Ramener la marge de profits sur la vente des médicaments à 15 %
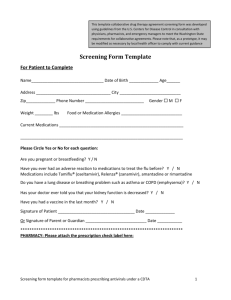
advertisement

Policy Brief The Pharmaceutical market in Mauritius: a case for stronger regulation. Mosadeq Sahebdin* For a population of 1.2 million inhabitants, it can be said that Mauritius has a high consumption rate of pharmaceutical products. This can be seen from the large number of drug importers, distributors and pharmacies on the island. The Mauritian population is known to be heavy drug users, due to the high rate of self-medication and the a pill for every ill mentality. It is not surprising therefore that some 24 companies import and distribute drugs and that there are 220 pharmacies over the island. At present, Mauritius spends about 2.8 percent of its GDP on health. Comparable figures for other countries are shown in following table. % of GDP on Health 14.0 12.0 % GDP 10.0 8.0 6.0 4.0 2.0 0.0 Madagascar Mauritius Singapore Seychelles UK New Zealand Belgium France USA The state health services employ over 650 doctors and 17 pharmacists. At primary care level, the state health services have 134 facilities, which provide medical, nursing, dispensary and support services at local level. In addition, there are 5 regional hospitals and three district hospitals. The private sector which absorbs 32% of the total expenditure on health in the country, employs over 400 doctors and provides primary and secondary services with 14 private clinics, 20 private medical laboratories and 275 private pharmacists. According to the WHO, Mauritius was performing in the health sector at about 70% of its potential, having regard to its level of expenditure on health. It ranked Mauritius at 84th out of 191 countries in overall achievement of the health system. At the end of 2001, there were in Mauritius 1,107 doctors, that is one doctor for every 1,089 inhabitants. Of those doctors, 694 (63%) were working in the public sector, and amongst these, 245 were specialists. There were 245 pharmacists, that is one for every 4,920 inhabitants. Of those, 17% were working in the public sector. According to a WHO report published this month, 9.3% of adults aged 18 and are diabetics 7.4% have arthritis 6.4% suffer from depression 4.6% have asthma, and 4.3% have cardiac ailments. These figures explain the high drug dependency among the population. According to the same WHO study, which started in 2003 in 16 other African countries, 32% of Mauritian households have to borrow or sell personal expenses to meet for medical expenses. 29.6% spend from their personal savings. 9% are in a catastrophic financial situation and their health expenses exceed their affordability by 40%. The study also reveals that 41.8% of expenses on health are used to buy drugs. Can we expect perfect competition? None of the assumptions of the theory of perfect competiton are applicable topharmaceuticals; hence we cannot expect price competition. Consumers do not choose to buy drugs. Price control However, some form of price regulation is necessary to provide for consumer protection and ensure supplies are available at a fair price. In Mauritius, the prices of drugs have always been controlled by the Ministry of Industry and Commerce. Government has fixed profit margins for importers, distributors and retailers respectively. Importers are allowed a profit margin of 9%, and 22% goes to retailers. Two years ago Government decided to decrease the respective profit margins. This raised an outcry from importers and pharmacists, who predicted the closing down of many pharmacies. One year later, it was business as usual, no closure had been registered. The prices of drugs used to be fixed on a six months’ basis. The method known as stabilising account allowed operators to recoup losses relative to fluctuations in exchange rate and enabled consumers to benefit from a specific price for at least six months. Three years ago, Government decided to change the method for calculation of drug prices. It has adopted the consignment basis method, enabling prices to be revised on each consignment. This has led to a disorderly market where similar drugs can be sold at two, sometimes three different prices in the same retail pharmacy. Some pharmacists have tried to abuse this situation by exacting new prices on former stocks. This has allowed some of them to exploit consumers’ ignorance of the fact that prices may differ from one retail outlet to the other and that patients do not normally shop around before buying drugs. Market concentration The root cause of high prices of drugs in Mauritius is the lack of competition on the market. There is too much concentration in the import and distribution market, leaving little chance to parallel importers and generic products. It is a cause for concern that big companies, representing multinationals tend to practice exclusive selling. Making the most of their huge logistic capacities, they can enjoy and make an abuse of their dominant position. As importers of famous brand names, they can exert an influence on the variety of drugs sold by the pharmacists. Hence it is not surprising that certain pharmacies do not stock generic products, thus depriving consumers of their right to choice. It is not uncommon for doctors working in private practice to prescribe exclusively brand names. On the other hand, it is not impossible for importers to claim, in invoices submitted to the price fixing unit, expenses which they may not have effected. As an example, Copharma may include in its costs brokers’ fees which it would not normally pay to the Rogers Cargo, as they form part of the same Rogers Group of Companies. In the same way, IBL Pharmaceuticals may enlarge its costs artificially by including brokers’ fees that they would normally not pay to Somatrans, a sister company. It has been alleged that such concentrations have led to the setting up of so-called black funds within companies, the proceeds of which have been used to finance political parties or in corruption. Irrational prescribing Irrational prescribing by physicians is one of the causes of the escalation of pharmaceutical budgets. Such practice include the heavy dependence of some prescribers on drug treatment for minor self-limiting complaints, overprescribing of certain types of drugs, prescribing of drugs of limited or no clinical value such as anti-diarrhoeals, prescribing expensive drugs when comparable but cheaper drugs are available and prescribing expensive brand forms. According to the Private Medical Practioners Association, doctors have to prescribe what they think best, irrespective of costs, because patients expect quick results. The other side of the coin is that most of the members of this association work in private practice, with patienst having a higher purchasing power. While these may not be considered as anti-competitive practices, some are related to anticompetitive behaviour on the part of importers and distributors. Knowing that doctors and pharmacies play a significant role in the sale of pharmaceutical products, companies often try