MONTHLY CDS DOCUMENTATION PEARLS – MARCH/APRIL
advertisement
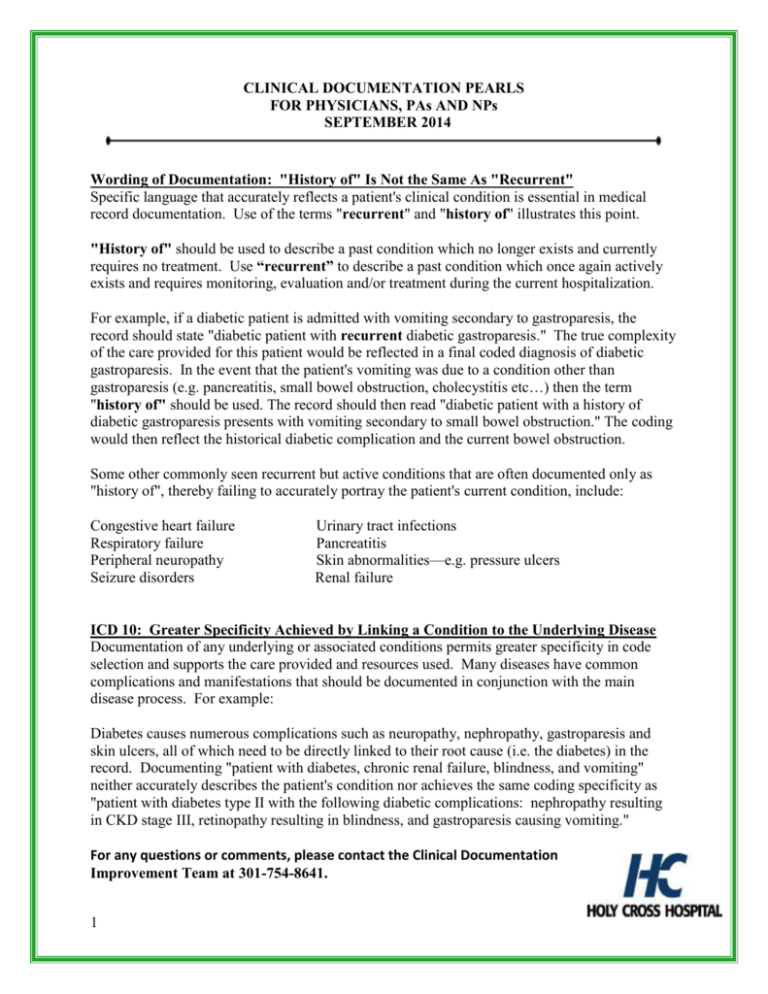
CLINICAL DOCUMENTATION PEARLS FOR PHYSICIANS, PAs AND NPs SEPTEMBER 2014 Wording of Documentation: "History of" Is Not the Same As "Recurrent" Specific language that accurately reflects a patient's clinical condition is essential in medical record documentation. Use of the terms "recurrent" and "history of" illustrates this point. "History of" should be used to describe a past condition which no longer exists and currently requires no treatment. Use “recurrent” to describe a past condition which once again actively exists and requires monitoring, evaluation and/or treatment during the current hospitalization. For example, if a diabetic patient is admitted with vomiting secondary to gastroparesis, the record should state "diabetic patient with recurrent diabetic gastroparesis." The true complexity of the care provided for this patient would be reflected in a final coded diagnosis of diabetic gastroparesis. In the event that the patient's vomiting was due to a condition other than gastroparesis (e.g. pancreatitis, small bowel obstruction, cholecystitis etc…) then the term "history of" should be used. The record should then read "diabetic patient with a history of diabetic gastroparesis presents with vomiting secondary to small bowel obstruction." The coding would then reflect the historical diabetic complication and the current bowel obstruction. Some other commonly seen recurrent but active conditions that are often documented only as "history of", thereby failing to accurately portray the patient's current condition, include: Congestive heart failure Respiratory failure Peripheral neuropathy Seizure disorders Urinary tract infections Pancreatitis Skin abnormalities—e.g. pressure ulcers Renal failure ICD 10: Greater Specificity Achieved by Linking a Condition to the Underlying Disease Documentation of any underlying or associated conditions permits greater specificity in code selection and supports the care provided and resources used. Many diseases have common complications and manifestations that should be documented in conjunction with the main disease process. For example: Diabetes causes numerous complications such as neuropathy, nephropathy, gastroparesis and skin ulcers, all of which need to be directly linked to their root cause (i.e. the diabetes) in the record. Documenting "patient with diabetes, chronic renal failure, blindness, and vomiting" neither accurately describes the patient's condition nor achieves the same coding specificity as "patient with diabetes type II with the following diabetic complications: nephropathy resulting in CKD stage III, retinopathy resulting in blindness, and gastroparesis causing vomiting." For any questions or comments, please contact the Clinical Documentation Improvement Team at 301-754-8641. 1