BIOMED 351 Endocrinology Exam
advertisement

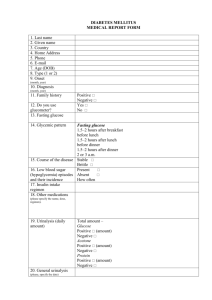
Name__________________________________________ Brown Medical School Bio 351 Endocrinology-Pathophysiology Systemic Pathology Organ System Pharmacology Final Exam March 24, 2006 Course Leaders James Hennessey, MD Elaine Bearer, MD-PhD Robert Patrick, PhD Pathology Pharmacology A 29 year-old woman with type 1 diabetes and hypothyroidism presents to her endocrinologist with progressive fatigue and weight loss. Her only medications are a brand-name levothyroxine preparation and insulin Aspart via an insulin pump. A recent TSH was within normal limits. Her diabetes is in excellent control as evidenced by her recent hemoglobin A1c of 6.4 % (Nl 4.3-5.8), though she does report an increased frequency of hypoglycemic episodes. Physical exam is notable for a blood pressure of 88/ 56 mmHg and modest hyperpigmentation of the buccal mucosa. Adrenal insufficiency is suspected. 1. The most useful initial test in this patient would be: A. B. C. D. E. Metyrapone test Midnight salivary cortisol Cortrosyn stimulation test 24 hour urine collection for free cortisol None of the above 2. The most likely cause of adrenal insufficiency in this patient would be: A. B. C. D. E. Autoimmune adrenalitis Tuberculosis Pituitary tumor Adrenoleukodystrophy None of the above 3. Treatment would most likely include: A. Glucocorticoid but not mineralocorticoid B Mineralocorticoid but not glucocorticoid C. Both glucocorticoid and mineralocorticoid D. Neither glucocorticoid nor mineralocorticoid E. None of the above 4. True/false The histology showed in the image above is consistent with the most likely clinical diagnosis in this case? 5.The key diagnostic feature is: A. Pink hyalinization B. neovascularization C. small roud blue cells invading the parenchyma D. necrosis A 23-year old Brown medical student with type 1 diabetes develops diabetic ketoacidosis after a bout of viral gastroenteritis and skipping several insulin injections in the past 24 hours. She complains of polyuria but has been unable to keep down fluids. She is taking rapid deep breaths (Kussmaul respirations) and appears quite fatigued but is cooperative and able to answer all questions. Laboratory data includes: pH 7.18 (Nl 7.36-7.49), Glucose 574 (Nl < 100 mg/dL), Potassium 4.9 (Nl 3.5-5.1 meq/L), serum and urine ketones strongly positive. 6. Of the following, the most important factor in the patient’s production of ketone bodies is: A. Increased gluconeogenesis in the liver B. Decreased glucose uptake in muscles C. Increased lipolysis in adipocytes D. Enhanced Insulin action in the peripheral tissues E. None of the above are important factors 7. Potassium therapy: A. Would not be necessary in this patient B. Would be indicated as soon as urine output is established C. Should be started intravenously after the ketoacidosis has completely resolved. D. Can be safely withheld until the patient is discharged home E. Is only required for those who also have Addison’s disease 8.Of the following, the least useful intervention would be A. Bicarbonate B. Insulin C. Normal saline D. L-thyroxine E. All of the above would be unnecessary 9.The following 3 questions refer to the image below: 10.The image shown is: A. An islet of Langerhans in the pancreas B. A glomerulus in the kidney C. An aveola in the lung D. A tumor in the prostate 11.The small round cells are most likely: A. Malignant epithelial cells B. CD8 positive lymphocytes C. Polymorphonuclear leukocytes D. mesangial cells 12.At this stage in this disease progression, there would most likely be A. Decreased blood glucose B. Increased insulin levels C. Elevated glucose in the blood D. Anti-insulin antibodies in the blood E. Boney metastasis A 78 year old woman comes to your office for her annual check-up accompanied by her daughter. Reviewing her intake data, you find that she has lost 15 pounds over the past year even though she was previously at her ideal weight. In questioning the patient, you find that her weight loss has been more acute, i.e., over the past 3 months due to a bout with pneumonia. On exam, you notice that her dentures are fitting poorly and her gums are inflamed. The patient’s daughter tells you that her mother has only been consuming cream soups, cream of wheat, mashed potatoes, jello and beverages. 13. Proportionately, the more acute the weight loss, especially if there is very little physical activity during the same period of time, the more: A. Adipose tissue is lost B. Lean body weight is lost C. Likely fluid is being accumulated D. Likely bone accounts for the majority of loss E. None of the above 14. This patient’s acute weight loss is superimposed on the muscle loss that naturally occurs with age. This muscle loss with aging, known as sarcopenia, occurs at a rate of 1% loss per year after the age of: A. 65 B. 45 C. 55 D. 75 E. 95 15. In evaluating her current diet you ask the patient and her daughter what beverages the patient has been drinking and they state that she drinks mostly tea with a little sugar and some grape juice. You realize the diet is grossly inadequate in a broad spectrum of nutrients. How would you proceed? A. Recommend nutritional supplements such as Ensure or Boost and refer to a dentist B. Recommend a vitamin and mineral supplement and refer to a dentist C. Refer to a dentist, knowing that once her dentition improves, her nutritional status will improve D. Recommend anabolic steroids and a new dentist E. Refer to an exercise physiologist for physical fitness training and strength assessment A 23-year-old woman living in the mountains of Bolivia is seen for evaluation of a goiter. She reports growing up in a village where nearly all of her elementary school classmates also had goiters. Several of her cousins and classmates siblings were severely retarded. On review of systems she reports fatigue, weight gain, cold intolerance and the recent onset of morning nausea. Her last menstrual period began 8 weeks prior to the visit. 