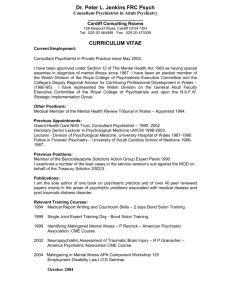
Systems Based Practice - Royal College of Psychiatrists
advertisement
DRAFT The Role of the Psychiatrist in health services Professor Dinesh Bhugra February 2009 1 Introduction Psychiatry is the branch of medicine that deals with the medical treatment of mental illness, emotional disturbance and abnormal behaviour. The term ‘psychiatry’ was first coined about 200 years ago, replacing the now archaic term ‘alienism’. A psychiatrist is a medically-qualified doctor who deals with mental illness, as well as the interaction between physical and mental illness. It is well established that a significant proportion of physically ill patients will also suffer from mental illness. An equally large number of patients with mental illness will have physical problems, either contributing to their illness or as a sequel of their mental illness. A major advantage of psychiatry training is learning about psychological and social causation in addition to medical knowledge in aetiology and the management of mental illness. Psychiatrists are thus best placed to use integrated bio-psychosocial models in understanding the aetiology of mental illness and managing mental illness, emotional disturbance and abnormal behaviour. This is what makes us different from other disciplines. Following the MMC and MTAS fiascos in 2007, Professor Sir John Tooke in his admirable report, Aspiring to Excellence, suggested that doctors need to redefine their role. Independent of this suggestion, the Royal College of Psychiatrists had already embarked on looking at issues related to professionalism and the role of the psychiatrist in the 21st century. His paper sets out a proposed road map for the role of the psychiatrist, and the competencies and skills required to deliver services. Other documents on professionalism in psychiatry and psychiatry’s contract with society will follow later in 2009. Background Psychiatry, like other branches of medicine, is a patient focused speciality. Patient-centred Psychiatry depends upon delivering care which is patient focused. Patient-centred care is defined as “(Care) which explores the Patients’ reasons for their visit, their concerns and need for information, seeks an integrated understanding of the patient’s world i.e. their whole person, emotional needs and life issues and finds common ground on what the problem is and mutually agrees on management, enhances prevention and health promotion and enhances the continuing relationship between the patient and the doctor” (Stewart 2001:445). The core of the therapeutic intervention is doctor-patient interaction which has six components as illustrated in Table 1. Table 1. Six interactive components of the patient-centred process. (After Brown et al 2003) 1. Exploring both the disease and the illness process History, physical examination, investigations. Dimensions of illness [explanatory models, feelings, ideas, effects on function and expectations] 2 2. 3. 4. 5. 6. Understanding the whole person The person (life history, development and personal issues) The proximal context (family, employment, social support) The distal context (culture, community, society) Finding common ground Problems and priorities Goals of treatment and management Roles of patient and doctor Incorporating health promotion and prevention Health advancement Avoiding and reducing risk Early identification Reducing complications Enhancing doctor-patient relationship Compassion Power Healing Self Awareness Transference and counter transference Being realistic Time and timing Team building and teamwork Managing resources The CanMEDS 2005 physician competency framework (Frank 2005) sets the scene for the training of physicians, competence of physicians, and quality care. It provides a competency-based framework for educators and resources for Continuing Professional Development (CPD), as well as information for other stakeholders. These competencies can be equally valid for psychiatry. They can also be common to other disciplines dealing with mental ill health and related complications. However, as in Psychiatry, the medical expert lies at the core of the CanMEDS construct (see figure 1). 3 Figure 1. There are seven components within this framework and these will be discussed below. However, each competency in the CanMEDS framework is made up of elements of their own and can further be broken down into smaller components for teaching, training and, learning. The seven competencies of the psychiatrist will define the professional, although each role will vary in different individuals according to their individual interests and responsibility. For example, those who are heavily involved in teaching, whether it is undergraduate or postgraduate, may have developed their role as a communicator or scholar better than their role as a manager or an advocate. However, this is not to say that most individuals cannot attain or follow these roles. From a UK perspective, Good Psychiatric Practice, published by the Royal College of Psychiatrists (2009 edition in press), highlights the key characteristics expected of a good psychiatrist. Good Psychiatric Practice lists attributes of a good psychiatrist in following areas: Trusting Relationship Good Clinical Care Consent to treatment Note keeping and inter-agency/inter-professional communication Confidentiality Availability and emergency care Working as a member of the team Referring patients Clinical governance Teaching and training 4 Researcher Being good employee and employer The core attributes listed in Good Psychiatric