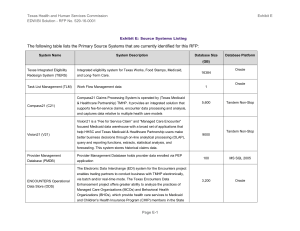
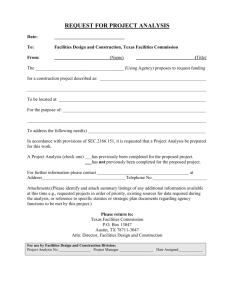
Data Collection Document - Texas Health and Human Services
advertisement

Texas Health and Human Services Commission RFP No. 529-13-0018 Attachment N: [Date] Data Collection Document The following content provides data collection specifications. Data Collection Specification - CV - Authorizations Collection Opportunity: CV - Client Visibility Across Programs Collection: DC149 - Authorizations Collection Description: Collect client authorization for programs and services across FFS and LTC programs. Data can be used to forecast future medical needs and financials. Currently, do not have access to Managed Care authorizations, but that could change with contract updates between the State and MCO. Functional Requirements: FR027 - Provide visibility to client authorization for Medicaid FR049 - Track health care timeliness, process of service delivery (including disease mgmt). FR065 - Measure and evaluate health impact of non-continuous service utilization Content: List By Client By Provider By Program By Location By Time Metrics: Number Clients Authorized for Program Service by Period, Estimated Potential Cost for Authorized Program Services by Period Topics: Service Authorization, Service Utilization Usage: Track health care timeliness, delivery and impact as it relates to client authorization for Medicaid services. Dimensions: Client, Program, Location, Time Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Retroactive rolling for up to 12 months [Eligibility and Enrollment] Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Provider @[Performing Provider, Provider Type/Specialty, Health Plan] Program @[Risk Group, Waiver Program] Location EDW/BI DD&I Page N-1 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Time @[Date of Authorization, Authorization Period] Major Source Systems:* Compass 21 (228 Tables, 2624GB) SAS (23 Tables, 7GB) Minor Source Systems:* Additional Data Sources: Leveraged Collections: Program Enrollment by Client Collection Provider Collection User Groups: DADS Budget Analysts DFPS Analysts HHSC IT MFADS Users SDS System Forecasting Vendor Drug Program Status: New EDW/BI DD&I Page N-2 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - CV - Churn Collection Opportunity: CV - Client Visibility Across Programs Collection: DC099 - Churn Collection Description: Periodically identify clients who have changes in eligibility, enrollment, and authorization across the enterprise then summarize and transform this information to produce churn Functional Requirements: FR024 - Trend client enrollment / disenrollment across programs and risk groups. FR025 - Investigate client churn by program or risk group. FR026 - Classify clients by disenrollment reasons to trigger intervention and/or alternate program placements Content: List By Client By Program By Time Metrics: Number of Clients Enrolling by Month, Number of Clients Disenrolling by Month, Number of Eligible Clients by Month, Ranked Reasons for Disenrollment, Ranked Reasons for Topics: Client Enrollment Usage: Assess course of changes on an individual and aggregate basis to ascertain reasons for changes: member communication issues, policy changes, changes in client residence or health status, or fraud and abuse are some potential reasons. Initiate processes to follow up on agency and enterprise service quality issues, forward potential fraud and abuse to OIG. Dimensions: Client, Program, Time Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Program @[Risk Group, Waiver Program, Dis/Enrollment Code] Time @[Date of Service, Fiscal Month, Fiscal Quarter, Fiscal Year] Major Source EDW/BI DD&I Page N-3 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Systems:* Compass 21 (228 Tables, 2624GB) Encounters (64 Tables, 356GB) MAXSTAR - MAXIMUS (Sizing TBD) TIERS (262 Tables, 448GB) Minor Source Systems:* ASKIT (356 Tables, 50GB) CMS/ICF/MR PRV PMT (90 Tables, 10GB) HEART (ALHQ/HQ) (300 Tables, 16GB) SAVERR (363 Tables, 1GB) Additional Data Sources: Alignment of EHR Data Elements CHIP Eligibility Codes and Descriptions SNAP SURS Texas Department of Justice Medical Records Leveraged Collections: Authorizations Collection Client Personal Cross-Reference Program Enrollment by Client Collection User Groups: DADS Budget Analysts DFPS Analysts HHSC IT MFADS Users SDS THSteps Status: EDW/BI DD&I Updated Page N-4 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - CV - Client Composite Eligibility Collection Opportunity: CV - Client Visibility Across Programs Collection: DC069 - Client Composite Eligibility Collection Description: Collect information on Client eligibility across programs including those outside of Medicaid (i.e. Medicare). Functional Requirements: FR022 - Track client eligibility across all programs included in TIERS FR063 - Integrate Medicaid and Medicare data for dual-eligible population. FR059 - Provide integrated visibility of drugs dispensed to Medicaid/Medicare dual eligibles. Content: List By Client (Eligible) across Programs By Time Metrics: Count of Eligible Clients, Number of Clients Enrolled in related Medicaid and Medicare Programs, Percent of Clients with continuous care by period, Percent of Continuous Care by Client over Time, Percent of Continuous Care by Client by Program Topics: Client Dual Eligibility Usage: Enable monitoring of client eligibility across all Medicaid programs. Integrate Medicaid data with Medicare data to improve visibility of client services. Dimensions: Client, Program, Time Frequency: Continuous where possible, otherwise daily Periodicity: Retroactive rolling for up to 12 months [Eligibility and Enrollment] Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Program @[Risk Group, Waiver Program] Time @[Enrollment Month, Fiscal Month, Fiscal Quarter, Fiscal Year] EDW/BI DD&I Page N-5 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Major Source Systems:* Compass 21 (228 Tables, 2624GB) Encounters (64 Tables, 356GB) TIERS (262 Tables, 448GB) Minor Source Systems:* HEART (ALHQ/HQ) (300 Tables, 16GB) Additional Data Sources: BME File CHIP Eligibility Codes and Descriptions Medicare Eligibility Leveraged Collections: Client Personal Cross-Reference Program Enrollment by Client Collection User Groups: DADS Budget Analysts DFPS Analysts HHSC Actuarial Analysis HHSC IT MFADS Users SDS System Forecasting THSteps TMHP Vendor Drug Program Status: EDW/BI DD&I New Page N-6 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - CV - Cohort Collection Opportunity: CV - Client Visibility Across Programs Collection: DC151 - Cohort Collection Description: Collection of utilization data for custom client cohort aggregations as defined by policy Subject Matter Experts. Functional Requirements: FR005 - Compare rates & costs for a client cohort within/across programs FR007 - Monitor service utilization by program, risk group, or cohort. FR083 - Perform geographic and/or demographic analysis of client drug utilization. FR012 - Determine when to modify existing programs or design a new waiver based on drug data. Content: List By Client (Client-demographic, Client-geographic), By Program, By Service, By Time Metrics: Average Cost by Custom Client Aggregation, Average Cost by Program Topics: Service Utilization Usage: Enable comparison of rates and costs for ad hoc client groupings within and across programs. Facilitate monitoring of service utilization by Risk Group, Program or custom Cohort. Allow analysis using geographic and demographic criteria associated with clients and services to help determine trends in program and service usage. Dimensions: Client, Program, Service, Time Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Program @[Risk Group, Waiver Program] Service @[Diagnosis, Procedure] Time @[Date of Service] Major Source EDW/BI DD&I Page N-7 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Systems:* ACS PCRA-VDP (Sizing TBD) CARE (17 Tables, 7GB) Compass 21 (228 Tables, 2624GB) Encounters (64 Tables, 356GB) SAS (23 Tables, 7GB) Minor Source Systems:* MEHIS (Sizing TBD) Additional Data Sources: Standard Measurement Libraries Leveraged Collections: Client Personal Cross-Reference Utilization Timeline by Client Collection User Groups: DADS Budget Analysts DFPS Analysts HHSC IT MFADS Users SDS System Forecasting THSteps TMHP Vendor Drug Program Status: New EDW/BI DD&I Page N-8 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - CV - Program Enrollment by Client Collection Opportunity: CV - Client Visibility Across Programs Collection: DC150 - Program Enrollment by Client Collection Description: Collect client enrollment for programs and services across Medicaid programs. Functional Requirements: FR081 - Perform geographic and/or demographic analysis of client access to care. FR072 - Discover duplication based on