16. Which test is the most likely to reveal the etiology of her goiter? A. B. C. D. E. An anti TPO antibody A urinary Iodine determination A thyroxine level A serum thyroglobulin level A thyroid ultrasound 17. Following this patient’s story further, a urine pregnancy test returns positive. You estimate, based on the hCG level that she is about 6 weeks pregnant. Which of the following concerns would apply to her baby? A. Even if the patient is hypothyroid, the baby should be fine as it’s thyroid should be able to produce thyroxine sufficient for it’s needs. B. In this circumstance, urine pregnancy tests are notoriously inaccurate and the patient is actually highly unlikely to be pregnant. C. Fetal outcomes are independent of maternal thyroid status and genetically determined. D. Fetal thyroid function does not develop until later in gestation and the baby’s development would be dependent on thyroid hormone transferred from the mother. E. Passive transfer of TSH receptor antibodies from mother to baby does not effect fetal thyroid function as the placenta inactivates the immunoglobulins. 18. If a patient requires treatment with L-thyroxine for primary hypothyroidism, which of the following tests is/are generally recommended for monitoring long-term response to treatment? A. B. C. D. E. Free T4 FreeT4 and free T3 TPO antibodies and free T4 TSH and free T4 TSH 19. All of the following statements concerning L-T4 are correct EXCEPT: A. L-T4 has a longer half-life compared to L-T3 B. Most (>50%) of the L-T4 in the blood is protein bound C. Calcium decreases L-T4 absorption from the GI tract D. Whenever L-T4 is used in thyroid therapy, L-T3 must also be administered E. The thyroid gland normally contains more LT-4 than LT-3 A 53-year-old woman reports a 6-week history of palpitations, heat intolerance and anxiety. Her primary care physician’s associate has prescribed a B-blocker for her over a weekend call and she has noticed increased frequency of bowel movements. On physical exam, her resting pulse rate is 112 beats per minute (BPM), blood pressure is 145/80 mmHg and she appears flushed and distracted. Eye exam reveals an alert look without obvious proptosis; her thyroid is enlarged and feels somewhat nodular. Heart exam is note worthy for an irregularly irregular rhythm and EKG reveals atrial fibrillation at a rate of 115 BPM. Thyroid function tests reveal a TSH of <0.01 uU/ml (nl 0.5-4.0), Free T4 of 2.4 ng/dl (nl 0.8-1.8). She is referred for a 123-I uptake and scan which reveals an uptake of 58% at 24 hours (nl 15-30%) and a homogeneous tracer distribution interrupted by an large area of no uptake in the left lower pole region. A thyroid ultrasound reveals heterogeneous consistency of the right lobe and upper left lobe with a 3.5 X 3.4 X 2.8centimeter hypoechoic nodule with what appear to be microcalcifications in the lower left lobe. 20. In regard to the thyroid function abnormality in this patient’s case, which of the following are likely? A. This patient is presenting with classic hypothyroid symptoms, most likely due to iodine deficiency. B. At this age, tachycardia is likely due to underlying heart disease and not likely associated with thyroid dysfunction. C. All of the thyroid function abnormalities can be best explained by the typical presentation of the left lower lobe nodule. D. This patient likely has autoimmune thyroid disease. E. This patient likely has a hypothalamic process which has resulted in pituitary production of TSH which is over stimulating thyroid hormone production. 21. The image above demonstrates key features of this disease which include all of the following EXCEPT A. Follicular cells are tall and crowded B. Pale colloid with scalloped margins C. Infiltration of inflammatory neutrophils D. Lymphoid infiltrates with predominance of T-cells E. Germinal centers 22. The patient described above is rendered euthyroid with appropriate therapy. She returns 6 months later after a repeat ultrasound is performed which reveals that her nodule has increased in size by approximately 25%. The appearance of microcalcifications is persistent and the patient is referred for an appropriate diagnostic intervention. Which of the following statements is true in regard to this nodule? A. Activating TSH-receptor mutations are commonly described in patients with nonfunctioning nodules such as the one described above. B. A fine needle aspiration of this nodule revealing papillary structures, nuclear inclusions and psammoma bodies would heighten concern of malignancy. C. The lack of pain in the thyroid area in this patient’s presentation is most consistent with a diagnosis of de Quervain’s giant cell thyroiditis. D. The most likely cause of growth of this nodule is a TSH secreting tumor of the pituitary. E. Most thyroid malignancies demonstrate a clear-cut familial inheritance pattern. 