Practice (p5) are: Clinical competence Being a good communicator and listener Being sensitive to gender, ethnicity and culture Commitment to equality and working with diversity Having a basic understanding of group dynamics Being able to facilitate a positive atmosphere within a team Ability to be decisive Ability to appraise staff Basic understanding of operational management Understanding and acknowledging the role and status of vulnerable patients Bringing empathy, encouragement and hope to patients and carers Critical self awareness of emotional responses to clinical situations Being aware of potentially destructive influence in power relationship Acknowledging situations where there is potential for bullying A comparison between Table 1 and the attributes of a good psychiatrist as laid down in Good Psychiatric Practice indicates a tremendous area of overlap in the qualities of an individual as well as the characteristics of a service that will be acceptable to patients and their carers. The CanMEDS Components Medical Expert: Whatever the sub-speciality within psychiatry, the role of the psychiatrist as a medical expert and a healer is at the core of it. This role distinguishes psychiatrists, especially in the treatment of mental illness, more than anything else. Whether one or all components of bio-psychosocial model are considered or employed in identifying causation and planning management of mental illness, the psychiatrist is primarily a medical expert and a healer. Psychiatrists possess a defined body of knowledge and clinical skills (including diagnostic, investigatory and management skills) which focus on patient centred care. The psychiatrist as a medical expert, is trained and able to collect, explore and synthesise information on the patient’s illness from history taking, direct observation and investigations through third party information and physical or laboratory investigations, which contribute to accurate diagnosis. The medical expert then uses evidence to plan and carry out treatment within the boundaries of their discipline and with clear responsibilities discussed and allocated within the team. The care is characterised by healing and using up to date, ethical, resourceefficient treatments through communications with key stakeholders. The core of the doctor–patient interaction lies in the patient centred processes. In order to be a medical expert, the psychiatrist needs to be able to integrate different models of aetiology and management embedded in medical knowledge, which will lead to appropriate diagnostic reasoning and clinical judgement associated with clinical decision making. These will lead to identification of appropriate therapies and human care within the prevalent ethical framework. The expert must remain up to date in both skills and knowledge and be aware of one’s limits of competence. 5 This awareness will contribute to appropriate help seeking and suitable referral whenever indicated. Six enabling competencies highlighted in CanMEDS framework are illustrated in Table 2 1. Functions effectively as a consultant; integrating roles provide optimal, ethical and patient centred care 2. Establish and maintain clinical knowledge, skills and attitudes appropriate to their practice 3. Perform a complete and appropriate assessment of the patient 4. Use preventative and therapeutic interventions effectively 5. Demonstrate proficient and appropriate use of procedural skills; both diagnostic and therapeutic skills 6. Seek appropriate consultations from other health professionals – recognising the limits of their expertise Table 2: Enabling competencies for the medical expert (CanMEDS Framework). Communicator: As a communicator, the psychiatrist facilitates the doctor–patient relationship. Communications with the patient, their carers and community and society at large, are a significant part of the role of a psychiatrist. Essential components of this role are establishing rapport and trust, formulating and explaining diagnosis, sharing information and facilitating a mutually agreed and shared plan of management. There may be disagreements or acknowledged differences in understanding of aetiological factors within the team and these need to be taken on board. The psychiatrist, as a communicator, must demonstrate empathy, compassion, trustworthiness and integrity with respect for diversity of opinion and cultural values, with clear attention to psychosocial aspects of illness. Keeping clear, appropriate and accurate notes and maintaining confidentiality are part of this role. Conveying appropriate information to patients, their carers and community and society at large in an easily understood manner at the right level are important. It can be argued that the role of psychiatrist as a communicator is at a different level when compared with other professionals in the team. This role is communicating a treatment and information strategy that informs patients, carers and society at large. Collaborator: As collaborator, the psychiatrist works effectively within a team to deliver acceptable and appropriate optimal patient care. Working within a team is at the heart of modern health care delivery. Shared decision making, conflict resolution, awareness of team dynamics, negotiation, and awareness of each team member’s roles and responsibilities are some of the components of the role. Other components include working with community agencies, such as voluntary organisations and primary care, and working across religious, cultural, sexual orientation, age, or gender divides. 