enrollment in the integrated eligibility systems. FR076 - Implement enterprise view across agencies of case management portfolio. FR077 - Monitor drug use for clients in concurrent/complex case management programs. FR080 - Perform geographic and/or demographic analysis of clients. FR024 - Trend client enrollment / disenrollment across programs and risk groups. FR004 - Provide capability to share data with other states for disaster response. FR006 - Monitor [cost] impact of migration between programs and services (including both internal and external as available) FR005 - Compare rates & costs for a client cohort within/across programs FR023 - Provide visibility to client enrollment for all Medicaid programs Content: List By Client By Location By Program Metrics: Number of Enrolled Clients Topics: Program, Client Enrollment Usage: Enable forecasting of future medical needs and financials based on Client program enrollment. Improve Case Management views across Programs and Agencies. Compare Client population and access to related Programs and services by demography and geography. Dimensions: Client, Location, Program Frequency: Continuous where possible, otherwise daily EDW/BI DD&I Page N-9 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA [Date] Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Location Program @[Risk Group, Program Waiver] Major Source Systems:* MAXSTAR - MAXIMUS (Sizing TBD) TIERS (262 Tables, 448GB) Minor Source Systems:* SAVERR (363 Tables, 1GB) Additional Data Sources: Program Codes and Descriptions SSA Addresses Leveraged Collections: Program Collection User Groups: DADS Budget Analysts DFPS Analysts DSHS Center for Health Statistics ECI Analysts HHSC IT HHSC Operations Support (Managed Care) MFADS Users Office of the Medical Director SDS System Forecasting THSteps TMHP Vendor Drug Program Status: EDW/BI DD&I New Page N-10 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - CV - Risk Groups Collection Opportunity: CV - Client Visibility Across Programs Collection: DC125 - Risk Groups Collection Description: Collect all episodes of care for individuals who meet HHS established Risk Group criteria (by Program). Integrate charges/costs, procedures/treatments, and prescriptions. Accumulate costs and align and track individuals’ episodes of care for frequency and severity of diagnoses (e.g. preventive and maintenance office visits versus hospital). Admissions and catastrophic Functional Requirements: FR007 - Monitor service utilization by program, risk group, or cohort. FR024 - Trend client enrollment / disenrollment across programs and risk groups. FR025 - Investigate client churn by program or risk group. FR086 - Provide consistent, integrated reference data (e.g., programs/waivers, risk groups, providers, drugs) to support: MCO oversight, regulatory reporting, and forecasting. Content: List By Client By Program Metrics: Number of Risk Group Clients, Projected Number of Risk Group Clients Topics: Risk Groups, Service Utilization Usage: Establish baselines for Risk Groups. Use service utilization data to define Risk Group profiles and trends. Compare courses of treatment for Risk Groups with established quality of care standards, and evidence-based protocols. Identify providers who may need education regarding updated standards of care for high risk and chronic conditions. Dimensions: Client, Program Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Program @[Risk Group, Waiver Program] EDW/BI DD&I Page N-11 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Major Source Systems:* TIERS (262 Tables, 448GB) Minor Source Systems:* HEART (ALHQ/HQ) (300 Tables, 16GB) Additional Data Sources: Leveraged Collections: Client Personal Cross-Reference User Groups: DADS Budget Analysts DFPS Analysts ECI Analysts HHSC IT MFADS Users SDS System Forecasting THSteps TMHP Vendor Drug Program Vision 21 Users Status: EDW/BI DD&I New Page N-12 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - CV - Unduplicated Count Collection Opportunity: CV - Client Visibility Across Programs Collection: DC076 - Unduplicated Count Collection Description: Collect data to produce periodic unduplicated counts of eligible individuals by program and/or Texas and MSIS Type Program codes, along with any other groupings regularly used for internal or CMS reporting. Maintain additional unduplicated counts that apply retroactive eligibility counts to the same groupings. Functional Requirements: FR002 - Create consistent and readily available per capita program denominators FR003 - Determine availability in comparable programs (Medicaid) Content: List By Program across Time Metrics: Count of Eligible and/or Enrolled Clients by Program, Risk Group or Cohort Topics: Program, Client Enrollment Usage: Provide easily accessible statistics for use in various program reporting and forecasting Dimensions: Program, Time Frequency: Continuous where possible, otherwise daily Periodicity: Retroactive rolling for up to 12 months [Eligibility and Enrollment] Security: None - Contains Program Aggregates Only Historical Retention: In perpetuity Granularity: Program @[Type Program Code, Risk Group, Waiver Program] Time @[Member Month, Fiscal Month, Fiscal Quarter, Fiscal Year] Major Source Systems:* Compass 21 (228 Tables, 2624GB) TIERS (262 Tables, 448GB) Minor Source Systems:* EDW/BI DD&I HEART (ALHQ/HQ) (300 Tables, 16GB) Page N-13 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Additional Data Sources: Leveraged Collections: Program Collection Program Enrollment by Client Collection User Groups: DADS Budget Analysts DFPS Analysts HHSC IT MFADS Users SDS System Forecasting THSteps TMHP Vendor Drug Program Status: EDW/BI DD&I Updated Page N-14 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - SD - Cost Collection Opportunity: SD - Service Delivery (Episodes of Care) Collection: DC104 - Cost Collection Description: Maintain periodic running totals by client of paid claims across all claim types including actual payouts as well as cost estimated managed care encounters. Maintain separate parallel totals of premiums and/or capitation payments attributable at individual levels. Contains a mapping for Fee for Service costs and Capitated Costs. Functional Requirements: FR005 - Compare rates & costs for a client cohort within/across programs FR006 - Monitor [cost] impact of migration between programs and services (including both internal and external as available) FR044 - Track cost of care across programs and providers FR052 - Track health outcomes by services and cost. FR054 - Identify what ought to be the norms for programs and services. FR009 - Benchmark Medicaid prices/costs/rates for comparisons within an agency and across programs with historical data. FR042 - Track and analyze differences in reimbursement units of service, e.g., time (day, hourly, fifteen minutes, encounter, etc.) FR011 - Improve ability to predict and manage the impact of changes to programs and service delivery models. FR051 - Track client quality of life linked to services and cost and vulnerability. FR088 - Compare Medicare with Medicaid providers Content: List By Client (Demographic), By Program, By Service, By Diagnosis, By Period [sum(quantity), sum(cost)] Metrics: Quantity, Actual Cost, Rate, Cost by Reimbursement Unit Topics: Cost, Service Utilization, Episodes of Care Usage: Enable tracking of costs by individual, and by identifiable groupings such as program, TP codes, primary diagnosis code (for LTC), and permit the identification of cost outliers. Compare actual costs of FFS versus Managed Care by Diagnosis, Demographic Groupings, Geography, etc. Identify candidates for PCCM, lock-in, other forms of Case Management. Dimensions: Client, Program, Service, Time EDW/BI DD&I Page N-15 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: In perpetuity Granularity: Client Program @[Risk Group, Waiver Program, Benefit Plan] Service @[Diagnostic Level] Time @[State Fiscal Month, Quarter, Year, Biennium] Major Source Systems:* ACS PCRA-VDP (Sizing TBD) CARE (17 Tables, 7GB) Compass 21 (228 Tables, 2624GB) Encounters (64 Tables, 356GB) PPS (42 Tables, 1075GB) SAS (23 Tables, 7GB) Minor Source Systems:* MEHIS (Sizing TBD) Additional Data Sources: Medicare Part A Claims Medicare Part B Claims Medicare Part C Claims Medicare Part D Claims OASIS Standard Measurement Libraries Leveraged Collections: Episode of Care Collection User Groups: DADS Budget Analysts DFPS Analysts HHSC IT MFADS Users SDS System Forecasting THSteps EDW/BI DD&I Page N-16 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 TMHP Vendor Drug Program Status: EDW/BI DD&I Replacement Page N-17 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - SD - DME and Supplies Collection Opportunity: SD - Service Delivery (Episodes of Care) Collection: DC121 - DME and Supplies Collection Description: Collect Durable Medical Equipment and Supplies data from Claims and Encounters. Combine standard measurement libraries and reference categorization data. Functional Requirements: FR070 - Detect, delineate, and track potential waste and inappropriate use (Drugs and Supplies). FR071 - Detect inappropriate use with respect to “once per lifetime” care episodes. Content: List By Client By Provider By Service By Procedure By Product, By Time Metrics: Units per Period, Excess per capita, Supplies Consumed versus Authorized, Excess Cost Topics: Service Utilization, DME Usage: Enable tracking of Durable Medical Equipment through Episode of Care integration. Allow for identification of inappropriate DME and/or supplies utilization. Dimensions: Client (Authorization), Service, Product, Time, Provider Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Service @ [Procedure] Product @ [Unit] Provider @ [Performing Physician] Time @ [Any Level] Major Source Systems:* CARE (17 Tables, 7GB) Compass 21 (228 Tables, 2624GB) EDW/BI DD&I Page N-18 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Encounters (64 Tables, 356GB) SAS (23 Tables, 7GB) Minor Source Systems:* Additional Data Sources: DME Conformance DME Registry Medicare Part A Claims Medicare Part B Claims Medicare Part C Claims Medicare Part D Claims Product Categories Supplies Conformance Leveraged Collections: Drug Category Collection Episode of Care Collection Provider Collection User Groups: DADS Budget Analysts DFPS Analysts HHSC IT HHSC Operations Support (Managed Care) Office of the Medical Director THSteps Status: Updated EDW/BI DD&I Page N-19 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - SD - Episode of Care Collection Opportunity: SD - Service Delivery (Episodes of Care) Collection: DC103 - Episode of Care Collection Description: Collect and integrate normalized service delivery details and costs by diagnostic, procedural, demographic and geographic groups across all service delivery modes (from claims and encounter data). Functional Requirements: FR021 - Integrate service data from the All Payers database (THCIC). FR026 - Classify clients by disenrollment reasons to trigger intervention and/or alternate program placements FR013 - Design more proactive services and programs given wider view of healthcare delivery over time FR034 - Track service delivery to client by provider including parent company. FR035 - Track service delivery across programs by provider including parent company FR036 - Compare episodes of care by provider type, specialty, or health plan. FR040 - Parse encounters and claims data into Episodes of Care service categories. FR041 - Expose streams of care episodes that cross programs or departments or agencies FR045 - Identify clients with a specified primary diagnoses over a specific period of time. FR046 - Detect clients with diagnoses indicating the need for disease management FR047 - Identify clients who have frequent service or provider changes to determine cause. FR050 - Integrate lab data with client records. FR052 - Track health outcomes by services and cost. FR053 - Provide the ability to predict and prevent negative outcomes, including data to help assess client quality of life FR055 - Map prescription drug stream to episode of care services data. FR056 - Collect physician administered drug data. EDW/BI DD&I Page N-20 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] FR057 - Monitor drugs prescribed by client, diagnosis, program, service, and provider. FR058 - Analyze drug delivery by provider. FR059 - Provide integrated visibility of drugs dispensed to Medicaid/Medicare dual eligibles. FR060 - Identify indicators of aberrant or irregular client use of drugs. FR062 - Monitor duration and continuity of care. FR064 - Identify, measure and evaluate health impact of non-continuous eligibility or enrollment (Medicaid programs) FR065 - Measure and evaluate health impact of non-continuous service utilization FR069 - Detect, delineate, and track potential waste and inappropriate use (Services). FR070 - Detect, delineate, and track potential waste and inappropriate use (Drugs and Supplies). FR073 - Discover duplication of services based on service utilization. FR074 - Discover duplication of services based on drug utilization. FR075 - Discover duplication across Texas healthcare services; not just Medicaid programs. FR078 - Compare client outcomes across case management programs. FR082 - Compare services used against services available by client & location. FR084 - Compare treatments for similar diagnoses by geography or demography FR086 - Provide consistent, integrated reference data (e.g., programs/waivers, risk groups, providers, drugs) to support: MCO oversight, regulatory reporting, and forecasting. FR071 - Detect inappropriate use with respect to “once per lifetime” care episodes. FR051 - Track client quality of life linked to services and cost and vulnerability. FR054 - Identify what ought to be the norms for programs and services. FR063 - Integrate Medicaid and Medicare data for dual-eligible population. FR066 - Integrate Vendor drug by incorporating drugs prescribed through private insurance providers. EDW/BI DD&I Page N-21 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] FR067 - Integrate health data from private insurers. FR068 - Integrate data about veterans who are also clients from the VA FR087 - Compile a history of care pertaining to EPSDT (THSteps) requirements FR049 - Track health care timeliness, process of service delivery (including disease mgmt). FR011 - Improve ability to predict and manage the impact of changes to programs and service delivery models. FR039 - Support coordination of care between successive care providers or programs FR019 - Align to State Medicaid Health IT Planning (SMHP) FR079 - Identify specific services by location. FR012 - Determine when to modify existing programs or design a new waiver based on drug data. FR103 - Provide visibility to clients by providers. FR099 - Provide history in accordance with retention requirements FR102 - Provide the ability to compare outcomes in institutional and noninstitutional providers FR005 - Compare rates & costs for a client cohort within/across programs FR006 - Monitor [cost] impact of migration between programs and services (including both internal and external as available) FR007 - Monitor service utilization by program, risk group, or cohort. FR008 - Anticipate future needs for programs by analysis of trends in services FR009 - Benchmark Medicaid prices/costs/rates for comparisons within an agency and across programs with historical data. FR010 - Detect outlier client cohorts and rates that merit new programs/waivers FR043 - Assess comparable services within and across all agencies FR044 - Track cost of care across programs and providers FR061 - Provide a single view of Medicaid services across programs/agencies. FR088 - Compare Medicare with Medicaid providers Content: EDW/BI DD&I List By Client [client demographic] Page N-22 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] By Provider [Place of Service] By Program By Service By Time Metrics: Episode Duration, Episode Cost Topics: Episodes of Care, Service Utilization Usage: Provide conformed views of treatment across service utilization to enable outcomes measurement and comparison across Clients, Programs and Providers. Dimensions: Client, Provider, Program, Service, Time Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Provider @[Performing Provider, Provider Type/Specialty, Health Plan] Program @[Risk Group, Waiver Program] Service @[Diagnosis, Procedure] Time @[Date of Service, Episode Duration] Major Source Systems:* ACS PCRA-VDP (Sizing TBD) CARE (17 Tables, 7GB) Compass 21 (228 Tables, 2624GB) Encounters (64 Tables, 356GB) KIDS (18 Tables, 18GB) SAS (23 Tables, 7GB) Minor Source Systems:* ASKIT (356 Tables, 50GB) CMIS - CSHCN (522 Tables, 1000GB) CRS (Tables TBD, 500GB) ImmTrac (100 Tables, 1024GB) MEHIS (Sizing TBD) MTS (Tables TBD, 40GB) TKIDS (140 Tables, 35GB) TWICES (365 Tables, 70GB) EDW/BI DD&I Page N-23 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Additional Data Sources: Alignment of Correlated Events Claims Parser for Drug Delivery Claims Parser for Services Client Identity Reconciliation and Merge Course Treatment Time-Line CPT-4 Procedure Codes DARS ECI Diagnostic Code Translators DME Conformance Drug Formulary Drugs to Diagnosis [External] DSHS TPC DSM-IV Codes and Descriptions Geocode Data (Stand alone) HCPCS Procedure Codes and Descriptions Health Care Coverage Time-Line HIX ICD-10 Diagnostic Codes and Descriptions ICD-10 Procedure Codes and Descriptions ICD-9 Procedure Codes and Descriptions Insurance Brokerage Data Mapping to Stages of Care Medicare Part A Claims Medicare Part B Claims Medicare Part C Claims Medicare Part C Claims