23. Which of the following statements regarding the use of thionamide drugs, i.e., methimazole and propylthiouracil, for treatment of hyperthyroidism is true? A. Methimazole is the preferred drug in pregnant and breast-feeding women. B. Their primary mechanism of action is to reduce thyroxine synthesis by inhibiting thyroid peroxidase C. Rare but serious adverse effects include ventricular tachycardia and rapidly developing cataracts. D. Propylthiouracil has a longer duration of action of and can be given less frequently than methimazole. E. Thionamides are the primary treatment for Graves Disease because permanent remission occurs in > 60% of patients after 12-18 months of treatment 24. Prescription medications currently available for the treatment of obesity operate through mechanisms of action which include: A. The enhancement of the absorption of fat through the activation of lipase in the gut. B. The combined effect of serotonin reuptake inhibition and increased serotonin production. C. The reuptake inhibition of norepinephrine and dopamine. D. Direct stimulation of Leptin secretion E. Indirect suppression of thyroxine production 25.Neurotransmitters involved in mechanisms of weight control include A. Serotonin B. Lipase C. Dopamine inhibiting substance D. Leptin E. Adipocyte stimulating factor 26.Surgical intervention for the treatment of obesity includes procedures that restrict intake and limiting the absorption of nutrients. Regarding these procedures, A. The gastric pouch procedure should be used prior to utilizing the Roux-en-Y gastric bypass procedure. B. Roux-en-Y gastric bypass is a more complex procedure with more severe side effects and typically more complications than the gastric pouch procedure. C Patients with a BMI greater than 40 are best treated through the use of surgical intervention. D. Patients with BMI less than 30 Kg/m2 are the best candidates for bypass E. None of the above A 16 year old girl presents to your office for the evaluation of weight gain. She denies overeating but loves soda and juice, watches 5 hours of TV per night, and is active only in gym class at school. Her past history is unremarkable and family history reveals that several members of her family are obese and have type 2 diabetes. She does not take any medications at present. Her menses are regular, and the remainder of the review of systems is negative. On physical examination, her height is 157 cm (25th percentile), weight 97 kg (>95th percentile), BMI 39.4 (>95th percentile). Her BP is 110/70. Her obesity is generalized. She has dark thickening of the skin around her neck. Her thyroid is of a normal size and texture. Her liver span is normal. She has completed puberty and has some terminal hair above her lip, and along her linea alba. The remainder of the examination is normal. 27. This patient’s obesity is most likely due to: A. Hypothalamic dysfunction B. Hypothyroidism C. Leptin deficiency D. Exogenous obesity E. Cushing’s Syndrome 28. Given the physical findings above, which potentially reversible complication is already present? A. Sleep apnea B. Hypertension C. Insulin resistance D. Hepatic cirrhosis E. Type IV hyperlipidemia 29. Proper management of this patient would include: A. The initiation of Orlistat by giving the patient a prescription for this medication at this visit. B. Referral to a bariatric surgeon to be evaluated for a Roux-en Y procedure. C. Obtain thyroid function studies as part of the bariatric evaluation of this patient. D. Have the patient start an exercise program and follow up in 6 months. F. Prolonged fasting should be instituted as soon as possible. A 49 year old man is referred at the recommendation of his ophthalmologist, who reported findings consistent with proliferative diabetic retinopathy. The patient has noted blurred vision, polyuria, polydypsia, and weight loss of about 10 lbs during the past 3 months. History and system review are otherwise unremarkable. Clinical exam is significant for weight of 184 lbs, BMI 27, decreased sensation in the feet by monofilament testing and absent Achilles reflexes. Laboratory data: Glucose 374 mg/dL (Nl < 100) HbA1c 11.8% ( Nl 4.3-5.8) Electrolytes normal Creatinine 1.2 mg/dL (0.4-1.3 mg/dL) BUN 20 mg/dL (Nl 6-24 mg/dL) Urine microalbumin 445mg/gram creatinine (< 300) 30. Which of the following statements is true? A. The patient probably has type 1 diabetes B. He meets criteria for diagnosis of microalbuminuria C. Neurologic findings are consistent with autonomic neuropathy D. Microaneurysms and exudates are the hallmark findings of proliferative diabetic retinopathy E. Pan-retinal laser photocoagulation is indicated 31. At the end of his initial visit, the patient requests information regarding the causes of diabetes and potential benefits of treatment. Which of the following statements is true? A. Cellular damage in diabetes results from increased formation of prostacyclin and nitric oxide and decreased formation of growth factors such as vascular endothelial growth factor B. Increased reactive oxygen species produced by insulin resistance and glucagons excess is the major cause of diabetic microvascular disease C. The patient’s risk of developing microvascular disease is directly related to his level of future glycemic control D. No clinical trials have examined the potential benefit of glycemic control in preventing diabetic complications E. Treatment of hypertension does not affect the risk of diabetic microvascular disease 32. Assuming the patient is not currently using insulin, it would be least appropriate to A. B. C. D. E. add which of the following to his current therapy: Pramlintide Insulin Sulfonylurea Metformin Sulfonylurea Fundoscope exam of the retina might reveal the image shown above. 33. These changes in the retina are primarily a consequence of all of the following complications of diabetes EXCEPT A. Non-enzymatic glycosylation of extracellular matrix and basement membrane B. Increased susceptibility to bacterial infection C. Proliferation of blood vessels D. Hypoxia due to decreased perfusion E. Vascular leakage A 41 year old woman with long-standing type 1 diabetes is hospitalized because of a nonhealing ulcer over the first metatarsal head on her right foot. She denies pain or fever and denies previous ulcers. She takes a mix of insulin (NPH and regular) twice daily with breakfast and supper, checks her blood glucoses levels 1-2 times daily, and sees her physician every 6 months. On physical exam, a 2.5 cm diameter necrotic ulcer with exudate and surrounding erythema is present. Sensation is decreased in the hands and feet. Laboratory data: Creatinine 1.5 mg/dL (Nl 0.4-1.3) BUN 24 