Gastroparesis: Pathophysiology and
management
Preceptor: Dr. Govind Makharia
Speaker: Dr. Moka Praneeth
Gastroparesis-Overview
Definition
Epidemiology
Pathophysiology
Clinical Manifestations
Diagnosis
Treatment
Definition
The diagnosis of gastroparesis is based on the combination
of
symptoms of gastroparesis,
absence of gastric outlet obstruction or ulceration
(documneted on UGIE or Barium swallow),
and documentation of delay in gastric emptying.
Michael Camilleri et al. Clinical Guideline: Management of Gastroparesis. Am J Gastroenterol 2013
Gastroparesis in Olmsted County, 1996–2006
Incidence
The age-adjusted prevalence of definite gastroparesis per 100,000
person was 9.6 (95% CI, 1.8–17.4) for men and 37.8 (95% CI, 23.2–52.4) for
women.
Incidence & prevalence of gastroparesis in India: ?
Jung HK et al. J Neurogastroenterol Motil. 2010
Gastroparesis: Etiology
Kendall and McCallum. Gastroenterology 1993.
Soykan et al. Dig Dis Sci 1998.
Electrophysiologic basis of gastric peristaltic waves
Gastric neuromuscular work after ingestion of a solid meal
Normal gastric emptying
The proximal stomach serves as the reservoir of food, and the
distal stomach as the grinder
Solids are initially retained in the stomach and undergo churning
while antral contractions propel particles toward the closed
pylorus.
Food particles are emptied once they have been broken down to
approximately 2 mm in diameter
Gastric neuromuscular disorders
Diabetic gastroparesis-pathophysiology
NOS – impaired expression
Gastric myenteric plexus of spontaneously diabetic
biobreeding /Worcester (BB/W) rats was studied
NANC relaxation in gastric muscle preparations in response
to transmural stimulation obtained from diabetic BB/W rats
was significantly impaired
Takahashi T et al. Gastroenterology. 1997 Nov
NOS – impaired expression
The number of NOS-immunoreactive cells in the gastric
myenteric plexus and the NOS activity were significantly reduced
in diabetic BB/W rats.
Northern blot analysis showed that the density of NOS
messenger RNA bands at 9.5 kilobases was significantly reduced
in the gastric tissues of diabetic BB/W rats.
Takahashi T et al. Gastroenterology. 1997 Nov
Watkins CC et al. J Clin Invest. 2000
Patterns of Gastric Emptying in Healthy People and in
Patients with Diabetic Gastroparesis
Idiopathic gastroparesis/IG – intact
vagal function
13 normal subjects, 9 patients of DG, 10 patients of IG, 5
patients of postsurgical gastroparesis
There were significantly decreased fasting levels of
pancreatic polypeptide and ghrelin in the diabetic
(79±26pg/ml) and postsurgical gastroparesis groups (51±11
pg/ml) compared to the normal subjects (315±76 pg/ml)
and the idiopathic gastroparesis group (161±53 pg/ml).
Gaddipati KV et al. Dig Dis Sci. 2006
IG – intact vagal function
Sham feeding was characterized by an increase in
pancreatic polypeptide levels in normal controls and
patients with idiopathic gastroparesis, with no change in
diabetic and postsurgical gastroparesis.
Meal ingestion resulted in an increase in pancreatic
polypeptide concentration in the normal subjects groups
and idiopathic gastroparesis group.
Gaddipati KV et al. Dig Dis Sci. 2006
IG & DG-cellular changes
Full-thickness gastric body biopsy specimens were
obtained from 40 patients with gastroparesis (20 diabetic)
and matched controls.
Sections were stained for H&E and trichrome and
immunolabeled with antibodies against PGP 9.5, nNOS,
VIP, substance P, and tyrosine hydroxylase to quantify
nerves, S100β for glia, Kit for ICCs, CD45 and CD68 for
immune cells, and smoothelin for smooth muscle cells.
Grover M et al. Gastroenterology. 2011 May
IG vs DG-cellular changes
Histologic abnormalities were found in 83% of patients.
The most common defects were loss of ICC with remaining ICC
showing injury, an abnormal immune infiltrate containing
macrophages, and decreased nerve fibers.
