Exhibit E: Source Systems Listing
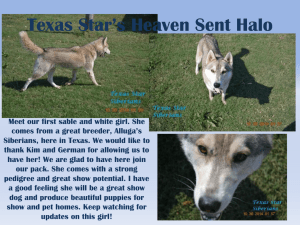
advertisement

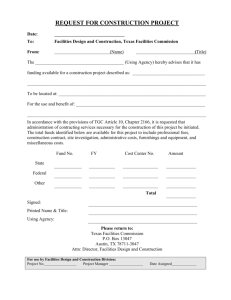
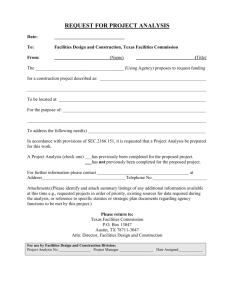
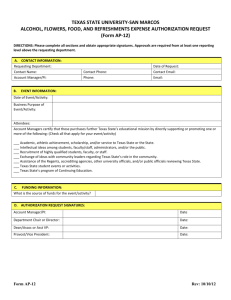
Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 Exhibit E Exhibit E: Source Systems Listing The following table lists the Primary Source Systems that are currently identified for this RFP: System Name System Description Database Size Database Platform (GB) Texas Integrated Eligibility Integrated eligibility system for Texas Works, Food Stamps, Medicaid, Redesign System (TIERS) and Long-Term Care. Task List Management (TLM) Work Flow Management data Oracle 16384 Oracle 1 Compass21 Claims Processing System is operated by (Texas Medicaid Compass21 (C21) & Healthcare Partnership) TMHP. It provides an integrated solution that 5,600 Tandem Non-Stop supports fee-for-service claims, encounter data processing and analysis, and captures data relative to multiple health care models Vision21 is a “Fee for Service Claim” and “Managed Care Encounter” focused Medicaid data warehouse with a broad set of applications that Vision21 (V21) help HHSC and Texas Medicaid & Healthcare Partnership users make better business decisions through on-line analytical processing (OLAP), Tandem Non-Stop 9000 query and reporting functions, extracts, statistical analysis, and forecasting. This system stores historical claims data. Provider Management Provider Management Database holds provider data enrolled via PEP Database (PMDB) application 100 MS SQL 2005 3,200 Oracle The Electronic Data Interchange (EDI) system for the Encounters project enables trading partners to conduct business with TMHP electronically, ENCOUNTERS Operational Data Store (ODS) via batch and/or real-time mode. The Texas Encounters Data Enhancement project offers greater ability to analyze the practices of Managed Care Organizations (MCOs) and Behavioral Health Organizations (BHOs), which provide health care services to Medicaid and Children's Health Insurance Program (CHIP) members in the State Page E-1 Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 System Name Exhibit E System Description Database Size Database Platform (GB) of Texas. The Claims Management System (CMS) processes long-term care claims for the Texas Department of Aging and Disability Services (DADS). DADS consist of former departments such as the Department of Long Term Care (LTC) Claims Management System (CMS) Human Services (TDHS) and the Department of Mental Health and Mental Retardation (MHMR). CMS handles claims filed via through TexMedConnect software, and by third-party business partners (no Tandem Non-Stop 533 longer process any paper claims). It also processes claims filed retroactively by the system. TexMedConnect and EDI can also be used to access claim status or client eligibility lookups based on information from CMS. Primary system for Vendor Drug Program (VDP). Performs drug Pharmacy/Pharmacy Rebate utilization review at the point of sale and on-line adjudication of Pharmacy/Pharmacy Rebate system is pharmacy claims. The RxPert application is a prior authorization under procurement and the EDW processing system that makes a determination for a prior authorization Contractor will work with the new request submitted via the PCRA system, PAXpress website, or the PA Pharmacy/Pharmacy Rebate Vendor to Call Center. The following types of data are contained in the system: (1) Client Information, (2) Pharmacy Information, (3) Provider Information, obtain system information and acquire data to meet the functional needs of this (4) Medical Claims Data, (5) Pharmacy Claims Data, (6) PA Details, and RFP. (7) Determination Information. Premiums Payable System (PPS) Health Services Delivery. Manage Premiums Payable records and 3,697 Oracle 375 Oracle calculate premium amounts. Managed care capitation rates are provided. Texas Medical Transportation System (Previously known as Tejas Texas Medical Transportation System (TMTS) (MTP). This system will integrate with Telecom to support scheduling and authorization for non-emergency medical transportation, including interfacing with the claims administrator and providing enhanced reporting. Contains (Health Insurance Portability and Accountability Act) Page E-2 Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 System Name Exhibit E System Description Database Size Database Platform (GB) HIPAA and (Personal Health Information) PHI. When women who are enrolled in Medicaid or CHIP managed care delivers, the HMO is eligible for a supplemental payment (in addition to their regular premium payment). Each HMO send in DSP “claims” in a specific format in excel workbooks. Visual basic applications reads the claims, check the claims against copy of the managed care eligibility data, check for a series of ‘edits’, and if the claim passes all edits it is accepted, otherwise it is rejected. Delivery Supplemental Accepted and rejected data is submitted for each HMO in excel Payments (DSP) workbooks, and produce a count and a voucher file which is used by 200 MB SQL Server and Data also stored in Excel File HHSC accounting to generate payments. Accepted and rejected data is maintained in SQL Server. More info about DPS can be found in: Texas Medicaid and CHIP Uniform Managed Care Manual http://www.hhsc.state.tx.us/medicaid/managed-care/umcm/ section 5.3.5 LTSS Provider Long Term Services and Supports Provider data 1 MS Access The Long Term Care (LTC) Provider system contains information about NE Provider - Long Term Care (LTC) Provider DADS Providers, Contracts, Rates, and Budgets. The information from this database is mainly used for paying the providers for services rendered and this is done by the Claims Processing System administered by TMHP. Page E-3 3 Oracle