mg/dL (Nl 6-20) 24 hr urine protein 2.48 grams (Nl 0-150) 34. Which of the following is true? A. At this point, her future risk of undergoing an amputation of some type is about 5% B. Risk factors for ulceration and amputation include tobacco use and peripheral vascular disease C. The risk of developing foot ulcers is not related to level of glycemic control D. Women with diabetes are less likely to develop coronary heart disease or stroke than diabetic males of similar age E. Intensive insulin therapy will improve glycemic control but will also have an adverse effect on wound healing 35. Of the following statements regarding diabetes and renal function, which is most accurate? A. Because of the marked proteinuria, the patient very likely has non-diabetic renal disease. B. Clinical studies indicate that most diabetics have a decreased GFR at the actual time of onset of their diabetes. C. At least 90% of patients will develop diabetic nephropathy if they have diabetes for 20 years or more. D. Diabetic nephropathy is associated with increased risk of cardiovascular disease even in the early stages. E. Caucasians with diabetes are at greater risk of developing end-stage renal disease than Afro-Americans or Latinos . 36. Potential problems with the patients current two-shot insulin regimen would be likely to include: A. More difficulty with overnight hypoglycemia than with a Glargine-containing regimen B. More difficulty with meal-timing than with a Lispro-containing regimen C. More difficulty achieving tight glycemic control than with a four-shot regimen D. Inaccuracy of mixing NPH and regular with failing vision E. All of the above A 55-year old male presents with fatigue, easy exhaustion, and personality changes. During the past 4 years, he has spontaneously passed several calcium kidney stones. He was taking no medications. Physical examination was unremarkable. Laboratory test results were as follows: BUN 18 mg/dl ( Nl 6-20) Creatinine 1.1 mg/dl (Nl 0.4-1.3) Albumin 4 gm/dl (Nl 3.6-4.4) Calcium 11.3 mg/dl (N 8.5-10.5) Phosphate 2.5 mg/dl (N 3-4.5) Liver enzymes normal Intact PTH 70 pg/ml (N 20-72) DXA lumbar spine, hip, both normal but forearm BMD consistent with osteopenia 37. The most likely diagnosis in this patient is: A. B. C. D. E. Milk alkali syndrome Primary hyperparathyroidism Vitamin D intoxication Humoral hypercalcemia of malignancy Hyperthyroidism 38. Appropriate therapy for this patient would be: A. B. C. D. E. Low calcium diet Calcitonin therapy Bisphosphonate therapy Neck exploration High phosphate diet 39. A 65 year-old woman with normal renal function, mild hypercalcemia and an elevated parathyroid hormone level is found to have an enlarged right upper parathyroid gland and 3 normal sized parathyroids. The most likely diagnosis is: A. Secondary parathyroid hyperplasia B. Parathyroid adenoma C. Type 1 multiple endocrine neoplasia syndrome D. Primary chief cell hyperplasia E. Tertiary hyperparathyroidism 40. A fine needle aspiration of a 2 cm thyroid mass in a 30 year-old woman contains cells with enlarged clear nuclei, prominent nuclear grooves and nuclear pseudoinclusions. The most likely diagnosis: A.Follicular adenoma B.Papillary carcinoma C.Undifferentiated (anaplastic) carcinoma D.Medullary carcinoma E.Adenomatous (hyperplastic) nodule 41. Which of the following statements concerning medullary thyroid carcinoma is true: A.Most common type of thyroid cancer among individuals exposed to irradiation in childhood. B.Heritable forms of this tumor have an autosomal recessive pattern of inheritance. C.Heritable forms of this tumor are commonly associated with pheochromocytomas. D.Pituitary tumors are found frequently in association with these tumors. E.Are derived from follicular cells of the thyroid. A 42-year old woman presented with longstanding tingling and numbness of her hands and fingers, and intermittent leg cramps. Ten years ago, she had neck surgery for removal of a goiter. Physical examination was positive for bilateral cataracts and positive Chvostek and Trousseau signs. Laboratory test results were as follows: BUN 20 mg/dl (Nl 6-20) Creatinine 1.0 mg/dl (Nl 0.4-1.3) Albumin 4 gm/dl (Nl 3.6-4.4) Calcium 7.0 mg/dl (Nl 8.5-10.5) Phosphate 5.0 mg/dl (Nl 3-4.5) Mg 1.8 mg/dl (1.3-1.9) 1,25-OHD 20 pg/ml (Nl 20-60) 25-OHD 30 ng/ml (Nl 30-80) PTH 10 pg/ml (Nl 20-71) 42. The most likely diagnosis in this patient is A. Vitamin D deficiency B. “Bone hunger” C. Hypoparathyroidism D. Hypomagnesemia E. Pseudohypoparathyroidism 43.The most appropriate treatment would be: A. Magnesium supplements B. Vitamin D C. Thiazide diuretic D. PTH injections E. Calcium gluconate 1 gm daily 44.A specific diagnosis of follicular carcinoma of the thyroid requires the presence of: A. B. C. D. E. Capsular and/or vascular invasion Numerous psammoma bodies Orphan Annie eye nuclei Demonstration of amyloid within the tumor stroma Numerous mitoses A 55-year old male is admitted to the hospital because of progressive lethargy, anorexia and occasional nausea and vomiting. His serum calcium level is 14.0 mg/dl. Chest roentgenograms show a left lung mass. 45. Which of the following would likely be found? A. Elevated PTH level B. Low urine calcium level C. Low Serum TSH and Free T4 D. Low Serum PTH E. Elevated serum magnesium 46.In addition to hydration with intravenous isotonic saline solution, which of the following would be most effective in lowering his serum calcium level? A. Furosemide B. Hydrochlorothiazide C. Zoledronic acid D. Prednisone E. Calcitonin True-False 47. Tumors with the morphological and clinical features of pheochromocytomas may arise in a variety of extra-adrenal sites. 48. Most adrenal tumors associated with the overproduction of aldosterone are malignant. 