On light microscopy, no significant differences were found
between DG and IG with the exception of nNOS expression,
which was decreased in more patients with IG (40%) compared
with DG patients (20%) by visual grading.
Grover M et al. Gastroenterology. 2011 May
IG vs DG- Ultrastructural differences
Tissue was collected from anterior aspect of stomach,
midway between GC and LC where the gastroepiploic
vessels meet, at ~ 9 cm proximal to pylorus, from 20 DG, 20
IG and 20 patients undergoing gastric bypass for obesity
4 tissue strips for each patient 1 mm × 10 mm long and
containing the muscularis propria plus a small portion of
the tunica submucosa, were immediately cut after the full
thickness biopsy was obtained and processed for electron
microscopy
The NIDDK GpCRC J Cell Mol Med. 2012 July
IG vs DG- Ultrastructural differences
ICC were affected in both diabetic and idiopathic gastroparesis.
19/20 DG patients had a thickened basal lamina around smooth
muscle cells and nerves.
In contrast, tissues from 18/20 patients with IG did not have the
thickened basal lamina around smooth muscle cells and nerves
but had more intense fibrosis than those from DG
Nerve damage was much more prominent in IG with both nerve
cell bodies and nerve fibers affected to a greater degree.
Unlike in DG, glial cells were also abnormal in IG
The NIDDK GpCRC J Cell Mol Med. 2012 July
Clinical Manifestations
Nausea
92%
Vomiting
84%
Bloating
75%
Early Satiety
60%
Abdominal pain
45-90%
Rule out rumination syndrome
Soykan et al. Dig Dis Sci. 1998 Nov; 43(11):2398-404.
Dyspepsia & gastric emptying
In a meta analysis of 17 studies involving 868 dyspeptic
patients and 397 controls, significant delay of solid gastric
emptying was present in 40% of patients of FD1
Severity of delay does not correlate with symptoms
Rapid gastric emptying, rather than delayed gastric
emptying, might provoke functional dyspepsia.2
1. Perri F et al. Am J Gastroenterol 1993.
2. Kusano M et al. J Gastroenterol Hepatol. 2011 Apr
Gastroparesis: a proposed
classification
Grade 1: Mild gastroparesis
Symptoms relatively easily controlled
Able to maintain weight and nutrition on a regular diet
or minor dietary modifications
Grade 2: Compensated gastroparesis
Moderate symptoms with partial control with
pharmacological agents
Able to maintain nutrition with dietary and lifestyle
adjustments
Rare hospital admissions
Grade 3: Gastroparesis with gastric failure
Refractory symptoms despite medical therapy
Inability to maintain nutrition via oral route
Frequent emergency room visits or hospitalizations
Abell et al. Neurogastroenterol Motil (2006) 18, 263–283
Diabetic Gastroparesis (DG)
Prevalence of delayed emptying in longstanding Type-1 and
2 Diabetics: 27-58% and 30% respectively
Diabetic gastroparesis typically develops after DM has
been established for ≥10 years, and patients with type 1
diabetes might have triopathy
DG-natural history
20 patients (6 men and 14 women) of diabetes mellitus (16
with type-1 DM, 4 with Type-2 DM)
No differences in mean gastric emptying of the solid
component (retention at 100 minutes at baseline: 56% +/19% vs. follow-up: 51% +/- 21%, P = 0.23) or the liquid
component (time for 50% to empty at baseline: 33 +/- 11
minutes vs. follow-up: 31 +/- 12 minutes, P = 0.71) during
follow-up
Jones KL et al. Am J Med 2002
DG-natural history
Mean blood glucose (17.0 +/- 5.6 mmol/L vs. 13.8 +/- 4.9
mmol/L, P = 0.007) and HbA(1c) (8.4% +/- 2.3% vs. 7.6% +/1.3%, P = 0.03) levels were lower at follow-up.
There was no difference in symptom score (baseline: 3.9
+/- 2.7 vs. follow-up: 4.2 +/- 4.0, P = 0.78).
There was evidence of autonomic neuropathy in 7 patients
(35%) at baseline and 16 (80%) at follow-up.
Jones KL et al. Am J Med 2002
DG-natural history
Between 1984-89, 86 patients of DM underwent
assessment
Solid gastric emptying percentage of retention at 100 min)
was delayed in 48 (56%) patients and liquid emptying (50%
emptying time) was delayed in 24 (28%) patients.
