Experience of a Trainee in Psychiatry in the UK with Iraqi roots
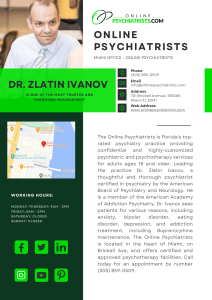
advertisement
TPSIG NEWSLETTER ROYAL COLLEGE OF PSYCHIATRISTS 1ST JAN 2015 Experience of a Psychiatry Trainee in the UK with Iraqi Roots When asked to write of my experiences as a UK psychiatry trainee with Iraqi roots, I was a little daunted. Being British born, bred and educated I can't say that I consciously felt any different from my peers. But after much considered thought I realised that there were a few things which set my experiences apart from others. I was raised in a Middle Eastern household. Both my parents travelled from Iraq to the United Kingdom in the early eighties where my siblings and I were born. My early childhood felt normal. But being primary schooled in a small village in North Yorkshire was when I first became aware of the dissimilarities. Spending time with my English friends, I was aware that my upbringing had been different. My parents did well to adapt to the British way of life, but naturally they held onto many of the values and principles of their own culture and instilled these in me during my upbringing. I distinctly remember a time when I resented this. As a child and teenager you just want to be the same as everyone else. Back then it was fair to say I denied my roots. Now I embrace them. I trained in Sheffield where the majority of psychiatric presentations I was exposed to were of white British men and women, reflecting the relatively less diverse ethnic make-up of South Yorkshire. Moving to London for my core psychiatric training was in many ways the opposite end of the spectrum. Being one of the most cosmopolitan cities in the world, you are caring for patients from a host of different nations. Growing up in an Iraqi household whilst living in the UK gave me the advantage of not only learning two languages, but also of learning two different cultures and the ways they present themselves emotionally. I was intrigued to observe from a young age such differences, and it was this that spurred my desire to learn more about the ways mental health presentations vary worldwide, and later my decision to join the Transcultural Psychiatry Special Interest Group at the Royal College of Psychiatrists. No one person is immune from mental illness. And whilst with physical illness the symptoms can be categorised rather distinctly, the presentations for psychiatric illnesses often vary significantly between cultures. It is therefore essential we understand them as much as possible. 1 TPSIG NEWSLETTER ROYAL COLLEGE OF PSYCHIATRISTS 1ST JAN 2015 My ethnic origin comes with both pros and cons in my practice as a psychiatrist. Whilst the former far outweighs the latter, inevitably there will be patients who resent seeing a doctor who either looks foreign or has a foreign sounding name. Thankfully, such personal experiences have been few and far between. On the other hand, being of similar background to your patient can help put them at ease and be advantageous to the doctor-patient relationship. It is often easier to confide in someone if we feel we have something in common with them. I have been struck by my observations of cultures where mental health is very much a new field. The stigma that comes with psychiatric illness is, sadly, very much a global problem. I've realised this in my own culture, where people will deny emotional problems for fear of being perceived as weak. The threat of losing their pride is too big a risk to take. But we all know that when mental illness is suppressed it has other ways of manifesting, psychosomatically being just one example. Far better to have a physical illness in some places than to admit a defect of your mind. I have just returned from Cambodia, where this problem is far too common. Mental health is neglected. Life goes on. Regardless of our differing backgrounds, as psychiatrists we must recognise the importance of understanding the cultural differences in the patient in front of us, remembering that even though their ethnic makeup may be different from ours, the language of empathy is universal and can be understood by all. We must strive for each and everyone of our patient's voices to be heard and promote their ability to express themselves. We must empower them. Dr Lena Jawad is a CT3 currently working in CAMHS in Central London. Her final core training placement will be in Forensic Psychiatry at Broadmoor Psychiatric Hospital. She has a strong interest in global mental health. 2