EPSDT Behavioral Therapy—Continued Stay Review
advertisement

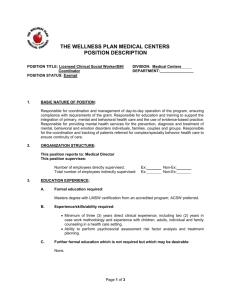
Service Request Application (SRA) for: Early and Periodic Screening and Diagnostic Treatment (EPSDT) BEHAVIORAL THERAPY CONTINUED STAY ALL ITEMS ARE REQUIRED After response is entered, use the Tab key to advance to next item. MEMBER INFORMATION PROVIDER INFORMATION Member First Name Member Last Name Medicaid Number Member Date of Birth Gender Male Female Member Address City, State & Zip Code Provider Name Clinical Contact Name Provider MIS# Provider Tax ID# Provider NPI Provider Phone Provider eMail Service Address City, State & Zip Code CLINICAL INFORMATION Procedure Code Primary Diagnosis Secondary Diagnosis Requested Units Requested Start Date Requested End Date 1. Have you submitted an SRA for this service and for this member within the last 30 days which was not approved? Yes No a. If yes, describe what changes have occurred to indicate that this service is now necessary: 2. Admission Date: 3. Is this a Service Transfer Request? Yes No a. If yes, do not complete this form; please complete the EPSDT Behavioral Therapy Service Transfer Request Form instead. 4. Requested number of weekly hours: a. Number of hours for direct therapy time: b. Number of hours for clinical supervision: c. Number of hours for service coordination: d. Other (list type of activity and hours): Revised 9/2/2014 ®Magellan Healthcare, Inc. Page 1 of 3 5. Treatment Summary and Letter of Medical Necessity: a. Did provider submit the Treatment Summary document to the treating physician? Yes No b. Did the treating physician authorize in writing medical necessity for the service based on the information contained in the Treatment Summary? Yes No c. Is the diagnosis a DSM defined diagnosis that is relevant to the need for treatment? Yes No d. Did the treating physician’s recommendations describe the member’s clinical need for behavioral modification services and confirm the diagnosis? Yes No e. If no to any of the above, please explain: 6. Please submit the updated Treatment Plan Summary document signed and approved by the treating physician. 7. Describe how the current therapy protocol is impacting the member’s clinical progress. Please include baseline and performance data that demonstrates the efficacy of the current therapy objectives. Data should be presented with specific references to each goal and objective in the treatment plan. Compare and contrast current therapy data with baseline data measures: 8. Describe any service gaps and how the lapse in service affected treatment planning and progress, service coordination and family learning and family/caregiver involvement in the application of behavior modification practices: 9. Identify reasons the member’s continued therapy cannot be managed in a lower level of care: 10. Describe how service coordination served to facilitate treatment plan outcomes based on the assessed needs of the child and the desired service outcomes of the caregivers: 11. Describe how service coordination served to facilitate treatment plan outcomes based on the assessed needs of the child and the desired service outcomes of the caregivers: 12. Describe how referrals to medical services (such as Speech Therapy, Occupational Therapy, Physical Therapy, Neurological services and Psychiatric services) have impacted the overall progress and generalization of skills gained from behavioral therapy services: 13. Describe progress regarding specific family involvement goals and objectives including a description of the methods used to measure progress within each goal area: 14. Describe progress toward achieving educational goals with other care providers (e.g., Medicaid Waiver funded Attendants, Relatives, etc.) who routinely come in contact with the child: Revised 9/2/2014 ®Magellan Healthcare, Inc. Page 2 of 3 15. Describe the generalization of adaptive functioning in multiple settings and describe the progress toward the anticipated date of discharge from services including all fading and consultative actions as planned: 16. Is the member/parent/guardian willing and medically stable to participate in services? Yes No 17. Describe the ongoing need to have a clinician involved with the family to provide behavioral therapy and define why services cannot be provided at a lower level of care: 18. Has there been meaningful or measurable improvement documented in the member’s behavior(s)? Yes No a. If yes, please describe: b. If no, please explain: 19. Is treatment making symptoms persistently worse? Yes No a. If yes, please describe: 20. Has member achieved an adequate stabilization of the challenging behavior and less intensive modes of therapy are appropriate?? Yes No a. If no, please explain: 21. Has member demonstrated an inability to maintain long-term gains from the proposed plan of treatment? Yes No a. If no, please describe member’s ability: 22. Is the service authorization request for 20 hours or more per week? Yes No a. If yes, describe the schedule of activities used to structure the therapy sessions and describe how each activity will facilitate the implementation of the behavioral modification plan: Revised 9/2/2014 ®Magellan Healthcare, Inc. Page 3 of 3