Medicare Part D Claims Procedure Code Translators RDM Service Categories SNOMED (D Axis) Codes and Descriptions Standard Measurement Libraries State Data Center Population Data Supplies Conformance Texas Department of Education School Records Texas Procedure Codes and Descriptions Leveraged Collections: EDW/BI DD&I Cost Collection Page N-24 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 Provider Collection User Groups: DADS Budget Analysts DFPS Analysts DSHS Center for Health Statistics ECI Analysts HHSC IT HHSC Operations Support (Managed Care) MFADS Users Office of the Medical Director SDS System Forecasting THSteps TMHP Vendor Drug Program Vision 21 Users Status: EDW/BI DD&I Updated Page N-25 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - SD - Provider Performance Collection Opportunity: SD - Service Delivery (Episodes of Care) Collection: DC120 - Provider Performance Collection Description: Collect Episodes of Care data to assess the quality of service offered by Provider. Currently, this is largely based on definitions from Business Analysts. In the future, performance will be defined by Episode of Care outcomes. Functional Requirements: FR037 - Assess quality of service by provider. FR038 - Consolidate provider metrics. FR088 - Compare Medicare with Medicaid providers FR078 - Compare client outcomes across case management programs. FR029 - Create an integrated provider profile. FR102 - Provide the ability to compare outcomes in institutional and noninstitutional providers Content: List By Client By Provider By Program By Service By Time Metrics: Average Cost Per Procedure by Provider, Number of Clients Serviced Topics: Provider Performance, Episodes of Care Usage: Compare client outcomes and costs across programs by Provider to evaluate provider performance. Dimensions: Client, Provider, Program, Service, Time Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: In perpetuity Granularity: Client Provider @[Performing Provider, Provider Type/Specialty, Health Plan] Program @[Risk Group, Waiver Program] Service @[Diagnosis, Procedure] Time @[Date of Service] EDW/BI DD&I Page N-26 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Major Source Systems:* ACS PCRA-VDP (Sizing TBD) CARES (106 Tables, 351GB) Minor Source Systems:* HCS (INFO) (56 Tables, 5GB) Additional Data Sources: ASPEN Dartmouth Atlas DM Contract for Manageable Conditions Medicare Part A Claims Medicare Part B Claims Medicare Part C Claims Medicare Part D Claims Provider Analytic Categories Provider Taxonomy Leveraged Collections: Episode of Care Collection User Groups: DADS Budget Analysts DFPS Analysts HHSC IT MEHIS Analysts MFADS Users Office of the Medical Director SDS System Forecasting THSteps TMHP Vendor Drug Program Status: EDW/BI DD&I Updated Page N-27 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - SD - Utilization Timeline by Client Collection Opportunity: SD - Service Delivery (Episodes of Care) Collection: DC014 - Utilization Timeline by Client Collection Description: Collect service utilization data for all Clients over time. Maintain optimized datasets for client service use over time versus cost. Functional Requirements: FR006 - Monitor [cost] impact of migration between programs and services (including both internal and external as available) FR008 - Anticipate future needs for programs by analysis of trends in services FR017 - Identify caregivers and track status (e.g., age, health, availability to client, location) Content: List By Client By Program By Service By Location across Time Metrics: Number of Procedures by Member Month, Number of Clients by Diagnosis Related Group, Number of Clients by BETOS, Number of Procedures by BETOS Topics: Service Utilization Usage: Track Client Service utilization over time in order to identify trends and anticipate future client needs. Dimensions: Client, Program, Service, Location, Time Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Program @[Risk Group, Waiver Program] Service @[Diagnosis, Procedure] Location @[Place of Service] Time @[Date of Service] EDW/BI DD&I Page N-28 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Major Source Systems:* ACS PCRA-VDP (Sizing TBD) CARE (17 Tables, 7GB) Compass 21 (228 Tables, 2624GB) Encounters (64 Tables, 356GB) KIDS (18 Tables, 18GB) SAS (23 Tables, 7GB) Minor Source Systems:* ASKIT (356 Tables, 50GB) CRS (Tables TBD, 500GB) MEHIS (Sizing TBD) MTS (Tables TBD, 40GB) Additional Data Sources: Standard Measurement Libraries Leveraged Collections: Client Personal Cross-Reference User Groups: DADS Budget Analysts DFPS Analysts HHSC IT MFADS Users SDS System Forecasting THSteps TMHP Vendor Drug Program Status: EDW/BI DD&I Updated Page N-29 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - DI - Composite Drug Utilization Collection Opportunity: DI - Drug Integration (with Episodes of Care) Collection: DC106 - Composite Drug Utilization Collection Description: Combine drug utilization data from prescription, physician administered, and client direct procurement sources. Functional Requirements: FR077 - Monitor drug use for clients in concurrent/complex case management programs. Content: List By Client By Provider By Program By Service By Location By Drug By Time Metrics: Average number of prescriptions (Demographic), Percent of Program exceeding Utilization, Cost by Program Topics: Drug Utilization, Episodes of Care Usage: Allow for monitoring and analysis of client drug utilization based on the full universe of drugs dispensed by providers regardless of delivery method. Dimensions: Client, Provider, Program, Service, Location, Drug, Time Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Provider @[Performing Provider, Provider Type/Specialty, Health Plan] Program @[Risk Group, Waiver Program] Service @[Diagnosis, Procedure] Location @[Place of Service] Product @[Drug] Time @[Date of Service, Fiscal Month, Fiscal Year, Any Aggregate Level] Major Source Systems:* EDW/BI DD&I ACS PCRA-VDP (Sizing TBD) Page N-30 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Compass 21 (228 Tables, 2624GB) Encounters (64 Tables, 356GB) Minor Source Systems:* MEHIS (Sizing TBD) Additional Data Sources: Standard Measurement Libraries Leveraged Collections: Drug Category Collection User Groups: DADS Budget Analysts DFPS Analysts HHSC IT THSteps Status: EDW/BI DD&I Updated Page N-31 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - DI - Drug Utilization Category Collection Opportunity: DI - Drug Integration (with Episodes of Care) Collection: DC105 - Drug Utilization Category Collection Description: Collect drug utilization data by therapeutic categories. Compile statistics including cost by client, client characteristics, diagnosis, program, or medical provider. Functional Requirements: FR057 - Monitor drugs prescribed by client, diagnosis, program, service, and provider. FR058 - Analyze drug delivery by provider. FR060 - Identify indicators of aberrant or irregular client use of drugs. FR070 - Detect, delineate, and track potential waste and inappropriate use (Drugs and Supplies). FR074 - Discover duplication of services based on drug utilization. FR083 - Perform geographic and/or demographic analysis of client drug utilization. FR012 - Determine when to modify existing programs or design a new waiver based on drug data. FR059 - Provide integrated visibility of drugs dispensed to Medicaid/Medicare dual eligibles. FR009 - Benchmark Medicaid prices/costs/rates for comparisons within an agency and across programs with historical data. FR010 - Detect outlier client cohorts and rates that merit new programs/waivers FR011 - Improve ability to predict and manage the impact of changes to programs and service delivery models. Content: List By Client (Client Demographic, Client Characteristics) By Provider By Program BY Service By Location By Product (Product Category) By Time Metrics: Average number of prescriptions (Demographic), Percent of Program exceeding Utilization, Cost by Drug Category Topics: Service Utilization, Drug Utilization Usage: Enable analysis of Program, Client, and Provider dimensions across drug categories. Identify trends in drug utilization across Programs, EDW/BI DD&I Page N-32 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Demographics and Geography. Dimensions: Client, Provider, Program, Service, Location, Product, Time Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Provider @[Performing Provider, Provider Type/Specialty, Health Plan] Program @[Risk Group, Waiver Program] Service @[Diagnosis, Procedure] Location @[Place of Service] Product @[Drug Category, Drug] Time @[Date of Service, Fiscal Month, Fiscal Year, Any Aggregate Level] Major Source Systems:* ACS PCRA-VDP (Sizing TBD) Compass 21 (228 Tables, 2624GB) Encounters (64 Tables, 356GB) Minor Source Systems:* MEHIS (Sizing TBD) Orchard (Harvest) (211 Tables, 70GB) Additional Data Sources: Claims Parser for Drug Delivery Standard Measurement Libraries Leveraged Collections: Client Personal Cross-Reference Drug Category Collection User Groups: DADS Budget Analysts DFPS Analysts HHSC IT HHSC Operations Support (Managed Care) MFADS Users SDS EDW/BI DD&I Page N-33 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 System Forecasting THSteps TMHP Status: EDW/BI DD&I New Page N-34 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - DI - Drugs by Diagnosis Collection Opportunity: DI - Drug Integration (with Episodes of Care) Collection: DC108 - Drugs by Diagnosis Collection Description: Collect drug claims by Client and Provider associated with Episodes of Care by primary diagnosis and diagnostic group. Functional Requirements: FR055 - Map prescription drug stream to episode of care services data. Content: List By Client By Provider By Program By Service By Location By Product By Time Metrics: Aggregated Drug Utilization by Episode Diagnosis, Top 10 Drugs Utilized by Episode Diagnosis, Bottom 10 Drugs Utilized by Diagnosis Topics: Drug Utilization, Episodes of Care Usage: Analyze drug utilization to reveal trends by cohort based on Client characteristics and diagnosis. Reveal common and divergent drug delivery patterns. Dimensions: Client, Provider, Program, Service, Product, Time Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Provider @[Performing Provider, Provider Type/Specialty, Health Plan] Program @[Risk Group, Waiver Program] Service @[Diagnosis, Procedure] Location @[Place of Service] Product @[Drug] Time @[Date of Service, Fiscal Month, Fiscal Year, Any Aggregate Level] Major Source Systems:* EDW/BI DD&I Page N-35 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Minor Source Systems:* Additional Data Sources: Alignment of Correlated Events Drugs to Diagnosis [Internal] Drugs to Procedure [External] HIE Leveraged Collections: Drug Category Collection Episode of Care Collection User Groups: DFPS Analysts HHSC IT THSteps Status: Updated EDW/BI DD&I Page N-36 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - DI - High Utilization Collection Opportunity: DI - Drug Integration (with Episodes of Care) Collection: DC139 - High Utilization Collection Description: Collect all service utilization data, integrate industry standard norms to allow for outlier Functional Requirements: FR010 - Detect outlier client cohorts and rates that merit new programs/waivers FR054 - Identify what ought to be the norms for programs and services. FR069 - Detect, delineate, and track potential waste and inappropriate use (Services). FR060 - Identify indicators of aberrant or irregular client use of drugs. Content: List By Client By Provider By Program By Service By Time Metrics: Average number of ER Visits (Demographic), Percent of Program exceeding Utilization Topics: Service Utilization Usage: Enable benchmarking of service utilization over time to establish norms and identify outliers. Facilitate detection of potential fraud, abuse and waste. Dimensions: Client, Provider, Program, Service, Time Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Provider @[Performing Provider, Provider Type/Specialty, Health Plan] Program @[Risk Group, Waiver Program] Service @[Diagnosis, Procedure] Time @[Date of Service, Fiscal Month, Fiscal Year, Any Aggregate Level] Major Source EDW/BI DD&I Page N-37 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Systems:* ACS PCRA-VDP (Sizing TBD) CARE (17 Tables, 7GB) Compass 21 (228 Tables, 2624GB) Encounters (64 Tables, 356GB) PPS (42 Tables, 1075GB) SAS (23 Tables, 7GB) Minor Source Systems:* Additional Data Sources: Standard Measurement Libraries Leveraged Collections: Client Personal Cross-Reference User Groups: DADS Budget Analysts DFPS Analysts HHSC IT HHSC Operations Support (Managed Care) MFADS Users Office of the Medical Director SDS THSteps Status: EDW/BI DD&I New Page N-38 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - DI - Inappropriate Usage Collection Opportunity: DI - Drug Integration (with Episodes of Care) Collection: DC140 - Inappropriate Usage Collection Description: Collect all drug utilization data, integrate industry standard norms to allow for outlier analysis. Functional Requirements: FR054 - Identify what ought to be the norms for programs and services. FR069 - Detect, delineate, and track potential waste and inappropriate use (Services). FR060 - Identify indicators of aberrant or irregular client use of drugs. FR070 - Detect, delineate, and track potential waste and inappropriate use (Drugs and Supplies). FR071 - Detect inappropriate use with respect to “once per lifetime” care episodes. Content: List By Client By Provider By Program By Service By Product By Time Metrics: Estimated Cost of Inappropriate Service, Total Number of Inappropriate Encounters by Client, Percent of Clients with aberrant use by Program Topics: Drug Utilization Usage: Enable benchmarking of drug utilization over time to establish norms and identify outliers. Facilitate detection of potential fraud, abuse and waste. Dimensions: Client, Provider, Program, Service, Product, Time Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Provider @[Performing Provider, Provider Type/Specialty, Health Plan] Program @[Risk Group, Waiver Program] Service @[Diagnosis, Procedure] EDW/BI DD&I Page N-39 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Location @[Place of Service] Product @[Drug Category Drug] Time @[Date of Service] Major Source Systems:* ACS PCRA-VDP (Sizing TBD) CARE (17 Tables, 7GB) Compass 21 (228 Tables, 2624GB) Encounters (64 Tables, 356GB) SAS (23 Tables, 7GB) Minor Source Systems:* MEHIS (Sizing TBD) Additional Data Sources: HEDIS Medicare Part A Claims Medicare Part B Claims Medicare Part C Claims Medicare Part D Claims Standard Measurement Libraries Supplies Conformance Texas Preferred Drug List Leveraged Collections: Client Personal Cross-Reference Drug Category Collection Drugs by Diagnosis Collection Episode of Care Collection User Groups: DADS Budget Analysts DFPS Analysts HHSC IT HHSC Operations Support (Managed Care) MFADS Users Office of the Medical Director SDS THSteps Status: EDW/BI DD&I New Page N-40 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - CLH - Course of Treatment Collection Opportunity: CLH - Client Life History Collection: DC110 - Course of Treatment Collection Description: Collect episodes of care by individual for all stages of care for primary diagnoses and/or diagnostic groups, including costs, procedures, and prescriptions Functional Requirements: FR084 - Compare treatments for similar diagnoses by geography or demography FR087 - Compile a history of care pertaining to EPSDT (THSteps) requirements Content: List By Client By Service By Product By Time Metrics: Number of Visits, Frequency of visits, Average Length of Treatment Sequence for particular diagnoses or Diagnostic Groups Topics: Service Utilization, Episodes of Care, Drug Utilization Usage: Enable analysis and outcome measurement across providers and programs by diagnosis. Allow for comparison of treatment against established quality of care standards, and evidence-based protocols. Identify outliers by individual, provider, and Managed Care Organization. Dimensions: Client, Service, Product, Time Frequency: On-Request or Triggered or Subscription from Health Information Exchanges Periodicity: Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Service @[Diagnosis, Procedure] Product @[Drug] Time @[Date of Service] Major Source EDW/BI DD&I Page N-41 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Systems:* Minor Source Systems:* Additional Data Sources: Alignment of EHR Data Elements Leveraged Collections: Drug Category Collection Episode of Care Collection User Groups: DADS Budget Analysts DFPS Analysts DSHS Center for Health Statistics HHSC IT MFADS Users SDS THSteps Vendor Drug Program Status: EDW/BI DD&I Updated Page N-42 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - CLH - Eligibility Lapse Collection Opportunity: CLH - Client Life History Collection: DC113 - Eligibility Lapse Collection Description: Identify individuals with lapses in eligibility and organize data into Episodes of Care. Functional Requirements: FR064 - Identify, measure and evaluate health impact of non-continuous eligibility or enrollment (Medicaid programs) Content: List By Client (client-eligible) By Provider By Program By Service By Time Metrics: Number of Diagnoses after Eligibility Lapse, Number of Treatments after Eligibility Lapse, Average Cost of Treatment post Eligibility Lapse, Number of Eligibility Denials by Reason Topics: Client Eligibility, Episodes of Care Usage: Enable tracking of Client Episodes of Care pre- and post-coverage lapse for frequency and severity of diagnoses (e.g. preventive and maintenance office