6 Manager: Health care resources are finite whereas the demand is ever increasing. The psychiatrist has to manage resources, time and teams. As managers, psychiatrists are essential in organising sustainable clinical practice, making decisions about allocating resources, and contributing to a resource-efficient and effective health care system. The role of the clinician as a clinical leader is important in identifying needs in allocated finite resources where demands continue to rise. The functional split of teams requires an open discussion regarding validity and resources required for such a development. Psychiatrists therefore need to negotiate with society as to what is required in the delivery of mental health care and discuss prioritisation of resources. They need to be aware of resources and allocation, and look at the effectiveness and efficiency of services being provided. They should be aware of research base and evidence and employ this information appropriately As mangers they should be able to manage their careers effectively, and have the skills to work and develop as managers and administrators. Advocate: As health advocates, psychiatrists should be able to advocate for their patients and carers, and work with them and their organisations to advocate jointly for resources for patients. They should also advocate for health promotion and prevention of disease as well as for their own role in society. They should be able to advise on mental health care policy and patient safety. As part of public mental health process, they ought to identify determinants of health for the populations that they serve. They have a responsibility to promote the health of individual patients, communities and populations. Scholar: As a scholar, the psychiatrist has a life long commitment to reflective learning, along with development of medical knowledge. Dissemination and application of new knowledge are important components. Elements included in this role are life-long professional development and learning with reflective practice, critical appraisal of evidence, using a variety of learning methods, mentoring, role modelling and research ethics and research questions along with facilitating learning by patients, their carers, psychiatric trainees and other disciplines. Professional: As professionals, psychiatrists are committed to the mental well being of their patients and treating mental illness using ethical practice, following professional standards, high personal standards and setting high standards with self-regulation. Elements of professionalism will be expanded in a later document but include among others: altruism; integrity and honesty; compassion and caring; morality and codes of ethics; responsibility to self, profession and society; commitment to excellence; accountability and self-awareness. A good psychiatrist will be able to demonstrate commitment to their patients, profession and society through ethical practice, self-regulation and sustainable practice. A psychiatrist is a clinician – dealing with mental illness in all its variations – who delivers expert clinical care for mentally ill individuals, usually within a team. They are able to diagnose and manage the complex end of the illness spectrum (diagnosing and managing complicated and complex cases and working with the society and communities they serve to prioritise cases and function effectively within available resources). They are also experts in managing simple cases which may become complex in the hands of inexperienced clinicians. They also have a role in running services, managing resources, teaching, training, researching, developing and delivering acceptable and accessible services with clear involvement in leadership roles and abilities. 7 According to the BMA, the consultant (psychiatrist’s) role is to: Demonstrate the competence and experience to cover complex cases e.g. more than one condition (or simple conditions that may have become complex as a result of handling by inexperienced clinicians) Train, supervise (and mentor) trainees and junior doctors Accept ultimate responsibility for the care of all patients referred to their service (under their leadership even if treatment is being carried out by others) Provide definitive (clinical) opinion and treatment that cannot be provided or managed in primary care The central role of a consultant is as a medical expert to provide high quality patient care. Delivery of care is interconnected with other roles such as ability to communicate, manage, innovate, educate and train. The primary objective of a psychiatrist is to use expert knowledge of psychiatry and personal skills to diagnose and treat patients with mental illness, retaining ultimate clinical responsibility for their care. An awareness of the evidence base or lack thereof and consequent acknowledgement of this is crucial in functioning well in clinical settings. The spirit of scientific enquiry is vital in clinical functioning. Healing may not be evidence based, but treatment can be. Medical and psychiatric decision cannot be automated. The patient must be viewed and treated in their world – with proximal factors such as employment, family and distal factors such as community, society, and cultures. Delivery of optimal health care which will be accepted by the patients and their carers depends on accurate diagnosis, treatment plans and adequate resources along with effective communication. Psychiatrists must be good role models and try to inspire and motivate colleagues and team members. Key skills: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. Specialist