liaiase with Coagulation ext 3294 4 x Light blue citrate and 2 x Lavender Thrombophilia EDTA tubes 81.4 – 126.6 iu/dl 88.3 – 163.5 iu/dl 3.5 – 10.4 iu/dl 2.5 – 4.9 l/l 50 – 150 % Sent to Hammersmith Sent to Hammersmith Sent to Cambridge Reticulocyte count Rheumatoid factor Sickle test Thromboelastography Thrombophilia screen: Antithrombin III Protein C Protein S Free APCR FVIIIc FV Leiden ProtrombinGene Mutation MTHFR 2 x Light Blue citrate tubes Test need to be done ASAP after collection. Please liaiase with Coagulation ext 3294 100 % Turnaround time (Working days) Pyruvate kinase deficiency 4 Haemolysis – anaemia Haemoglobinuria 2 3 hours 87 – 167 59 – 111 Secs Secs Up to two months 4 hours 2 3 hours 4 hours On request or 14 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE TEST Additional Thrombophilia tests Anti Thrombin III antigen Protein C Antigen Total Protein S Plasminogen Homocysteine von Willebrand’s screen VWF VIIIc VWFAntigen VWF Ristocetin co-factor VWF Normandy VWF Collagen binding VIII Multimers White cell markers CD3 CD4 CD8 CD16+56 CD19 LEUK Date of issue: 23 June 2011 SAMPLE & COLLECTION INSTRUCTIONS Page 139 of 144 REFERENCE RANGE 4 x Light blue citrate Other rare Thrombophilia tests are available on request please discuss with Principal BMS 224.0 – 367.0 Jane Needham 2.40 – 4.64 19.1 – 34.3 93.8 – 147.8 Male 5.64 – 14.88 Female3.0 –12.52 3 x Light Blue citrate tubes 1 Lavender EDTA samples received Monday to Thursday UNITS COMMON INDICATIONS Turnaround time Working days) On request or 14 mg/L mg/L ug/mL iu/dl umol/L umol/L von Willebrand’s disease 50 – 150 50 – 150.0 50 – 150 iu/dL iu/dL iu/dL 50 – 150 iu/dL 0.72 – 2.74 0.40 – 1.61 0.22 – 1.12 0.08 – 0.72 0.08 – 0.61 10*9/L 10*9/L 10*9/L 10*9/L 10*9/L 14 On request or 2 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 140 of 144 SEROLOGY TEST SAMPLE & COLLECTION INFORMATION Alpha virus Gold top gel tube Adenovirus antibody Refer to viral antibody screen Amoebic IFAT Antenatal screen (Rubella IgG, HIV, Hepatitis B surface antigen, Syphilis) Antistaphylolysin Gold top gel tube and a faeces sample required also Gold top gel tube (request form MUST be signed) Gold top gel tube Antistreptolysin O (ASO) Gold top gel tube Aspergillus precipitins Gold top gel tube Avian precipitins Gold top gel tube Bartonella antibodies Gold top gel tube Bilharzia antibodies Gold top gel tube Bordetella pertussis antibodies Borrelia burgdorferi antibodies Brucella antibodies Gold top gel tube Cat scratch disease Refer to Bartonella antibodies Gold top gel tube Collection 8 weeks after bite. Brown top 4.7ml gel tube REFERENCE UNITS RANGE COMMON INDICATORS TURNAROUND TIMES (WORKING DAYS) Referred - 21 Days Referred - 21 Days Staphylococcal disease Streptococcal disease Farmers lung 8 (max) Tests performed on WEDNESDAY only. Referred - 21 Days Referred - 21 Days Referred - 21 Days Referred - 21 Days Cat scratch disease Referred - 21 Days Referred - 21 Days Lyme disease 1 Brucellosis Referred - 21 Days 21 Days Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 Page 141 of 144 TEST SAMPLE & COLLECTION INFORMATION REFERENCE UNITS RANGE COMMON INDICATORS TURNAROUND TIMES (WORKING DAYS) Chlamydia psittaci Refer to viral antibody screen Chlamydia Trachomatis antibodies Cytomegalovirus antigen Referred - 21 Days Cytomegalovirus IgM Gold top gel tube (By arrangement ONLY) Urine in a 25ml sterile universal container or respiratory secretions Gold top gel tube Cytomegalovirus IgG Gold top gel tube 1 Dengue antibody Gold top gel tube Referred - 21 Days Enterovirus IgM (includes antibodies to Coxsackie A and B and Echovirus infections) Epstein Barr virus antibodies Filarial antibodies Gold top gel tube Referred - 21 Days Gold top gel tube Referred - 21 Days Gold top gel tube Referred - 21 Days