At follow-up in 1998, 62 patients were known to be alive, 21
had died, and 3 were lost to follow-up.
1. Kong MF et al. Diabetes Care 1999
DG-natural history
In the group who had died, duration of diabetes (P = 0.048), score
for autonomic neuropathy (P = 0.046), and esophageal transit (P
= 0.032) were greater than in those patients who were alive, but
there were no differences in gastric emptying between the two
groups.
Of the 83 patients who could be followed up, 32 of the 45 patients
(71%) with delayed solid emptying and 18 of the 24 patients (75%)
with delay in liquid emptying were alive
Gastroparesis was not associated with a poor prognosis
Kong MF et al. Diabetes Care 1999
IG vs DG - Differences
Out of 416 patients, 254 patients of IG, 137 with DG and 25 with
other causes
More likely to be female (89% vs 71%-T1 vs 76%-T2), Caucasians (90%
vs 77% vs 76%)
Mean Age at enrollment: T2DM (53 ± 11) > IG (41 ± 14) > T1 DM (39
± 11 years)
Obesity in: T2 DM (71%) vs 28% (T1DM) vs IG (26%)
The NIDDK GpCRC. Clin Gastroenterol Hepatol. 2011
IG vs DG - Differences
Nausea and vomitings are the most common symptoms
prompting evaluation for DG
Abdominal pain was more often a symptom prompting
evaluation for IG (76% IG, 60% T1DM, 70% T2DM; p=0.01).
The NIDDK GpCRC. Clin Gastroenterol Hepatol. 2011
IG vs DG - Differences
20% having chronic but stable symptoms, 33% having
chronic but worsening symptoms, 33% having chronic
symptoms with periodic exacerbation, and 10% having a
cyclic pattern.
Patients with T1DM were more likely to have grade 3
gastroparesis severity (29% IG, 49% T1DM, 39% T2DM) and
had greater frequency of hospitalisations due to
dehydration
The NIDDK GpCRC. Clin Gastroenterol Hepatol. 2011
IG vs DG - Differences
The symptoms with highest severity at enrollment were stomach
fullness and postprandial fullness for IG, nausea for T1DM, and
stomach fullness for T2DM.
DG had more severe retching and T1DM had more severe
vomiting than IG
Severity of postprandial fullness and upper abdominal pain in: IG >
DG
The NIDDK GpCRC. Clin Gastroenterol Hepatol. 2011
IG vs DG - Differences
Gastric retention in: T1 DM (47 ± 27% at 4 hours) > T2 DM (33 ± 24) > IG
(28 ± 19)
IG had an increase in endometriosis and migraine headaches, whereas
T2DM had an increase in coronary artery disease.
An acute onset of symptoms was reported in approximately half of the
patients in each of the IG, T1DM, and T2DM.
An initial prodrome was present at the start of symptoms in a minority,
approximately 15% of cases, without significant differences among the
three groups.
The NIDDK GpCRC. Clin Gastroenterol Hepatol. 2011
Evaluation
Clinical Evaluation
Evaluate Volume Status
Abdominal distention, Succussion splash
Clues to other etiologies
Malar rash, sclerodactyly
Cachexia, lymphadenopathy
Lab
Electrolytes
Protein/albumin
Glucose
Thyroid/parathyroid
If suspected, autoantibodies for scleroderma, SLE,
polymyositis
Gastric emptying scintigraphy
Patient Preparation
NPO at least 3 hours prior to the
procedure
No smoking for 3 hours prior to the
procedure
Ensure that diabetics receive orange
juice 4-12 hrs before examination
Briefly explain to the patient:
The oral administration of the
radiotracer
Positioning and immobilization during
the imaging
Procedure
Time 1.5 hrs liquid, up to 3-4 hrs solid
Baseline solid Study:
Prepare one or two eggs/chicken liver/idli (in AIIMS) and mixed in
radiotracer
Stir and scramble
Or prepare choice of gastronomic vehicle with radiotracer
Administer to patient PO with 30-120 ml of water. Encourage
patient to eat quickly
Procedure (cont)
Patient Supine
Place patient in supine position.