49. Some cases of adrenal hyperplasia may be associated with decreased production of aldosterone and cortisol. Following a routine physical examination, a 69-year old male is noted to have a serum alkaline phosphatase level which is twice normal. He is asymptomatic. His liver function tests are otherwise normal. Serum calcium and phosphate levels are normal. 50. The most likely diagnosis is: A. Primary hyperparathyroidism B. Bone metastases C. Osteomalacia D. Paget’s disease of bone E. Secondary hyperparathyroidism 51. Which of the following abnormalities is present typically in patients with type 2A multiple endocrine neoplasia: A. Medullary thyroid carcinoma, pheochromocytoma, parathyroid hyperplasia B. Parathyroid carcinoma and jaw tumors C. Pancreatic endocrine tumors and pituitary adenomas D. Renal cell carcinomas and pheochromocytomas E. Parathyroid hyperplasia and pituitary tumors A 66 year old woman presented with a painless saber shin deformity of the right tibia. On bone scan, there was increased uptake in the proximal left femur and right tibia. X-rays revealed sclerosis and lytic lesions of the proximal left femur and right tibia. 52. An appropriate recommendation for this patient would be: A. B. C. D. E. Etidronate Nasal calcitonin No therapy indicated at this time Risedronate Oral pamidronate A 60-year old male complains of back pain and fatigue. Resting pulse is 110 and there is tenderness over the lumbar spine. Laboratory data reveal a hematocrit of 27% (Nl 3245), serum calcium of 12.0 mg/dl (Nl 8.5-10.5), a normal serum alkaline phosphatase, and serum protein electrophoresis shows a monoclonal gamma globulin spike. Skeletal X-rays reveal severe demineralization. 53. The most likely diagnosis is: A. B. C. D. E. Primary hyperparathyroidism Multiple myeloma Severe osteoporosis Sarcoidosis Paget’s disease A 58-year old white female presents with mild back pain. After lifting her 25 pound grandson, she experienced sharp and severe pain in the center of her back. General health had been good. She was taking no medications. Menopause occurred at 51 years of age and she received hormone replacement therapy for less than a year. She had been smoking a pack per day for 20 years. Milk intake was negligible. Physical examination was normal except for a mild to moderate thoracic kyphosis. Blood chemistry profile, CBC and serum 25-OHD were normal. Thoraco-lumbar spine x-rays revealed two thoracic vertebral compression fractures. 54. The most likely diagnosis in this patient is A. Paget’s disease of bone B. Metastatic disease C. Postmenopausal osteoporosis D. Primary hyperparathyroidism E. Cushing’s syndrome A. B. C. D. E. 55. The most effective therapy of the following would be Hormone replacement therapy Nasal calcitonin Bisphosphonate Fluoride Calcium 56. In a 40 year-old woman with a cortisol producing 2 cm in diameter adrenocortical tumor, which of the following statements is correct: A. B. C. D. E. The contralateral adrenal is typically hyperplastic Pituitary ACTH cells are hyperplastic There is a high likelihood that the adrenal tumor is benign Plasma ACTH levels are markedly increased The patient is likely to have generalized hyperpigmentation. 57. Pheochromocytomas of the adrenal gland. A.Produced catecholamines and steroid hormones B.Are usually benign tumors C.Are typically unilateral in patients with type 2 multiple endocrine neoplasia D.Typically present in childhood E. Are often associated with pituitary adenomas 58. Which of the following statements concerning pituitary adenomas is true. A. Usually malignant B. Affected patients normally present with hyperthyroidism C. The most common subtype contains prolactin D .Composed of cells with squamous differentiation and areas of cyst formation E. Most common tumor arising in the posterior lobe of the pituitary 59. A needle biopsy of a diffusely enlarged thyroid gland in a 50 year-old woman with hypothyroidism shows extensive lymphoid infiltrates with reactive germinal centers and multiple foci of oncocytic (Hurthle cell) change. The most likely diagnosis is: A.Subacute (granulomatous) thyroiditis B.Amyloidosis C.Hashimoto’s disease D.Oncocytic (Hurthle cell) carcinoma E.Secondary hypothyroidism due to TSH deficiency A 27-year old woman presents to your office stating that she has not had a period in 9 months. Her history is notable for having noticing significant weight loss from the 150 lb range to approximately 110 lbs. She had been at 150 lbs. since age 16. In questioning her, she does confess to signs and symptoms consistent with an eating disorder and you determine that the weight loss is attributable to this without any signs of a malignancy or other etiologic conditions. She denies hot flashes. As part of your evaluation you administer progesterone to the patient and she does not have a withdrawal bleed. 60. Which of the following tests results would you anticipate finding? A. High TSH B. Abnormal imaging study of the brain (example: MRI) C. Abnormal imaging study of the uterus (example: Hysteroscopy or Ultrasound) D. Low or normal FSH E. High Testosterone 61. If you were to give this woman estrogen followed by progesterone for one month which of the following would you expect? A. B. C. D. E. Resumption of a normal menstrual pattern A single period following discontinuation of the progesterone Heavy uncontrolled and continued bleeding No bleeding The onset of symptoms of the menopause (hot flashes, etc.) A 25 year old woman presents stating that her periods have stopped. She has hot flashes. She has had no surgical instrumentations or surgery. During the course of an evaluation, her chromosomes (karyotype) return the following. 