Galactomanan Gold top gel tube Referred - 21 Days Haemophilus B antibody Gold top gel tube Referred - 21 Days Helicobacter pylori antigen Stool sample in 60ml universal 8 Testing performed Friday ONLY Referred - 21 Days 1 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 TEST SAMPLE & COLLECTION INFORMATION Hepatitis A IgG and IgM Gold top gel tube Hepatitis B surface antigen (NOT Antenatal) Hepatitis B antibodies Gold top gel tube Page 142 of 144 REFERENCE UNITS RANGE COMMON INDICATORS TURNAROUND TIMES (WORKING DAYS) 1 7 Hepatitis B markers Gold top gel tube. 10 weeks post vaccination Gold top gel tube Immunity 8 Performed Tuesday ONLY 1 after +ve screen Hepatitis B viral load Gold top gel tube 14 Hepatitis C antibody Gold top gel tube 5 Mon – Thurs ONLY Hepatitis C viral load Gold top gel tube Referred -21 Days HIV 1 and 2 antibodies (NOT Antenatal) 1 HIV viral load Gold top gel tube (request form MUST be signed and state Patient has consented to test) Lavender top EDTA tube Influenza A antibodies Refer to viral antibody screen Influenza B antibodies Refer to viral antibody screen Legionella antibodies Gold top gel tube Legionella urinary antigen 25ml sterile universal 1 Leishmania antibodies Gold top gel tube Referred -21 Days Leptospira antibodies Gold top gel tube Referred -21 Days Malaria Lavender top EDTA to haematology for Film and call Microbiologist for advice. Antibodies rarely required. Referred -21 Days Atypical pneumonia Referred -21 Days Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 TEST SAMPLE & COLLECTION INFORMATION Measles antibodies IgG IgM Meningococcal PCR Gold top gel tube Gold top gel tube Lavender top EDTA tube. By prior arrangement with the laboratory. Gold top gel tube Mumps antibodies Page 143 of 144 REFERENCE UNITS RANGE COMMON INDICATORS TURNAROUND TIMES (WORKING DAYS) Ring CCDC if 1 suspected Referred -21 Days Meningococcal Referred -21 Days disease Ring CCDC. Ring CCDC if Referred -21 Days suspected. Referred -21 Days Mycoplasma antibodies Refer to viral antibody screen Parvovirus B19 IgM Gold top gel tube Suspected infection in pregnancy Referred -21 Days Q fever (Coxiella burnetii) antibodies Refer to viral antibody screen Puo flu like illness, returning traveller, animal exposure, culture negative Endocarditis Referred -21 Days RSV antibodies Refer to viral antibody screen Rubella IgG Gold top gel tube Immunity 7 Rubella IgM Gold top gel tube. Date of onset essential. Referred -21 Days Schistosome antibodies Gold top gel tube Infection. If suspected ring CCDC Bilharzia Strongyloides serology Gold top gel tube Syphilis serology Gold top gel tube Referred -21 Days Referred -21 Days Infection 10 Basingstoke and North Hampshire NHS Foundation Trust Revision: 7 Q-Pulse Filename: MP-GEN-HANDBK Basingstoke & North Hampshire Hospital Author: David Beacher Authorised by: N. Hutchinson PATHOLOGY DIRECTORATE Date of issue: 23 June 2011 TEST SAMPLE & COLLECTION INFORMATION ToRCH screen (Toxoplasma, Rubella IgM and IgG, CMV IgM, Herpes) Toxoplasma antibodies Gold top gel tube Tropical screen Varicella zoster antibodies Viral respiratory antibody screen Yersinia antibodies Gold top gel tube Gold top gel tube – Discuss with Microbiologist Gold top gel tube Gold top gel tube, collected between day 1-3 (acute) and day 10-21 (convalescent). The acute specimen will be stored until the convalescent is received. (Adenovirus, Chlamydia psittaci, CMV, C.burnetii, Influenza A and B, RSV, Mycoplasma). The range of investigations performed will depend on clinical details; accurate and full information will ensure the relevant tests are performed. Gold top gel tube Page 144 of 144 REFERENCE UNITS RANGE COMMON INDICATORS TURNAROUND TIMES (WORKING DAYS) Referred -21 Days Infection 2 Immunity 1 Referred -21 Days Referred -21 Days