Acquisition should be started as quickly
as possible after ingestion of food
Position camera anterior or LAO
Instruct patient to remain motionless
during imaging
Obtain Patient images every 5 minutes
up to 30 minutes, then every 15
minutes thereafter, allowing the
patient to ambulate between images
Or preset dynamic images for 60-90
minutes. Patient remain motionless
under camera
Supine is good for checking esophageal
reflux
Procedure (cont)
Patient standing
Position patient standing or sitting, one image facing
camera. Optional :one image with back to camera
Obtain immediate images, then every 10 minutes
Standing, sitting, then standing uses normal movement
and gravity to aid realism in study
Procedure Liquid Study
Baseline Liquid Study
Add 500 uci of 99mTc-DPA TO 120 ml,
of water or orange juice
Administer to patient PO, encourage
patient to drink quickly.
Images same as solid study, although
only imaged for 1.5 hours
Normal Results
Liquid (e.g., radiolabeled water or orange juice ) t1/2 (50%) at 10-15
minutes ) or 80% in 1 hour
Solid (Type and size of meals and population varies): t1/2 (50%) movement
out the stomach within a lower limit of 32 minutes to an upper limit of
120 min with and adult mean of 90 min.
Delayed GE (gastric retention) was determined to be >90% at 1 h, >60% at
2 h and>10% gastric retention at 4 h.
Terminate study before 60 min if gastric emptying becomes > 95%
Wireless motility capsule
Farmer A D et al. United European Gastroenterology
Journal 2013;2050640613510161
Farmer A D et al. United European Gastroenterology
Journal 2013;2050640613510161
Comparison of the various techniques, currently utilized, indicating their relative
advantageous and disadvantageous features.
Farmer A D et al. United European Gastroenterology
Journal 2013;2050640613510161
Clinical impact
The association of delayed emptying with specific symptoms is
relatively weak
Gastric emptying tests do not yield a high diagnostic specificity
With few exceptions, most studies have failed to demonstrate a
correlation between the severity of delayed emptying and
response to prokinetics
An initial treatment approach should be required before
performing gastric emptying test
In refractory patients or in those with symptoms that impair
nutritional status or the ability to function normally, assessment of
gastric emptying may play a pivotal role
Tack J et al. Best Pract Res Clin Gastroenterol. 2009
GERD-Gastric emptying study
Gastroparesis can be associated with and may aggravate
GERD.
Evaluation for the presence of gastroparesis should be
considered in patients with GERD that is refractory to acidsuppressive treatment.
Michael Camilleri et al. Clinical Guideline: Management of Gastroparesis. Am J Gastroenterol 2013
Treatment algorithm
Dietary/Non-medical
Poor evidence Multiple small meals
Liquid instead of solid meals
Low fat, Reduce indigestible fiber
Discontinue medications that slow emptying if possible
Nutrition
If oral intake is insuffi cient, then enteral alimentation by
jejunostomy tube feeding should be pursued (after a
trial of nasoenteric tube feeding).
Indications for enteral nutrition include :
unintentional loss of 10 % or more of the usual body
weight during a period of 3 – 6 months
repeated hospitalizations for refractory symptoms.
Michael Camilleri et al. Clinical Guideline: Management of Gastroparesis. Am J Gastroenterol 2013
Antiemetics
No evidence from controlled trials
Phenothiazines
Prochlorperazine (Stemetil)
Promethazine (Phenergan)
Serotonin 5-HT3 antagonists
Ondansetron (Zofran)
Muscarinic antagonisits
Butylscopolamine (Buscopan)
Prokinetics-algorithm
Metoclopramide (Maxalon)
Only FDA approved drug for gastroparesis
Erythromycin
Domperidone (Motilium/Vomidon)
Not FDA approved in US
Cisapride (Prepulsid)
Removed from market 2000
Cardiac toxicity
Pasricha et al. J Neurogastroenterol Motil, Vol.19
Endoscopic Therapy
Venting PEG
Botox injection – Pylorus
Pyloric Balloon Dilation (No published evidence)
Temporary placement of stimulation leads in stomach
to predict response to more permanent stimulator
Intrapyloric injection of Botox
23 patients (5 males, 19 idiopathic) underwent 2 UGIEs with 4
week interval
Injection of saline (in 11 as first injection) or botox 4×25 U (in 12
patients) in a cross-over RCT
Before the start of the study and 4 weeks after each treatment,
they underwent a solid and liquid gastric emptying breath test
with measurement of meal-related symptom scores, and filled out
the GCSI
Arts J et al. Aliment Pharmacol Ther. 2007
Intrapyloric injection of Botox
Significant improvement in emptying and GCSI was seen
after initial injection of saline or botox.