62.Which of the following is the most likely cause of her amennorrhea A. Stress B. Premature ovarian failure C. A malignant brain tumor D. Uterine adhesions E. A benign brain tumor 63. Which of the following tests would most likely be abnormal on evaluation? A. B. C. D. E. FSH Prolactin Progesterone MRI of the brain Imaging study of the uterus 64. A 35 year old woman has amenorrhea. You note increased facial hair, a deep voice and a large right pelvic mass on examination. Which of the following ovarian tumors could explain the clinical findings? A. B. C. D. E. Mature cystic teratoma Fibroma Endodermal sinus tumor Sertoli-Leydig cell tumor Struma Ovarii 65. The most common cell types of origin for testicular and ovarian cancers are: A. B. C. D. E. Epithelial in testis and epithelial in ovary. Epithelial in testis and germ in ovary. Germ in testis and germ in ovary. Germ in testis and epithelial in ovary. Stromal in testis and stromal in ovary. The Women’s Health Initiative is perhaps the most important study addressing the menopause ever conducted, fundamentally changing how menopausal women are treated. . 66. In this study, the combined (hormone) replacement therapy trial was stopped prior to the planned completion because of which of the following findings? A. B. C. D. E. More heart attacks than anticipated. More cases of breast cancer than anticipated. Not as protective for colon cancer as anticipated. Not as protective of fractures as anticipated. Too many deaths in the study (hormone replacement therapy) group compared to placebo. 67. Which of the following is a BENEFICIAL effect of estrogen replacement therapy (without progesterone) as shown by the Women’s Health Initiative? A. B. C. D. E. Decrease in heart disease Decrease in breast cancer Decrease in stroke Decrease in bone fractures Decrease in gallbladder cancer An 18 yo college student presents with signs of androgen excess. On taking a patient’s history she states that she has noticed a recent rapid increase in hair growth and acne. She has also noticed an increased libido 68. Which of the following tests is most consistent with her history and the imaging studies shown (with markedly enlarged and cystic ovary)? A. B. C. D. E. Elevated testosterone Elevated prolactin Elevated TSH Elevated CBC Elevated FSH 69. You conclude that this patient has a virilizing tumor. Which of the following findings on physical exam would be most consistent with this diagnosis? A. Acne B. Secondary sexual hair growth C. Clitoromegaly D. Moderate obesity E. Increased muscle mass F. Breast engorgement 42-year-old male presents to the ER with nausea, vomiting, and abdominal pain radiating to the back. Past medical history is negative for alcohol use and gallstones. Physical exam is unremarkable except for tenderness to palpation in the mid-epigastric region and pustular lesions over his thigh and extensor surface of his arms consistent with eruptive xanthoma. 70. The serum is found to have creamy white surface layer. Plasma lipid profile that best describes this patient A. Elevated Triglyceride B. Elevated Low density lipoprotein C. Elevated Lipoprotein (a) D. Elevated High-density lipoprotein E. Low Total Cholesterol A. B. C. D. E. 71. The first step in the treatment of this patient Restriction of dietary fat Nicotinic Acid Fibric Acid HMG CoA Reductase Inhibitors Bile Acid Resin 72. The underlying genetic disorder of lipoprotein metabolism is secondary to A. B. C. D. E. Defects in the gene that encodes the LDL receptor Defect in apo B-100 ligand Deficiency of Lipoprotein Lipase Deficiency of cholesteryl ester transfer protein Increase in apo CII expression A 75 y/o man is referred for evaluation of erectile dysfunction (ED). He has experienced increasing difficulty achieving erections over the past 5 years. He is happily married; but he has noticed a mild decrease in his libido. His past history is notable for diabetes for the past 9 years, controlled with diet, and benign prostatic hyperplasia (BPH), for which he is being treated with an alpha-adrenergic blocker. He is taking no other medications.He has noticed an increase in headaches, which he has attributed to increased stress. He denies any change in his vision. On physical examination he has a body mass index (BMI) of 23 kg/m2 and a BP of 140/90 mmHg. He is well virilized with no gynecomastia and has a testicular volume of 20 mL bilaterally. Rectal examination demonstrates a mildly enlarged prostate. He has normal pedal pulses and no evidence of neuropathy. Visual fields are full to confrontation. Laboratory testing reveals the following: Total testosterone = 147 ng/dL and 185 ng/dL (280-1050) on two occasions; LH = 4 mIU/mL (3-15); FSH= 5.3 mIU/mL 3-18); and a prolactin=71.9 ng/ml (5-20) His hematocrit 36.8 % (Nl 32-45) with normal indices. Prostate Specific Antigen (PSA) =0.2 ng/mL (< 4.0) and HbA1C=6.0% (3.5-5.5). bone densitometry (DXA) demonstrates a T score of –2.2 at the L-S spine (nl> -1.0) and –2.1 at the hip (nl> -1.0). 73. What is the most likely cause of this patient’s ED? A. B. C. D. E. Hypogonadism Diabetic neuropathy Vascular disease Anemia of chronic disease Possible contribution of several or all of the above. 74. Which of the following would be least helpful as you evaluate this patient’s status? A. B. C. D. E. TRH stimulated prolactin determination Pituitary MRI scan Serum cortisol Thyroid function tests Serum hGH and IGF-1 levels 75. What treatment options would you propose? A. B. C. D. E. Immediate referral to a neurosurgeon Phophodiesterase inhibitors (Viagra/Levitra/Cialis) Testosterone replacement Bromocriptine or other dopamine agonist Combination of testosterone replacement and PDE inhibitor. JS is a 46 year old woman, who is the vice principal of an elementary school. She weighs 192 lbs. and is 5’4” tall (BMI=33.0). She currently has normal blood pressure and lipids, but she was recently diagnosed with type 2 diabetes. She has tried to loose weight a number of times, but nothing has really worked for her. 76. Which of the following are NOT goals for prevention of diabetes complications? A. B. C. D. E. Reduce weight