to influence them, with huge incentives. Prescribing brand names and the sale of same are directly related to unfair promotional practices, such as offering gifts and so-called study tours to doctors. These gifts may range from calendars to pens, from bloc notes to dinners for the family in a five-star hotel and holidays abroad. On the other hand, the profit margins decided by Government tend to cause pharmacists to push brand names. The more the product is expensive, the higher will be the profits. Parallel importers also suffer from this same preference for brand names. While they import brand names from other sources than the manufacturers, they are able to sell at cheaper prices. Pharmacists would not often stock these products on the grounds of sub-standard quality, although what deters them is the low profit. On the other hand, consumer behaviour tends to encourage this situation. The high rate of selfmedication, as established by the WHO report, is related to the high drug dependency. Another factor which encourages pharmacists to stock brand names is the consumer perception that the more expensive the product the more efficient it is. Other practices that need to be addressed through regulation are the aggressive advertisement on food or vitamin supplements, the free sale of prescription-only drugs and doctors establishing their practice on the premises of pharmacies in violation of the Pharmacy Act. It has been regularly noted that, prior to end-of-year examinations, companies advertise and market vitamin supplements and so-called memory boosters aggressively. They often tend to abuse of the limitation of the law which interdicts advertisement of pharmaceuticals. As for the sale of prescription- only-drugs, the Pharmacy Act is clear on the restriction of their sale only on presentation of a prescription by a physician. Nevertheless, it is common practice for pharmacists to sell such products as antibiotics, over the counter. This unethical practice under- estimates the risks run by patientsconsumers. It has also been noted that, in spite of the provisions of the Pharmacy Act, many pharmacies have now secured, within their premises, a small medical cabinet where doctors examine patients in turn. While private doctors, estimated to be too many, are offered a place to reach more patients, pharmacies benefit from their proximity to push their products. In a large village in the east of Mauritius, competition among the 12 pharmacists seem to be fierce, at least six of them have put up partitions within their retail outlets to provide for dictors to receive patients. In one pharmacy, in the town of Vacoas, patients are seen by a doctor on a mezzanine installed under the ceiling of the pharmacy. Such unethical and illegal practices are equivalent to unfair competition to the disadvantage of pharmacists who abide by the law. Regulatory framework Drugs prices are fixed by the Price Fixing Unit of the Ministry of Industry and Commerce. Enforcement of the Pharmacy Act, relevant to marketing practices is the responsibility of the Pharmacy Board, which comprises of the Director of Pharmaceutical Services, government pharmacists and representatives of the Pharmacist Association. Consumers are not represented on this board. Import permits are delivered by the Ministry of Industry and Commerce, upon recommendations from the Trade and Therapeutics Committee. This also comprises of Government Officials and representatives of importers and private pharmacists. Consumer organizations are not represented. It is a matter of concern to consumers that the Trade and Therapeutics Committee is heavily dependent on external bodies such as the US FDA, to allow or interdict drugs on the local market. According to Professor Luc Montagnet, who is thepresident of the Institute for Reseach on Aids, in France, the FDA receives funds from laboratories. This explains their unwillingness to issue interdiction orders against such dangerous drugs as Vioxx. Recommendations. There is an urgent need for Government to formulate a National Drugs Policy after consultations with all parties concerned. In the absence of such an official stand, the private sector operators tend to set their rules on the market. More so, in the present context where political party funding seems to be accepted as a normal practice. This is a cause for concern to consumers. But still, this is no surprise when it has been said that the FDA fund political campaigns to the tune of US $ 21 million. National Drug Policies, should it be recalled, provide the framework within which essential drugs of acceptable quality, safety and efficacy will be made available to all those who need them at prices they can afford. Along the same lines, it can be expected that the WHO Essential Drugs List is effectively used as a tool to curtail high drug prices. In Mauritius, as in some other countries, the Essential Drug List is used only in the public sector. The private sector, in its endeavour to control a major market share of pharmaceuticals consistently refuses to accept the List. Vested interests have also contributed to lead consumers to believe that essential drugs are cheap, hence second-class drugs for the poor. Government should encourage parallel importers. A major campaign to encourage the use of generic products is imperative. There is an urgent need for civil society organizations to stand in unison on the drug price front. In view of consumers’ general indifferent attitude, even if the two consumer organizations joined forces, they would not influence Government decisions as opposed to the strong business lobby. A civil society network will contribute to further consumer awareness on rational drug use and bring a change in mentality. It is interesting to note that Government intends to set up a National Health Complaints Comission to investigate into consumer complaints. It will be impossible to address unethical practices without the support of prescribers. The Medical Council Act does not provide for the Council to regulate issues relative to prescription. The setting up of a regulatory mechanism which takes into account the peculiarity of the pharmaceuticals market is becoming urgent. Such a regulatory authority would include a mechanism to regulate behaviour of doctors, as well as distributors, including pharmacists at the retail level. Government’s proposal to set up a Pharmacy Council to regulate the activities of the profession and establish a Code of Ethics for the profession is noteworthy. Reference Ministry of Health, White Paper for the Health Sector Reform, Government of Mauriitus, 2003. Dr K. Balasubramanaian, Health and pharmaceuticals in Developing countries: Towards social justice and Equity, Consumers International, 1996 Nitya Nanda and Amr Ullah Khan , Competition Policy for the Pharmaceuticals Sector in India, Towards a Functional Competition Policy for India, an overview, edited by Pradeep S. Mehta, CUTS International,…. ICP Press releases. * The author is the Coordinator of the Institute for Consumer Protection, Mauritius. .