visits versus hospital admissions and catastrophic events). Allow Cost analysis to be performed to quantify the cost of cover Dimensions: Client, Provider, Program, Service, Time Frequency: On-Request or Triggered or Subscription from Health Information Exchanges Periodicity: Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Provider @[Performing Provider, Provider Type/Specialty, Health Plan] Program @[Risk Group, Waiver Program, Eligibility Denial Code] Service @[Diagnosis, Procedure] Time @[Date of Service] Major Source Systems:* EDW/BI DD&I TIERS (262 Tables, 448GB) Page N-43 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Minor Source Systems:* Additional Data Sources: Eligibility Codes and Descriptions Enrollment Codes and Descriptions Service Authorization Codes and Descriptions Leveraged Collections: Client Composite Eligibility Collection Episode of Care Collection User Groups: DADS Budget Analysts DFPS Analysts HHSC IT MFADS Users SDS System Forecasting Vendor Drug Program Status: EDW/BI DD&I Updated Page N-44 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - CLH - HIE Collection Opportunity: CLH - Client Life History Collection: DC152 - HIE Collection Description: Collect HL7 data from a variety of Health Care Services including hospitals and Private Insurance Groups to enrich Client records. Functional Requirements: FR033 - Obtain surveillance data (HL7) currently collected by hospitals. FR050 - Integrate lab data with client records. FR052 - Track health outcomes by services and cost. FR028 - Identify people without health insurance. FR066 - Integrate Vendor drug by incorporating drugs prescribed through private insurance providers. FR067 - Integrate health data from private insurers. FR075 - Discover duplication across Texas healthcare services; not just Medicaid programs. FR013 - Design more proactive services and programs given wider view of healthcare delivery over time Content: List By Client By Program By Service By Time Metrics: Percent of Program exceeding Utilization, Cost by Program Topics: HIE, Episodes of Care, Service Utilization Usage: Enable more detailed analysis of Client medical profile and history including care received outside of Medicaid. Dimensions: Client, Program, Service, Time Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA. Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Program @[Risk Group, Waiver Program] Service @[Diagnosis, Procedure] EDW/BI DD&I Page N-45 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Product @[Drug] Time @[Date of Service, Fiscal Month, Fiscal Year, Any Aggregate Level] Major Source Systems:* Minor Source Systems:* Additional Data Sources: Alignment of EHR Data Elements Course Treatment Time-Line EMR Parser Service Categories Leveraged Collections: Client Personal Cross-Reference User Groups: DADS Budget Analysts DFPS Analysts DSHS Center for Health Statistics HHSC IT HHSC Operations Support (Managed Care) MFADS Users Office of the Medical Director SDS System Forecasting THSteps Status: EDW/BI DD&I New Page N-46 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - CLH - High Risk Cohort Collection Opportunity: CLH - Client Life History Collection: DC116 - High Risk Cohort Collection Description: Collect all episodes of care for individuals who have had specified high risk diagnoses such as Type I and Type II Diabetes, Asthma, COPD, etc., including charges/costs, procedures/treatments, and prescriptions. Accumulate costs and align and track individuals’ episodes of care for frequency and severity of diagnoses (e.g. preventive and maintenance office visits versus hospital admissions and catastrophic events). Functional Requirements: FR010 - Detect outlier client cohorts and rates that merit new programs/waivers FR046 - Detect clients with diagnoses indicating the need for disease management FR049 - Track health care timeliness, process of service delivery (including disease mgmt). Content: List By Client By Program By Service (High Risk) By Location By Time Metrics: Number of Clients by High Risk Cohort, Number of Diagnoses by Time, Number of Clients with Comorbidities Topics: Risk Group, Episodes of Care, Service Utilization Usage: Accumulate baseline statistics for high risk cohorts receiving Medicaid benefits. Develop high risk profiles. Identify candidates for Disease Management programs. Compare courses of treatment for cohorts with established quality of care standards, and evidence-based protocols. Identify providers who may need education regarding updated standards of care for high risk and chronic conditions. Dimensions: Client, Program, Service, Location, Time Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client EDW/BI DD&I Page N-47 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Program @[Risk Group, Waiver Program] Service @[Diagnosis, Procedure] Location @[Service Location] Time @[Date of Service] Major Source Systems:* Minor Source Systems:* Additional Data Sources: Procedure Code Translators TANF Leveraged Collections: Client Composite Eligibility Collection Cohort Collection Episode of Care Collection User Groups: DFPS Analysts DSHS Center for Health Statistics HHSC IT MFADS Users SDS System Forecasting THSteps TMHP Vendor Drug Program Status: EDW/BI DD&I Updated Page N-48 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - CLH - LTC Care Collection Opportunity: CLH - Client Life History Collection: DC111 - LTC Care Collection Description: Collect all Episodes of Care for individuals in LTC Programs/Waivers across different care models such as state supported institutions, institutional care, home and community based care, and self-directed care. Functional Requirements: FR049 - Track health care timeliness, process of service delivery (including disease mgmt). FR051 - Track client quality of life linked to services and cost and vulnerability. FR053 - Provide the ability to predict and prevent negative outcomes, including data to help assess client quality of life Content: List By Client (Client-Eligible, Client-Waiver) across Program (LTC) By Service By Time Metrics: Average Cost per Episode, Average Length per Episode, Average Cost per Client by Program Topics: LTC, Episodes of Care, Service Utilization Usage: Enable development of measures based on required levels of care and care models to compare costs of similar LTC care. Align and track Clients’ other Episodes of Care for frequency and severity of diagnoses (e.g. preventive and maintenance office visits versus hospital admissions and catastrophic events). Dimensions: Client, Program, Service, Time Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Client Program @[Risk Group, Waiver Program] Service @[Diagnosis, Procedure] Time @[Date of Service] EDW/BI DD&I Page N-49 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Major Source Systems:* CARE (17 Tables, 7GB) Compass 21 (228 Tables, 2624GB) Encounters (64 Tables, 356GB) SAS (23 Tables, 7GB) Minor Source Systems:* Additional Data Sources: ASPEN Leveraged Collections: Episode of Care Collection Program Enrollment by Client Collection User Groups: DFPS Analysts HHSC IT MFADS Users SDS Status: EDW/BI DD&I Updated Page N-50 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - DM - Client Personal CrossReference Opportunity: DM - Data Management Foundation Collection: DC065 - Client Personal Cross-Reference Description: Over time, collect identifying and personal data for clients across all Medicaid programs and systems. Append both financial assessment and functional assessment data. Functional Requirements: FR006 - Monitor [cost] impact of migration between programs and services (including both internal and external as available) FR005 - Compare rates & costs for a client cohort within/across programs FR015 - Use Vital Statistics (or County Records) to notify business units of client life changes. FR023 - Provide visibility to client enrollment for all Medicaid programs FR026 - Classify clients by disenrollment reasons to trigger intervention and/or alternate program placements FR027 - Provide visibility to client authorization for Medicaid FR045 - Identify clients with a specified primary diagnoses over a specific period of time. FR046 - Detect clients with diagnoses indicating the need for disease management or FR047 - Identify clients who have frequent service or provider changes to determine cause. FR052 - Track health outcomes by services and cost. FR053 - Provide the ability to predict and prevent negative outcomes, including data to help assess client quality of life FR057 - Monitor drugs prescribed by client, diagnosis, program, service, and provider. FR059 - Provide integrated visibility of drugs dispensed to Medicaid/Medicare dual eligibles. FR062 - Monitor duration and continuity of care. FR064 - Identify, measure and evaluate health impact of non-continuous