Control glucose Control lipids Use preventive practices for eyes, kidneys and feet Control blood pressure 77. Which of the following nutrients should be minimized for diet therapy for a diabetic patient? A. B. C. D. E. Protein Carbohydrate Fat Fiber Alcohol 78. Which of the following is not usually considered to be the physician’s role in clinical diet counseling for a diabetic patient? A. B. C. D. E. Assess the patient’s motivation Teach the patient about the necessary diet changes Assess the patient’s compliance with diet recommendations Reinforce the advice from other team members All of the above 79. Known nutrition related risk factors for development of Type 2 diabetes include: A. B. C. D. E. Intake of carbohydrate Excess intake of high glycemic index foods Early introduction of high glycemic index foods Exposure to cow proteins Vegetable protein intake PR is a 40 year old woman, who is 5’5” and 168 pounds (BMI = 28 Kg/m2). Her 75 g glucose tolerance test showed that she is glucose intolerant, but she does not meet the criteria for diabetes. 80. In consideration of diet to prevent diabetes for PR, the glycemic index of foods might be considered. Glycemic index A. Is a mechanism to determine which carbohydrate sources are most nutritious. B. Compares the glycemic response curve of a food to that of white bread. C. Compares all foods to the chemical structure of white bread. D. Is based on the concept that all carbohydrates evoke the same metabolic response. E. Is the only characterisic of food that is of clinical relevance. 81. Nutritional care for PR during her efforts to prevent diabetes will likely involve A. Tight management of all nutrients. B. Establishment of a consistent amount of protein throughout the day. C. Identification of a caloric level that will allow her to lose weight. D. Establishment of consistent amount of fat day-to-day. E. Any two of the above. 82. Known nutrition related risk factors for development of Type 1 diabetes include A. B. C. D. E. Intake of carbohydrate Intake of high glycemic index foods Early introduction of high glycemic index foods Exposure to cow proteins Exposure to toxins in breast milk A 25 year old woman is brought to the Emergency Room by her husband. He reports that she has been feeling weak and lethargic for about a week. This has progressively worsened and, for the past 2 days, she has had nausea and vomiting. She is a fourth grade teacher, and several of her students have been sick recently with a flu-like illness. On review of systems by the ER physician, a history is obtained indicating that the patient noted progressively increasing thirst starting approximately one week ago and has been passing large volumes of urine, which require her getting up several times during the night. The patient’s last menstrual period was approximately 3 weeks ago and, when asked about this, she noted that she and her husband had decided to have a family and therefore stopped using birth control about 2 weeks ago. Questions regarding the family history reveal that her mother and a paternal aunt developed diabetes when they were middle-aged. There is no other known family history of chronic diseases. On examination, the patient is noted to be somnolent but responsive to questions. The vital signs are: Hgt. 5’6”, Wgt 124 lbs, BMI 19.5 Kg/m2 Pulse 120 BPM and regular BP 95/60 mmHg Respirations 20/minute with deep inspiration and expiration. Temperature 37o C Her breath is noted to have a fruity odor. Initial laboratory findings include: Blood glucose 950 mg/dl (Nl < 100) Serum ketones large (Nl Negative) Arterial pH 7.15 (Nl 7.36-7.44) 83. The most likely diagnosis to explain the metabolic state of this patient is: A. B. C. D. E. Influenza Type 1 diabetes Type 2 diabetes MODY diabetes Gestational diabetes 84.The best test to confirm the specific disease responsible for the metabolic abnormalities in this patient would be: A. B. C. D. E. Influenza hemaglutinins A determination of plasma hemoglobin A1c (HbA1c) A plasma insulin level A glucose tolerance test Serum titers of anti-insulin, anti-GAD, and anti-islet antibodies 85. Of the following, the most appropriate longterm treatment for this patient’s condition would be: A. B. C. D. E. Sulfonylurea Metformin Thiazolidinedione Basal-bolus insulin regimen Diet and exercise only A 50 year old man is admitted to the hospital for elective knee surgery. His medical history is unremarkable except for long-standing obesity, with a current body mass index of 35 kg/m2. His maximum waist circumference is 44 inches. As part of routine blood testing on the morning of his operative procedure, his fasting blood glucose level is noted to be 110 mg/dl. One month later, although asymptomatic, he is evaluated with a glucose tolerance test (75 gm oral glucose after overnight fasting). The blood glucose values are as follows: Fasting 112 mg/dl (< 100) 30 minute 154 mg/dl 1 hour 202 mg/dl 2 hour 225 mg/dl (< 140) 3 hour 178 mg/dl 86. The most likely diagnosis in this patient is: A. B. C. D. E. Normal glucose tolerance Type 1 diabetes Type 2 diabetes Impaired fasting glucose MODY diabetes 87. t is considered important to screen this patient for other features that may be used to diagnose the Metabolic Syndrome. Which of the following determinations is not required to establish this diagnosis: A. B. C. D. E. Blood pressure Fasting triglycerides LDL cholesterol Waist circumference Fasting blood sugar . 88. Of the following agents, which would be the least likely to cause weight gain and hypoglycemia: A. B. C. D. E. Sulfonylurea Metformin Thiazolidinedione Basal-bolus insulin regimen All cause weight gain and hypoglycemia A 39 year old woman is seen by her primary care physician for a routine visit and gynecological exam. She has a history of being “heavy” since adolescence. She delivered her second child 2 years previously and comments to her physician that she “never lost the weight” after that pregnancy and has gained weight since. She is 5 feet 2 inches tall and weighs 170 lbs (BMI 31 kg/m2). She works as a bank teller and does not regularly exercise. Her medical history and review of systems are otherwise unremarkable. 