psychiatric assessment Treatment planning Managing complex cases Risk assessment and managing risk Developing and sustaining ethical practice Pharmacological treatment Psychotherapeutic treatments Physical treatments Social treatments Physical medical skills Team working Appraisal and educational skills Teaching skills Critical appraisal skills Audit and research skills Collaborating with others Being a resource for others Clinical leadership, management and strategic planning Advocacy 8 Appendix 1 Core Competencies Demonstrate diagnostic and therapeutic skills to efficiently and ethically manage a spectrum of patient care problems within the boundaries of the specialty Elicit a relevant concise and accurate history Conduct an effective physical examination Carry out relevant procedures to collect, analyse and interpret data. Reach a diagnosis Perform appropriate therapeutic procedures to help resolve the patient’s problem Access and apply relevant information and therapeutic options to clinical practice Pose an appropriate patient related question Execute a systematic search for evidence Critically evaluate medical literature and other evidence Demonstrate medical expertise to situations other than indirect patient care. This includes the ability to do the following: Be an expert witness Give presentations/public education Recognise personal limits of expertise Decide when and whom to refer to Implement own professional development Demonstrate effective consultation skills Present well-documented patient assessments and recommendations in both verbal and written forms Essential Roles and Key Competencies Medical Expert: Demonstrate diagnostic and therapeutic skills for ethical and effective patient care: precise clinical history, physical examination, investigation Assess and apply relevant information and therapeutic options to clinical practice Demonstrate medical expertise in situations other than direct patient care 9 Recognise personal limits of experience Demonstrate effective consultation skills with respect to patient care, education and legal opinions: present well-documented patient assessment Communicator: Establish therapeutic relationships with patients and their families: Elicit and synthesise relevant information from patients, their families and communities: beliefs, age, gender, culture Listen effectively, foster understanding Discuss appropriate information with patients, their families and communities and other healthcare professionals Team Player: Consult and liaise with other health professionals Recognise limits of personal competence Contribute effectively to multidisciplinary team, activities (training etc) Aware of roles and expertise of other disciplines Integrate opinions of patients in decision-making Manager: Managing resources and time effectively to balance patient care, learning needs, outside activities and personal life Allocate finite healthcare and education resources effectively and work efficiently Utilise I.T. effectively for patient care, CPD Health Advocate: Help promote health and prevent disability Identify social/cultural factors of health Recognise and respond to settings related to advocacy: populations at risk, policy awareness, development of policy Scholar/Educator: Personal CPD strategy and learning needs and methods 10 Be a critical appraiser of sources of medical information Educator: help others to define learning needs and development, provide feedback, adult learning Professional: Deliver highest quality care with integrity, honesty and compassion: racial, cultural and societal issues Appropriate personal and interpersonal behaviours: self-awareness Ethically acceptable/responsible: local laws Attributes: Medical Knowledge Up to date knowledge needed to evaluate and manage patients Clinical Skills Demonstrate proficiency in history taking Effective physical examination (Investigations: organise and evaluate) Lead and manage diagnostic studies Demonstrate practice skills Show proficiency in technical skills Clinical Judgement Demonstrate clinical reasoning Make sound diagnostic and therapeutic decisions Understand the limits of knowledge Incorporate cost awareness and risk benefit analysis Interpersonal Skills Communicate and work effectively with patients, families, other members of the team and agencies Professional Attitudes and Behaviour Accountability 11 Accept responsibility Maintain comprehensive, timely and legible medical records Available for consultation Seek improvement in quality of care provided Facilitating learning of patients, communities, students and other disciplines Lifelong learning Evaluate critically relevant new medical and scientific information relevant Self-awareness Humanistic qualities Demonstrate integrity and honesty Demonstrate compassion and empathy Respect for privacy and dignity Ethical Managerial Skills Effective and efficient working Utilise IT Health Advocacy Health promotion and prevention Advocate for patients (families and communities) 12 Patient Care Core Competencies General Psychiatry 1 History and examination Complaint History PMH Systematic review FH/sociocultural history Developmental history 1 Differential diagnosis/ evaluation plan Treatment plan 2 Differential diagnosis 2 Assess and document psych. potential Risk assessment Involve treatment standards Intervene effectively to minimise risk Implement prevention methods 3 Evaluate assess and recommend effective management 3 To conduct therapeutic interviews 4 To conduct a range of individual, group and family therapies 5 