outline4278
advertisement

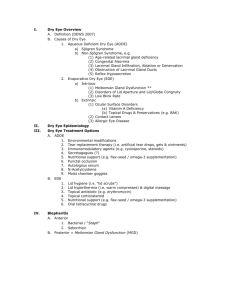
I. Diagnostic Tests Preferred by Renowned Practitioners A. The tests selected by 68 renowned practitioners for their first choice test, if only one test were allowed, in order of preference were (Korb et al, Cornea, 2000): 1. History 2. Fluorescein BUT (FBUT) 3. Fluorescein staining 28% 19% 13% 4. Rose bengal staining 5. Schirmer 6. Slit lamp exam 10% 8% 7% II. History A. Written questionnaires 1. McMonnies & Ho – The first validated questionnaire 2. Ocular Surface Disease Index © by Allergan 3. Authors’ comprehensive questionnaire B. Combined verbal questioning and written questionnaire – the optimal method III. Ocular Surface Staining – Fluorescein, Rose Bengal and Lissamine Green A. Why are stains used? B. Questions, controversies and specific actions of stains C. A new role for lissamine green D. A new vital stain IV. Lid Wiper Epitheliopathy (LWE) A. LWE is a recently described disorder correlated to dry eye symptoms with and without contact lenses. (Korb et al, 2002) B. Lid Wiper Defined: The aspect of the marginal conjunctiva of the upper eyelid that wipes the ocular surface during blinking. The epithelia of the lid wiper are squamous. C. Requires understanding of Kessing's space 1. Kessing’s space is the space separating the surface of the tarsal palpebral conjunctiva of the upper eyelid from the ocular surface. 2. The epithelial surface of the palpebral conjunctiva of Kessing's space is columnar, is not designed to rub or be rubbed, and is protected from contact with the ocular surfaces by Kessing’s space. D. Lid wiper diagnosis requires the use of a vital dye E. The premier dye to detect abnormalities of the ocular surface differs for the: 1. Conjunctiva — Rose bengal (Is Lissamine green a substitute?) 2. Cornea — Fluorescein 3. Lid Wiper — Not established but use of multiple dyes preferred F. Lid Wiper Epitheliopathy and Dry Eye Symptoms in CL Wearers (Korb et al, 2002) 1. 80% of symptomatic CL wearers demonstrated LWE - The correlation between symptomatic and asymptomatic contact lens wearers and lid wiper epitheliopathy was significant. G. LWE & Dry Eye Symptoms in Non-CL Wearers 1. 81% of symptomatic non-contact lens wearers demonstrated LWE. 2. Conclusion: A significant proportion of the population with dry eye exhibits lid wiper epitheliopathy. H. Conclusions 1. LWE is diagnosed by staining with specific techniques. 2. LWE is an alteration of the epithelia of the lid wiper and or their protective physiological coatings. 3. LWE is usually present with all dry eye states, particularly if of significance. AAO, Dallas, 2003 1 of 4 4. LWE is correlated to dry eye symptomatology, and particularly foreign body sensation, grittiness, and symptoms occurring with lid movement and blinking. 5. LWE is correlated to dry eye symptoms occurring with all contact lenses. 6. The columnar cells of the palpebral conjunctiva are not designed to rub. 7. Contact lenses must pay tribute to Kessing’s space. 8. The squamous epithelia of the lid wiper are designed for the movement and rubbing actions of the upper lid, but require an adequate tear film and lubrication to prevent LWE. 9. All dry eye states compromise the lid wiper. 10. Treatments for lid wiper epitheliopathy V. Biomicroscopic Evaluation A. Standard and novel techniques for dry eye diagnosis B. Foam and its significance VI. The Lipid Layer: Clinical Significance, Correlation To Dry Eye Disorders and Contact Lenses, and Meibomian Gland Dysfunction (MGD) A. Observation of lipid layer thickness (LLT) and characteristics (Interference Patterns) 1. Observation using conventional slit-lamp with specular reflection is of limited value. 2. Tearscope-plus™ (Keeler) – lipid layer evaluation a) Special tribute to Jean-Pierre Guillon for 15 years of research of the lipid layer and development of clinical instrumentation, Tearscope-plus™ 3. Authors’ interpretation of interference colors a) The reservoir is the lower meniscus; the spreading mechanism is blinking. b) Optimal (≥150 nm), good (90-135 nm), average (60-75 nm), thin (< 60 nm) c) The lipid layer is dynamic, not static. (Hamano 1979, Korb et al. 1994) 4. Author’s simplified approach to lipid layer classification and implications 5. Clinical procedure for Tearscope-plus™ B. Clinical significance of lipid layer findings and correlation to dry eye tests 1. “The placing of all types of soft lenses on the eye disrupts the tear film sufficiently to provide a significant increase in evaporation.” Cedarstaff & Tomlinson (1983) 2. Lipid layer (LL) correlated to evaporation and tear film stability. A four-fold increase in tear evaporation occurs if the LL is absent or not confluent. (Craig & Tomlinson, 1997) 3. The thicker the lipid layer, the greater the tear film stability (Craig & Tomlinson, 1995) 4. Correlation of LLT to FBUT & Schirmer (Isreb et al, 2003) 5. If LLT increased by treatment of meibomian glands, symptomatic relief of dry eye symptoms achieved (Korb & Greiner, 1994) 6. Meibomian gland dysfunction (MGD) and contact lens intolerance (Korb & Henriquez, 1980) C. Lipid layer thickness increase as a function of blinking (Korb et al., 1994) D. Lipid layer and contact lenses 1. Rigid gas permeable lenses: the consensus is that there is no LL 2. Hydrogel lenses: the consensus is that the LL is at best highly variable and abnormal 3. New hydrogel lenses AAO, Dallas, 2003 2 of 4 E. Meibomian gland (MG) evaluation and classification of Meibomian gland dysfunction (MGD) 1. Meibomian gland obstruction – the cause of the majority of MGD 2. Methods and classification of meibomian gland function and dysfunction 3. Foam – An important diagnostic phenomenon F. Lipid layer and meibomian gland treatment 1. MGD is related to contact lens intolerance. (Korb & Henriquez, 1980) 2. Meibomian therapy improves contact lens wear. (Paugh et al., 1990) 3. Lipid layer thickness increases following meibomian gland treatment. G. Lipid layer compromise, humidity, and summary of MGD treatments 1. The lipid layer may be compromised by many factors. 2. Vocations, including stress at prolonged near-point activities and computer tasks, may compromise blinking. This may result in lipid layer compromise leading to dry eye symptoms, and computer vision syndrome (computer induced eye discomfort syndrome). (Korb et al, 2003) 3. Humidity. The lipid layer thins in low ambient humidity, and is optimal in high (over 80%) relative humidity. (Korb, 2001) 4. Among the therapeutic possibilities are: improved blink efficacy, meibomian gland treatment (scrubs and expression) to improve the quantity and quality of secretions, warm compress treatment (Olson et al, 2003) surgical elevation of the lower lid, the use of tetracycline and similar medications, and the use of tear film additives. New medications, including salagen and topical cyclosporin A, also offer promise. H. Summary: 1. The lipid layer is dynamic, and its evaluation should be considered a dynamic rather than a static evaluation. The LL is not intended to be of uniform thickness. 2. LLT is correlated to dry eye disorders 3. Complete blinking (particularly if forceful) promotes meibomian secretion and increases LLT. Incomplete and/or infrequent blinking compromises meibomian gland function and the LL. A low blink rate with computer use leads to computer vision syndrome. 4. The LL (and tear film) of many individuals is inadequate to support the increased evaporation rate encountered with contact lens wear. 5. New lens materials are required to minimize evaporation phenomena and provide a more normal lipid layer on the outer surface of the lens. 6. Tear film additives require improvement to more closely replicate the tear film and specifically to include components that will improve the lipid layer. VII. Tear Film Stability, Break-up Time (BUT), and the Fluorescein BUT (FBUT) test. A. FBUT test should be the “first test” to determine if a tear film disorder is present. B. Criticized as inaccurate, unscientific and not reproducible, because an invasive test. C. Clinical procedures – “consensus” technique for measuring FBUT D. Non-invasive break-up time (NIBUT) (Mengher et al.) 1. Tearscope-plus™ (Keeler) and other instruments E. A new modification of the FBUT test, the DET test by Korb VIII. The Schirmer Test – The Original Intent (1903) was to measure reflex tear production. A. Questions – with or without anesthesia? Eyes open or closed? B. Recommendations, interpretations, Zone-quick (phenol red test) AAO, Dallas, 2003 3 of 4 IX. Clinical Strategy and Procedure for Diagnosis of Tear Film Disorders A. Pflugfelder et al. strategy and sequence of testing (1998) B. Bron strategy and sequence of testing (1997) C. Korb strategy and sequence of testing (2002) X. New Tests A. The high humidity test B. Differentiation of dry eye from allergic irritative disorders C. Mucin tests XI. Common Dry Eye Conditions A. Evaporative – obstructive meibomian gland dysfunction, blepharitis and inflammatory conditions B. Aqueous tear deficiency – keratoconjunctivitis sicca, Sjgren’s syndrome, pharmacologically induced, aging XII. Treatment of Dry Eye Disorders A. Meibomian gland dysfunction 1. Obstruction vs inflammatory vs infection B. Medications – tetracycline, doxycyclin C. New medications – salagen, Restasis (cyclosporin A), secretagogues D. Punctal occlusion E. Replacement therapies – androgens, estrogens, meibomian gland components F. Artificial tears – the past, the present, and the future 1. The past – pre-2003, artificial tear solutions provided very limited benefit. 2. The present – New modalities more effective (Endura, Systane) 3. The future – Replication of the tear film AAO, Dallas, 2003 4 of 4