eligibility or enrollment (Medicaid programs) FR065 - Measure and evaluate health impact of non-continuous service utilization EDW/BI DD&I Page N-51 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] FR072 - Discover duplication based on enrollment in the integrated eligibility systems. FR073 - Discover duplication of services based on service utilization. FR074 - Discover duplication of services based on drug utilization. FR075 - Discover duplication across Texas healthcare services; not just Medicaid programs. FR076 - Implement enterprise view across agencies of case management portfolio. FR077 - Monitor drug use for clients in concurrent/complex case management programs. FR078 - Compare client outcomes across case management programs. FR080 - Perform geographic and/or demographic analysis of clients. FR081 - Perform geographic and/or demographic analysis of client access to care. FR082 - Compare services used against services available by client & location. FR083 - Perform geographic and/or demographic analysis of client drug utilization. FR084 - Compare treatments for similar diagnoses by geography or demography FR085 - Support longitudinal views of clients by geographic and/or demographic groups FR051 - Track client quality of life linked to services and cost and vulnerability. FR018 - Integrate DSHS registries with client records. FR049 - Track health care timeliness, process of service delivery (including disease mgmt). FR020 - Incorporate public health strategy program data, e.g., immunizations, smoking FR024 - Trend client enrollment / disenrollment across programs and risk groups. FR025 - Investigate client churn by program or risk group. FR007 - Monitor service utilization by program, risk group, or cohort. FR008 - Anticipate future needs for programs by analysis of trends in services EDW/BI DD&I Page N-52 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] FR010 - Detect outlier client cohorts and rates that merit new programs/waivers FR004 - Provide capability to share data with other states for disaster response. FR016 - Identify family units (not just households) FR022 - Track client eligibility across all programs included in TIERS FR002 - Create consistent and readily available per capita program denominators FR034 - Track service delivery to client by provider including parent company. FR028 - Identify people without health insurance. FR014 - Create integrated, unduplicated client profile and improve data quality. FR103 - Provide visibility to clients by providers. FR099 - Provide history in accordance with retention requirements FR060 - Identify indicators of aberrant or irregular client use of drugs. Content: List By Client (client identifiers, financial assessments, functional assessment) Metrics: N/A - Base Collection Topics: Client Identity Resolution, Master Data Management Usage: Provide a single and comprehensive source for all client information. Dimensions: Client Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade. Must be at least as long as Service Granularity: Client Major Source Systems:* ACS PCRA-VDP (Sizing TBD) KIDS (18 Tables, 18GB) NORTH STAR (44 Tables, 8GB) EDW/BI DD&I Page N-53 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Minor Source Systems:* Access HR (2200 Tables, 2GB) CMBHS (1296 Tables, 860GB) CPW Provider (27 Tables, 250GB) CRS (Tables TBD, 500GB) DSHS IMD - MSIS Reporting (6 Tables, 65GB) HCDCS (Tables TBD, 1GB) HCS (INFO) (56 Tables, 5GB) HHSAS (42000 Tables, 4GB) IMPACT (900 Tables, 500GB) NBS/LIMS (694 Tables, 220GB) SAVERR (363 Tables, 1GB) TER (Tables TBD, 1115GB) TKIDS (140 Tables, 35GB) Additional Data Sources: BME File Case management Cross-Reference Census Data CHIP Client Analytic Categories Client Conformance Client External Source Integration DSHS NPAOP DSHS TPC Enrollment Codes and Descriptions Functional Assessment Codes and Descriptions Geocode Data (Stand alone) ICD-9 Diagnostic Codes and Descriptions Insurance Brokerage Data Insurance Provider Data Program Codes and Descriptions RDM Service Authorization Codes and Descriptions State Data Center Population Data WIC Leveraged Collections: EDW/BI DD&I N/A - Base Collection Page N-54 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 User Groups: DADS Budget Analysts DFPS Analysts DSHS Center for Health Statistics ECI Analysts HHSC Actuarial Analysis HHSC IT HHSC Operations Support (Managed Care) MEHIS Analysts MFADS Users Office of the Medical Director SDS System Forecasting THSteps TMHP Vendor Drug Program Vision 21 Users Status: EDW/BI DD&I Updated Page N-55 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - DM - Drug Category Collection Opportunity: DM - Data Management Foundation Collection: DC047 - Drug Category Collection Description: Collect and align Drug data from a variety of sources both internal and external to Texas HHS. Provide a single and comprehensive source for all Drug Category information at HHS. Functional Requirements: FR055 - Map prescription drug stream to episode of care services data. FR060 - Identify indicators of aberrant or irregular client use of drugs. FR070 - Detect, delineate, and track potential waste and inappropriate use (Drugs and Supplies). FR074 - Discover duplication of services based on drug utilization. FR083 - Perform geographic and/or demographic analysis of client drug utilization. FR086 - Provide consistent, integrated reference data (e.g., programs/waivers, risk groups, providers, drugs) to support: MCO oversight, regulatory reporting, and forecasting. FR100 - Provide a drug reference file FR101 - Provide a DME and supply reference file Content: List By Product (Drug Category) Metrics: N/A - Reference Collection Topics: Drug Categorization Usage: Provide Drug Categorization data that enables analysis across Episodes of Care, Provider and Client. Dimensions: Product Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Reference data exists in proprietary systems but needs to be acquired for enterprise use. Historical Retention: EDW/BI DD&I Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Page N-56 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Granularity: Product @[Drug Category, Drug, NDC, Formulation] Major Source Systems:* ACS PCRA-VDP (Sizing TBD) Minor Source Systems:* MEHIS (Sizing TBD) Additional Data Sources: Claims Parser for DME and Supplies Classification Scheme Alignment CMS PDL Drug Analytic Categories Drug Classification Drug Cross-Reference Drugs to Diagnosis [Internal] Drugs to Procedure [External] Drugs to Procedure [Internal] HEDIS Industry Therapeutic Groups National Drug Code Reference Data Standard Measurement Libraries Texas Preferred Drug List Leveraged Collections: N/A - Base Collection User Groups: DADS Budget Analysts DFPS Analysts DSHS Center for Health Statistics ECI Analysts HHSC IT HHSC Operations Support (Managed Care) SDS THSteps Vision 21 Users Status: EDW/BI DD&I New Page N-57 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - DM - Medicare Services Collection Opportunity: DM - Data Management Foundation Collection: DC134 - Medicare Services Collection Description: Collect claims and encounters data from Medicare programs. Integrate Medicare claims and encounters into Client Episodes of Care. Functional Requirements: FR063 - Integrate Medicaid and Medicare data for dual-eligible population. FR088 - Compare Medicare with Medicaid providers FR006 - Monitor [cost] impact of migration between programs and services (including both internal and external as available) FR059 - Provide integrated visibility of drugs dispensed to Medicaid/Medicare dual eligibles. FR075 - Discover duplication across Texas healthcare services; not just Medicaid programs. FR048 - Include non Title XIX funded program services that have a direct impact on Medicaid client health Content: List By Client By Provider By Program, By Service By Time Metrics: Average Cost per Claim, Average Cost per Client over time Topics: Dual Eligibility, Service Utilization Usage: Enable comparison of service utilization and costs by Program for dual eligible Clients. Dimensions: Client, Provider, Program, Service, Time Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Based on future detail design requirements Granularity: Client Provider @[Provider Type/Specialty, Health Plan] Program @[Risk Group, Waiver Program] Service @[Diagnosis, Procedure] EDW/BI DD&I Page N-58 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 Time @[Date of Service] Major Source Systems:* Minor Source Systems:* Additional Data Sources: Medicare Part A Claims Medicare Part B Claims Medicare Part C Claims Medicare Part D Claims Leveraged Collections: Client Personal Cross-Reference User Groups: DADS Budget Analysts DFPS Analysts HHSC IT HHSC Operations Support (Managed Care) MFADS Users SDS System Forecasting THSteps TMHP Vendor Drug Program Status: EDW/BI DD&I New Page N-59 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - DM - Program Collection Opportunity: DM - Data Management Foundation Collection: DC147 - Program Collection Description: Collect and align Program data across the HHS Enterprise. Provide a single and comprehensive source for all Program information at HHS to include services offered, related legislation, benefit plans and more. Functional Requirements: FR035 - Track service delivery across programs by provider including parent company FR001 - Map programs and waivers to create a program profile FR002 - Create consistent and readily available per capita program denominators FR003 - Determine availability in comparable programs (Medicaid) FR009 - Benchmark Medicaid prices/costs/rates for comparisons within an agency and across programs with historical data. FR036 - Compare episodes of care by provider type, specialty, or health plan. FR039 - Support coordination of care between successive care providers or programs FR041 - Expose streams of care episodes that cross programs or departments or agencies FR042 - Track and analyze differences in reimbursement units of service, e.g., time (day, hourly, fifteen minutes, encounter, etc.) FR043 - Assess comparable services within and across all agencies FR044 - Track cost of care across programs and providers FR061 - Provide a single view of Medicaid services across programs/agencies. FR073 - Discover duplication of services based on service utilization. FR030 - Provide visibility to provider enrollment for all Medicaid programs. FR072 - Discover duplication based on enrollment in the integrated eligibility systems. FR076 - Implement enterprise view across agencies of case management portfolio. FR077 - Monitor drug use for clients in concurrent/complex case EDW/BI DD&I Page N-60 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] management programs. FR005 - Compare rates & costs for a client cohort within/across programs FR006 - Monitor [cost] impact of migration between programs and services (including both internal and external as available) FR007 - Monitor service utilization by program, risk group, or cohort. FR008 - Anticipate future needs for programs by analysis of trends in services FR010 - Detect outlier client cohorts and rates that merit new programs/waivers FR011 - Improve ability to predict and manage the impact of changes to programs and service delivery models. FR020 - Incorporate public health strategy program data, e.g., immunizations, smoking FR047 - Identify clients who have frequent service or provider changes to determine cause. FR052 - Track health outcomes by services and cost. FR012 - Determine when to modify existing programs or design a new waiver based on drug data. FR013 - Design more proactive services and programs given wider view of healthcare delivery over time FR057 - Monitor drugs prescribed by client, diagnosis, program, service, and provider. FR017 - Identify caregivers and track status (e.g., age, health, availability to client, location) FR029 - Create an integrated provider profile. FR078 - Compare client outcomes across case management programs. FR048 - Include non Title XIX funded program services that have a direct impact on Medicaid client health FR022 - Track client eligibility across all programs included in TIERS Content: None Metrics: N/A - Base Collection Topics: Program, Master Data Management Usage: Enable creation of per capita program denominators. Allow for comparison of programs and services to identify areas of overlap and alternatives. Monitor cost to programs by service to identify trends and forecast future EDW/BI DD&I Page N-61 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] program needs. Dimensions: Program Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: Observe and comply with HIPAA Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Program @[Risk Group, Waiver Program] Major Source Systems:* ACS PCRA-VDP (Sizing TBD) CARE (17 Tables, 7GB) Compass 21 (228 Tables, 2624GB) Encounters (64 Tables, 356GB) SAS (23 Tables, 7GB) TIERS (262 Tables, 448GB) Minor Source Systems:* Additional Data Sources: Drug Merge Medicaid Program Registry Program Codes and Descriptions SSA Addresses Leveraged Collections: N/A - Base Collection User Groups: DADS Budget Analysts DFPS Analysts DSHS Center for Health Statistics HHSC Actuarial Analysis HHSC IT HHSC Operations Support (Managed Care) MEHIS Analysts MFADS Users Office of the Medical Director EDW/BI DD&I Page N-62 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 People who need clean addresses for mailings SDS System Forecasting THSteps TMHP Vendor Drug Program Status: EDW/BI DD&I New Page N-63 Confidential – Sensitive Procurement Information [Date] Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] Data Collection Specification - DM - Provider Collection Opportunity: DM - Data Management Foundation Collection: DC148 - Provider Collection Description: Collect data from internal and external sources on Providers and align across the HHS Enterprise. Provide a single and comprehensive source for all Provider information at HHS to include Provider address, Physicians, Certifications/Accreditations, Locations, Citation History and more. Functional Requirements: FR036 - Compare episodes of care by provider type, specialty, or health plan. FR038 - Consolidate provider metrics. FR044 - Track cost of care across programs and providers FR047 - Identify clients who have frequent service or provider changes to determine cause. FR079 - Identify specific services by location. FR088 - Compare Medicare with Medicaid providers FR039 - Support coordination of care between successive care providers or programs FR032 - Integrate registry data from provider accreditation organizations. FR017 - Identify caregivers and track status (e.g., age, health, availability to client, location) FR030 - Provide visibility to provider enrollment for all Medicaid programs. FR031 - Provide integrated, cleansed provider data to support regulatory changes FR034 - Track service delivery to client by provider including parent company. FR035 - Track service delivery across programs by provider including parent company FR037 - Assess quality of service by provider. FR081 - Perform geographic and/or demographic analysis of client access to care. FR082 - Compare services used against services available by client & location. EDW/BI DD&I Page N-64 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 [Date] FR080 - Perform geographic and/or demographic analysis of clients. FR084 - Compare treatments for similar diagnoses by geography or demography FR057 - Monitor drugs prescribed by client, diagnosis, program, service, and provider. FR058 - Analyze drug delivery by provider. FR012 - Determine when to modify existing programs or design a new waiver based on drug data. FR083 - Perform geographic and/or demographic analysis of client drug utilization. FR029 - Create an integrated provider profile. FR103 - Provide visibility to clients by providers. FR105 - Map provider and provider parent company relationships Content: List By Provider By Program By Location Metrics: N/A - Base Collection Topics: Provider, Episodes of Care, Master Data Management Usage: Enables Provider analysis by Program, Service, Diagnosis, Location and other attributes. Dimensions: Provider, Program, Services, Location Frequency: Continuous where possible, otherwise daily Periodicity: Weekly, Monthly, Fiscal Year, Calendar Year Security: None Historical Retention: Net-change retention for a minimum of one decade (must be at least as long as Service Delivery) Granularity: Provider @[Performing Provider, Provider Type/Specialty, Health Plan] Program @[Risk Group, Waiver Program] Location @[Service Locations] Major Source Systems:* CARES (106 Tables, 351GB) Compass 21 (228 Tables, 2624GB) MAXSTAR - MAXIMUS (Sizing TBD) NE Provider (61 Tables, 1GB) PPS (42 Tables, 1075GB) EDW/BI DD&I Page N-65 Confidential – Sensitive Procurement Information Texas Health and Human Services Commission RFP No. 529-13-0018 TIERS (262 Tables, 448GB) Minor Source Systems:* ANE (68 Tables, 4GB) Additional Data Sources: BDE File BNE Census Data Drug Formulary Geocode Data (Stand alone) ICF-MR OASIS PARIS Provider Facilities Provider Identity Reconciliation and Merge Provider Ownership and Contract Info Provider Structure with Employees Provider Taxonomy SureScripts Leveraged Collections: N/A - Base Collection User Groups: DADS Budget Analysts DFPS Analysts DSHS Center for Health Statistics HHSC IT HHSC Operations Support (Managed Care) MEHIS Analysts MFADS Users Office of the Medical Director People who need clean addresses for mailings SDS System Forecasting THSteps TMHP Vendor Drug Program Status: EDW/BI DD&I New Page N-66 Confidential – Sensitive Procurement Information [Date]