To recognise and treat psychiatric disorders 13 Medical Knowledge Core Competencies General Psychiatry 1 Epidemiology, aetiology, phenomenology, diagnostic criteria, effective treatment strategies, course and prognosis 1 Knowledge of human growth and development included. Behaviour, cognitions, psychosexual including culture 2 Differential diagnosis healthcare delivery systems and family work 2 Behavioural sciences - learning theory, formal family organisations, family dynamics and communication, group dynamics, anthropology, sociology and theology, cultural psychiatry, community mental health, epidemiology, research methods, psychodynamic theory 3 Ethics 3 Patient evaluation and treatment selection include psychological testing, lab tests, MSE, diagnostic interview, treatment comparison, psychosocial. Therapies All forms of psychotherapy Brief therapy CBT Psychodynamic psychotherapy All delivery systems of Psychotherapy Individual/Family Treatment of psychosexual dysfunction Doctor-patient relationship Biometric treatments Pharmacotherapy Pharmacological actions Clinical indications Side-effects Drug interactions Toxicities Appropriate prescribing Cost effectiveness Ethnopsychopharmacology Li ECT, Light 14 Medical Knowledge Core Competencies Cont. General Psychiatry Emergency psychiatry Suicide Crisis intervention Home treatment Differential diagnoses in emergency PICU Homicide, rape and violent behaviour Early onset management Substance abuse Pharmaceutical actions of substance abuse Signs/symptoms and onset of toxicity/withdrawal Epidemiology CAP Assessment and training Disorders in infancy Learning Disability Psychiatry of old age Forensic Liaison Specific syndromes Psychological and neurological aspects of physical illness Psychological and neurological complications of physical illness Psychosomatic/Somatopsychic Coping strategies Ethical issues 15 1. Interpersonal and Communication Skills Competencies Level 1 Listen to and understand patient’s verbal and non-verbal communication Communicate effectively with patients verbal, non-verbal and written. Develop and maintain therapeutic alliance through trust, empathy, honesty, openness and comfort. Level 2 Partnerships with patients and carers. Transmit information clearly and meaningfully. Understand ‘counter transference’. Level 3 Communicate members. collaboratively and Educate patients, carers, community work with multidisciplinary team 2. To elicit important diagnostic data affecting treatment from individuals from different ethnic, racial, gender and educational backgrounds -including assessing and managing highly charged affect in patients. 3. Ability to know when to seek consultation, how to discuss it with patients and families and evaluating the consultation. 4. Offer consultancy to other disciplines and communities, thus communicating effectively, clearly and meaningfully, and respect the knowledge and expertise of the requesting professional. Communication with patients and their families at appropriate educational level, cultural sensitivity, explanatory models, preventative strategies, developing rapport. 5. Maintaining medical records and prescriptions in a legible and clearly understandable format with confidentiality, privacy and dignity. 6. Listen effectively to members of the team, elicit needed information, integrate information, manage conflict and communicate treatment plan. 7. Communicate effectively the results of the assessment, use of informed consent, genetic counseling, risk/benefit of treatment, alternative plans, and appropriate education. Practice Based Learning 1. Recognise and accept limitations in their own knowledge base and clinical skills. 2. Appropriate skills for obtaining training and evaluating up to date information using IT, participation in educational activities. 16 3. Appropriate education of caseload, supervision, consultation, case based learning, practice guidelines, reviewed patient records, examining errors in practice, patient education. 4. Critical evaluation of relevant medical literature. 5. Effective remediation if required. Professionalism Core Competencies Demonstrate responsibility in communicating to and from patients, families and other health professionals. Responsibility to be demonstrated by adequate record keeping, coordinating care, providing cover appropriately, providing continuing care. Demonstrate ethical behaviour, integrity, honesty, compassion and confidentiality, informed consent, professional conduct and conflict of interest. Respect for patients and their families irrespective of gender, sexual orientation, religious or political beliefs. Review conduct and re-medicate, review other’s conduct if required and acknowledge and mediate the medical errors. Systems Based Practice Be aware of and follow protocols and guidelines Lead and delegate authority Accurate medical data etc. Limitation of health care resources. Awareness of available resources. Awareness of legal aspects. 