No further improvement occurred after the second
injection
No significant difference in improvements of solid t(1/2)
and liquid t(1/2), meal-related symptom scores or GCSI
Arts J et al. Aliment Pharmacol Ther. 2007
Surgical
Gastrostomy for venting and jejunostomy for
feeding
Completion gastrectomy in markedly symptomatic
PSG
Pyloroplasty (± jejunal feeding tube placement)
Subtotal gastrectomy + Roux-Y reconstruction for
gastric atony due to PSG)
Gastric Electrical Stimulation
Gastric Electric Stimulation
Gastric Neurostimulation (Enterra)
12 bpm
High Frequency (~ 4 x Slow Wave Freq)
Frequency
Low Energy with short pulse
Gastric Pacing:
3 bpm
Energy
Low Frequency (~ Slow Wave Freq)
High Energy with long pulse
Mechanisms of action of gastric
electrical stimulation
Unknown
Gastric emptying not consistently improved
Gastric dysrhythmias not normalised
Increased gastric accommodation
Increased vagal afferent activity
Increased thalamic activity
McCallum RW et al. Neurogastroenterol Motil
Enterra therapy: Humanitarian device
exemption
Enterra therapy was granted approval as a Humanitarian
Use Device (HUD) to be used in patients with refractory
diabetic or idiopathic gastroparesis, restricted to
institutions where Institutional review board approval has
been obtained
FDA 2000
Enterra therapy CE mark Indication
Enterra therapy is indicated for the treatment of patients
with chronic intractable (drug refractory) nausea and
vomitings secondary to gastroparesis
From: Gastric Electrical Stimulation: An Alternative Surgical Therapy for Patients With Gastroparesis
Arch Surg. 2005;140(9):841-848. doi:10.1001/archsurg.140.9.841
Figure Legend:
Diagrammatic representation of the laparoscopic placement technique showing trocar placement, lead placement in the stomach
wall, and position of the subcutaneous pocket for the neurostimulator.
Date of download: 1/30/2014
Copyright © 2014 American Medical
Association. All rights reserved.
Figure
4 Vomiting frequency
in patients
diabetic gastroparesis
after after implantation of a
Vomiting
frequency
in patients
withwith
diabetic
gastroparesis
implantation of a gastric electrical stimulator device
gastric electrical stimulator device
Permission obtained from Elsevier ©
McCallum, R. W. et al. Clin. Gastroenterol. Hepatol. 11, 947–954 (2010)
Hasler, W. L. (2011) Gastroparesis: pathogenesis, diagnosis and management
Nat. Rev. Gastroenterol. Hepatol. doi:10.1038/nrgastro.2011.116
Hasler, W. L. (2011) Gastroparesis: pathogenesis, diagnosis and management
Nat. Rev. Gastroenterol. Hepatol. doi:10.1038/nrgastro.2011.116
GES for the Treatment of Gastroparesis: A Meta-Analysis
Total Symptom Severity Score
13 papers
Requirement for Enteral or
Parenteral Nutritional Support
Vomiting Symptom Severity Score
Change in Weight (kg)
Nausea Symptom Severity Score
O’Grady G, et al. World J Surg 2009; 33:1693-1701
GES for the Treatment of Gastroparesis: A Meta-Analysis
Complications
8.3 %
(22/265 patients, 10/13 studies)
Infection
8
Skin erosion
6
Pain at site
4
Gastric perforation
2
Device migration
1
Volvulus
1
O’Grady G, et al. World J Surg 2009; 33:1693-1701
GES for the Treatment of Gastroparesis: A Meta-Analysis
A meta-analysis of 10 studies (n = 601) using high-frequency GES
to treat patients with gastroparesis from January 1995 to January
2011
GES significantly improved both TSS (P < 0.00001) and gastric
retention at 2 h (P = 0.003) and 4 h (P < 0.0001) in patients with
diabetic gastroparesis (DG), while gastric retention at 2 h (P =
0.18) in idiopathic gastroparesis (IG) patients, and gastric
retention at 4 h (P = 0.23) in postsurgical gastroparesis (PSG)
patients, did not reach significance.