89. Her body weight status would be classified as: A. B. C. D. E. Normal weight for height Overweight Obesity Morbid obesity Gestational 90. Her body weight status is associated with an increased risk of all of the following EXCEPT : A. Diabetes mellitus B. Hypertension C. Lung cancer D. Hyperlipidemia E. Breast Cancer A 36-year-old man with three children 12, 10 and 8 years old, complains of headaches for the past 3 months, double vision for 6 months and diminished libido for over a year. On physical exam he is 5' 6" tall, weighs 142 lbs. and has normal blood pressure. He seems to have some loss of peripheral vision and small soft testicles. 91. Of the following, which is most likely to be helpful in determining the cause of his small soft testicles? A. B. C. D. E. His performance on the Oppenheimer test of testicular function. Serum levels of the hypothalamic releasing factor dopamine. Circulating levels of total testosterone Insulin like Growth Factor 2 levels A Karyotype 92. Of the following, which would be a likely cause of the clinical scenario outlined above. A. B. C. D. E. A non-secretory microadenoma of the pituitary. A growth hormone releasing hormone secreting hamartoma of the hypothalamus. A dihydrotestosterone secreting tumor of the testicle. A micro prolactinoma A macro prolactinoma 93. Of the following, which pharmacologic intervention may possible is helpful? A. B. C. D. E. Pulsatile gonadotropin releasing hormone administration. A dopamine agonist. A dopamine antagonist. Prostate specific antigen immunotherapy. Growth hormone administration. A 26 y/o male presents for the evaluation of infertility. He and his 27 y/o wife have been having unprotected intercourse for 2 years without a conception. Your evaluation leads to a diagnosis of hypogonadotropic hypogonadism due to Kallman Syndrome. 94. Which treatment is likely to improve his fertility? A. B. C. D. E. Testosterone injections IM or subcutaneous FSH and hCG Cabergoline Aromatase inhibitors A combination of testosterone and hCG A 23 year old male from a rural community in Asia presents with a complaint of infertility. On questioning he also reports a low libido and erectile dysfunction. His past history is significant for mumps orchitis at age 19. On physical exam his testicles are small and firm. 95. Laboratory evaluation is likely to show: A. Low FSH, Low LH, low testosterone B. Azoospermia, normal FSH and LH C. Low testosterone, high sperm count D. High estrogen, Low LH E. High LH, High FSH, Low testosterone A 24-year old female patient with hypercholesterolemia is recommended to start dietary therapy. 96. The most plausible mechanism by which adding a plant sterol to her diet will effect this patient’s risk of a coronary event is: A. B. C. D. Lowers serum LDL cholesterol by decreasing the cholesterol content of bile Raises serum HDL cholesterol via Cholesterol Ester Transfer Protein pathway. Lowers serum Triglyceride levels by enhancing lipoprotein lipase activity Promotes nitrous oxide induced endothelial relaxation via a direct effect. 97. The diet recommended to lower this patient’s risk of coronary heart disease is: A. A diet high in n-6 polyunsaturated fats. B. A diet with less than 7% of calories from fat with the addition of a multivitamin, flaxseed, and 1 gram of fish oil supplements. C. A diet rich in fruits and vegetables, fish and nuts. D. A low carbohydrate, high fat diet. 98. A serious complication associated with benign prostatic hyperplasia is: A. Pain in the pelvis. B. Nocturia. C. Infection of the kidney. D. Impotence. E. Bleeding. 99. Gleason developed a grading system for prostatic carcinoma which involves: A. Ultrasonography and calculation of the total tumor volume. B. Analysis of the cytological features of the tumor cells. C. Use of serial sections to reconstruct the glandular architecture. D. 5 grades of tumor pattern numbered 1-to-5; a Gleason score was the sum of the two most frequent pattern numbers. E. Use of special stains to identify aneuploid cells. 100.Which of the following characteristics is associated with testicular seminoma: A. It is the most common testicular tumor. B. Tumor is often infiltrated with lymphocytes. C. It is extremely radiosensitive. D. The prognosis is excellent with appropriate therapy. E. All of the above. 101. Which of the following testicular tumor types is incorrectly associated with its cell type of origin: A. Leydig cell tumors arise from germ cells. B. Choriocarcinomas arise from germ cells. C. Yolk sac tumors arise from germ cells cells. D. Embryonal carcinomas arise from germ cells. E. Teratomas arise from germ cells. 102.Identify the common testicular cancer that is extremely radiosensitive: A. Embryonal carcinoma. B. Seminoma. C. Yolk sac tumor. D. Sertoli cell tumor. F. Leydig cell tumor. 103. Circulating FSH levels decrease following treatment with either leuprolide (Lupron) or goserelin (Zoladex). Indicate the mechanism for this decrease in FSH. A. Induction of FSH metabolizing enzymes B. Stimulation of renal FSH excretion C. Desensitization of pituitary GnRH receptors D. Inhibition of GnRH release E. Inhibition of GnRH synthesis 104. Which of the following agents inhibits adrenal steroid biosynthesis? A. B. C. D. E. Amiloride Mitotane Dexamethasone Pegvisomant Octeotride 105. In the treatment of Cushing's Syndrome, which of the following drugs acts both by inhibiting adrenal steroid biosynthesis, and also as an androgen antagonist? A) Ketoconazole B) Metyrapone C) Spironolactone D) Mitotane E) Aminoglutethimide