Title: A New Paradigm of Dry Eye Etiology, Diagnosis and Treatment
1
Title: A New Paradigm of Dry Eye Etiology, Diagnosis and Treatment
Synopsis
This lecture will present a new paradigm for the etiology, diagnosis and treatment of dry eye and the evidence based medicine supporting this new paradigm, including the everexpanding role of meibomian gland dysfunction and the new concept of meibomian gland functionality. Emphasis will be placed on how this research provides a practical clinical approach for the diagnosis and management of dry eye patients in everyday practice. Diagnostic methods and treatment modalities and the authors’ new recommendations will be presented.
Introduction
- A framework of reference for a new paradigm
Is there a need for a new approach – is current understanding, diagnosis and treatment effective?
Is dry eye a single or multifactorial entity?
Is dry eye aqueous or lipid deficient? Is there a difference and does contemporary thinking adequately explain aqueous and/or lipid deficient states?
Why is there no correlation between signs and symptoms of dry eye?
What are the initiating factors for dry eye?
Are diagnostic methods adequate?
Do diagnostic tests allow diagnosis and/or explain aqueous and/or lipid deficient states?
What are the preferred diagnostic tests and what information do they provide?
What is role of blinking in dry eye?
Is posterior blepharitis synonymous with meibomian gland dysfunction?
Is current treatment adequate and are the physiological and pathological components of dry eye addressed?
Is dry eye a definitive disease or a rubric for many conditions?
Is there currently a level of anomalous clinical and scientific results which force questioning whether areas of present dry eye science and treatment are inadequate and force the adoption of a new paradigm? And what would that paradigm be?
Current understanding
Definition of Dry Eye:
Dry eye is a multi-factorial disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance and tear film instability with potential damage to the ocular surface. It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface. (DEWS report 2007)
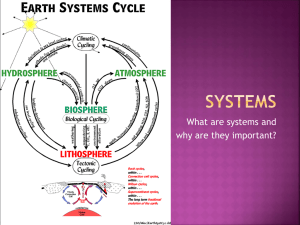
Contemporary models of the ocular surface
2
Etiopathogenic classification of dry eye – the 2007 DEWS report
The contemporary model of dry eye was established by 2007 DEWS report.
Systemic, behavioral, and environmental factors
Aqueous - deficient vs. evaporative dry
Meibomian Gland Dysfunction (MGD)
The diagnosis and classification of MGD is arbitrary
Hypersecretion (seborrheic)
Inflammatory MGD (pouting & plugging)
Infective MGD (glands and/or lids)
Tests for Dry Eye
Multifactorial disease presents a diagnostic dilemma
Multiple tests need to be considered
What can we test in the clinic?
Symptoms
– History, Symptom Questionnaires
Tear film stability – TBUT, aqueous secretion, lipid layer thickness, meniscometry
Ocular surface integrity
– staining (NaFl, RB, LG): cornea, conjunctiva, lid wiper,
Marx line
Meibomian gland function – diagnostic expression, meibometry
Tear film osmolarity – commercially available osmometer
Practical sequence of testing
Clinical history
Symptom Questionnaire
Interferometry if available
Slit lamp evaluation
FBUT (DET)
Ocular surface staining – combining stains
Schirmer testing
Lid and meibomian morphology
Meibomian expression
The Lid Wiper
A Missing Link in Dry Eye Diagnosis and Treatment
Lid Wiper defined – that aspect of the marginal conjunctiva of the upper eyelid that wipes the ocular surfaces during blinking
Windshield wiper analogy
Lid wiper epitheliopathy (LWE) defined
Diagnosis and grading of LWE
The use of stains in diagnosis
3
Correlation of LWE to dry eye signs and symptoms
Causative Factors of LWE – inflammation, lubrication, mechanical
The role of the lid wiper in ocular sensation and symptoms
Treatment of LWE
Meibomian Glands
Expanding role of meibomian glands: Meibomian gland dysfunction may be the leading cause of dry eye syndrome throughout the world.
Requires precise understanding and defining MGD and MG functionality
Distinguish between posterior blepharitis and MGD
Meibomian Gland Function
Functions of MG
– evaporation, tear film stability, vision, lubrication
What is a normal functional meibomian gland ?
Meibomian gland secretion dependent upon blinking
What us MGD ? A practical definition
How is MG functionality determined and quantified?
Specific MG activity at any given time?
Development of instrumentation for quantification of MG function.
Correlation between numbers of MG yielding liquid secretion (MGYLS) to dry eye symptoms?
The mean number of MGYLS in nasal, central & temporal regions of the lower eyelid
– a surprising finding
Time required for a single optimally secreting mg to recover after being drained of available oil
Diurnal variations in MG yielding liquid secretion
Variations in meibomian excreta with expression
Why meibomian gland obstruction? Obstruction of the meibomian gland ducts and orifices by keratinized epithelial plugs and other matter.
Expanded Classification of MGD should include: Obstructive MGD without obvious inflammation
Treatment of MGD
Warm compresses (WC)
Profiles for lid temperature in WC treatment
Scrubs
Expression – office treatment
Self-expression
Commercially available devices for MG treatment
Role of blinking
Medications
– topical and systemic
4
The Role of Interferometry
Instrumentation
Measurement of thickness and characteristics
Correlation of lipid layer thickness to dry eye symptoms
Correlation to meibomian gland expressibility and function
Role in diagnosis and treatment
A New Paradigm
Presents a new framework and perspective to understand the multifactorial nature of dry eye states and disease. The new model-paradigm explains many of the dichotomies and anomalous findings encountered in multifactorial dry eye states.
The model – paradigm includes the following sequelae of a decrease in lipid layer quality and thickness beyond below that threshold required to maintain tear film stability.
Implications of MGD
Decrease in lipid secretions
Evaporation increases
Decrease in aqueous layer thickness
Unstable tear film
Ocular surface compromised
Dry eye Inflammation
Lubricity compromised
Microtrauma
Lid Wiper Epitheliopathy
Triple Response of Lewis
Inflammation
Palpebral and Bulbar conjuctivitis
Posterior blepharitis
Sequelae of a compromised lipid layer
Does lacrimal gland up-regulate & overwork?
Diabetic & adrenal analogues
Treat MGD early to prevent
Inflammation of ocular surface
Lacrimal gland inflammation
LWE
Dry eye
5