Chu H et al. J Gastroenterol Hepatol. 2012
Glucose Control in Diabetic gastroparesis Patients
HbA1c Reduction
at 6 and 12 months vs. Baseline
10.0%
Baseline 9.8%
Baseline 9.4%
9.0%
At 6 mths
At 6 mths
At 12 mths
8.5%
Baseline 8.6%
•Forster et al: Further experience with gastric stimulation to
treat drug refractory gastroparesis. Am J Surgery 2003;
186(6): 690-695
At 12 mths
8.4%
8.0%
•Lin et al: Treatment of Diabetic Gastroparesis by HighFrequency Gastric Electrical Stimulation. Diabetes Care 2004;
27(5), 1071-1076.
7.0%
At 12 mths
6.5%
At 6 mths
6.0%
Forster 2003
Lin 2004
Van der Voort
2005
•Van Der Voort et al: Gastric Electrical Stimulation Results in
Improved Metabolic Control in Diabetic Patients Suffering
From Gastroparesis. Exp Clin Endocrinol Diabetes 2005;
113:38-42
Nutritional Support
Nutritional Support Reduction
Patient Number
25
20
9
15
TPN
10
J-tubes
5
13
5*
* p < 0.05
0
Baseline
12 mths
48
28
n
Lin et al: Treatment of Diabetic Gastroparesis by High-Frequency Gastric
Electrical Stimulation. Diabetes Care 2004; 27(5), 1071-1076
Conclusion
More studies on gastroparesis are warranted in India
WMC is as good and has advantages compared to gastric
emptying scintigraphy, the gold standard
GES is a good choice for refractory gastroparesis
Treatment options are likely to improve after the
pathophysiology of gastroparesis is better understood.
Thank you
WAVESS*: Study Design
Multicenter double blind crossover
ON
R
Baseline
a
n
d
Implant o
m
1/2
1/2
OFF
Phase I
0
N=
33
Phase II
1
2
33
33
6
12
Months
27
24
Patients
17 diabetic
16 idiopathic
* Worldwide Anti-Vomiting Electrical Stimulation Study
Gastric Electrical Stimulation
Enterra System (Medtronic)
The History of Gastric Stimulation
1972: Kelly and Laforce at Mayo Clinic induced antegrade and retrograde
conduction of slow waves in canines with gastric stimulation.
1988: McCallum et al at University of Virginia showed increased gastric
emptying in canines with vagotomy
1997: Familoni et al reported improved peristalsis in canines with GES
1998: The WAVESS study group demonstrated the feasibility of GES, leading
to Enterra therapy.
The History of Gastric Stimulation
1963 – Bilgutay et al.: Gastric stimulation was practiced for
the treatment of postoperative ileus.
Surgery
Laparoscopy - 3 Ports
Left upper quadrant port becomes
stimulator pocket
Length of stay: 2-3 days
Evaluate neurostimulator parameters
before discharge
Lead Location
Greater curvature
Leads placed
10cm from pylorus
Utilize measuring
tape or 10cm suture
length
Leads 1cm apart
Lead Placement
Proximal anchoring
point utilizing
winged/trumpet anchor
One centimeter
electrode length in
stomach wall
Lead Fixation
Disc sutured to
stomach wall
1-2 sutures
Lead suture wire
clipped to disc
1-2 clips
Switch on and interrogation
Device is initiated
remotely
A system check is
performed and
impedance is checked
Power setting is
programmed and
rechecked on
discharge
Comparison of methods used to assess gastric
emptying
Parkman et al. Neurogastroenterol Motil. 2010 Feb
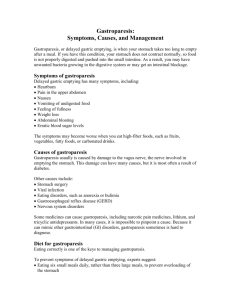
Gastroparesis: Pathophysiology
Excessive
relaxation
Poor
antro-pyloro-duodenal
synchronisation
Abnormal
duodenal
motility
Antral
hypomotility