17 Role Learning “Bedside” Teaching Structured Teaching Workshops Apprenticeship Model Medical Expert Self Directed Individual Mentoring Problem based learning Clinical reasoning Effective Consultation Presentation Skills E.B. Medicine I.T. Bioethics Empathy Respect Individual and group Reflection of experiences Role models in effective communication Conceptual frame skills in communication Racial/Cultural Role playing Video + Interdisciplinary organisation Seamless healthcare delivery Role modelling Governance structures Teambuilding Managing time, teams and structures Leadership skills Role modelling Shadowing Allocation of resources Practice Management Individual patient and patient population issues Modelling Multidisciplinary teaching Effective intervention and assistance Self directed learning Evidence base Lifelong learning Practice reflection Modelling Clinical standard setting Quality assurance Quality management Health economics Critical appraising Direct observation feedback Modelling Case based discussion Medicolegal W.R. Medical ethics W.R. Awareness of professional responsibilities Communicator Collaborator Manager Health Advocate Scholar Professional 18 Appendix 3 MANAGEMENT AND LEADERSHIP TRAINING 1. 2. 3. 4. 5. 6. 7. 8. 9. Self-awareness and self-management Managing teams Managing conflict Supervision, feedback and appraisal Time management and priority setting Problem solving Strategy and vision Chairing meetings Working with other groups and agencies Appendix 4 From UEMS document: Profile of a Psychiatrist The core function of a psychiatrist is to integrate biological, psychotherapeutic and social factors in aetiology and intervention, Biological treatment Definition To apply biological methods in the treatment of persons with mental disorders. Biological understanding of mental disorders is essential for assessment and treatment of patients with mental disorders. Biological treatment is based on a systematic theory and on good clinical practice. It is evidence based on specific methods comprising a theory of mental and behavioural health and pathology. Biological treatment competencies The psychiatrist is able to… 1. Establish and maintain the treatment alliance 2. Establish a diagnosis of the mental disorder based on assessment 3. Assess which biological method is most appropriate 4. Apply and/or refer to specific biological interventions whenever appropriate 5. Evaluate outcome of biological treatment Psychotherapy Definition To apply psychotherapeutic methods in the treatment of persons with mental disorders. Psychotherapeutic understanding of mental disorders is essential for assessment and treatment of patients with mental disorders. Psychotherapy is based on a systematic theory and on good clinical practice. 19 It is evidence based on specific methods comprising a theory of mental and behavioural health and pathology. Psychotherapy competencies The psychiatrist is able to… 1. Establish and maintain the therapeutic alliance 2. Establish a diagnosis of the mental disorder and of personality based on psychotherapeutic assessment 3. Assess which psychotherapeutic method is most appropriate 4. Apply and/ or refer to specific psychotherapeutic interventions whenever appropriate 5. Evaluate outcome of psychotherapy Social psychiatric intervention Definition To apply social interventions in the treatment of persons with mental disorders. Understanding of mental disorders in their social context is essential for assessment and treatment of patients with mental disorders. Social psychiatric interventions are based on a systematic theory, and on good clinical practice. It is evidence based on specific methods comprising a theory of mental and behavioural health and pathology. Social psychiatric intervention competencies The psychiatrist is able to… 1. Establish and maintain the therapeutic alliance 2. Establish a diagnosis of the social dysfunction based on assessment 3. Assess which social psychiatric intervention method is most appropriate 4. Apply and/ or refer to specific social psychiatric intervention whenever appropriate 5. Evaluate outcome of social psychiatric interventions Integrated treatment The psychiatrist is able to… Plan and apply treatment, integrating assessment and knowledge of biological, psychotherapeutic and social psychiatric areas in such a way that it is experienced by the patient as coherent. References and selected further reading:Academy of Medical Royal Colleges (2004) Implementing the European Working Time Directive: Guidance from the Academy of Medical Royal Colleges. 20 Bhugra, D. Bell S, Burns, A (eds) (2008). Management Training for Psychiatrists London:. Royal College of Psychiatrists Press. Crawford M (2001) Involving users in the development of psychiatric services – no longer an option. Psychiatric Bulletin; 25, pp114-116. Donaldson L (2004) Towards excellence in assessment in medicine: a commitment to a set of guiding principles. Department of Health. Elwyn, G., Greenhalgh, T. and MacFarlane, F (2001). Groups: a Guide to Small Group Work in Healthcare, Management, Education and Research. Radcliffe Medical Press Ltd., Oxford. General Medical Council (1993) Tomorrow’s Doctors: recommendations on undergraduate medical education. Ikkos G (2003) Engaging patients as teachers of clinical interview skills. Psychiatric Bulletin; 26, pp53-55. Piachaud J (2002) Teaching learning disability to undergraduate medical students. Advances in Psychiatric Treatment; 11, pp334-341. Reynolds, A. and Thornicroft, G. (1999). Managing Mental Health Services, Open University Press, Buckingham. Royal College of Psychiatrists (2004) Being seen and heard. A training package. Southgate L and Grant J (2003) Principles and standards for an assessment system for postgraduate medical training. PMETB subgroup on assessment. van der Vleuten C; Newble D; Case S; Holsgrove G; McRae C; McCann B; and Saunders N (1994) Methods of Assessment in Certification: in Newble D; Jolly B; and Wakeford R. (Eds.). The Certification and Recertification of Doctors: Issues in the Assessment of Clinical Competence; 105-125; Cambridge University Press. Young, A. (1999). The Medical Manager. BMJ Books, London 21