P110 (RA6073) - British Renal Society
advertisement
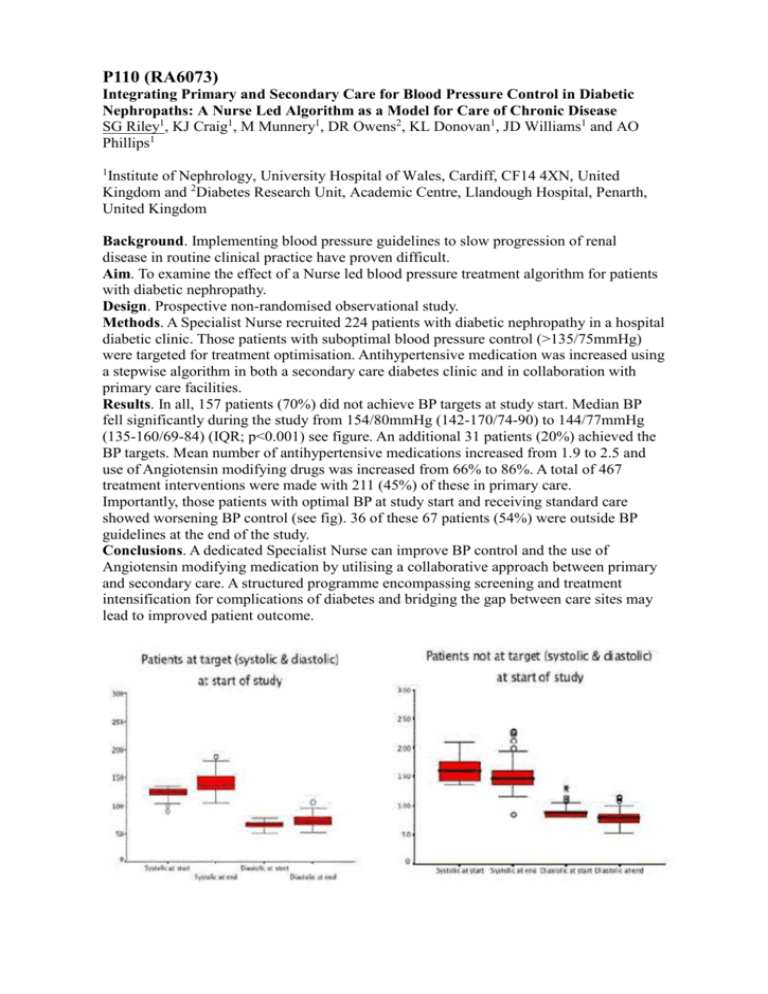
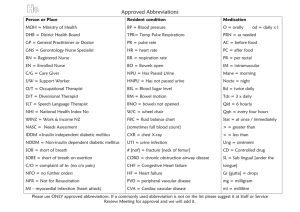
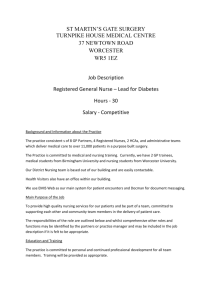
P110 (RA6073) Integrating Primary and Secondary Care for Blood Pressure Control in Diabetic Nephropaths: A Nurse Led Algorithm as a Model for Care of Chronic Disease SG Riley1, KJ Craig1, M Munnery1, DR Owens2, KL Donovan1, JD Williams1 and AO Phillips1 1 Institute of Nephrology, University Hospital of Wales, Cardiff, CF14 4XN, United Kingdom and 2Diabetes Research Unit, Academic Centre, Llandough Hospital, Penarth, United Kingdom Background. Implementing blood pressure guidelines to slow progression of renal disease in routine clinical practice have proven difficult. Aim. To examine the effect of a Nurse led blood pressure treatment algorithm for patients with diabetic nephropathy. Design. Prospective non-randomised observational study. Methods. A Specialist Nurse recruited 224 patients with diabetic nephropathy in a hospital diabetic clinic. Those patients with suboptimal blood pressure control (>135/75mmHg) were targeted for treatment optimisation. Antihypertensive medication was increased using a stepwise algorithm in both a secondary care diabetes clinic and in collaboration with primary care facilities. Results. In all, 157 patients (70%) did not achieve BP targets at study start. Median BP fell significantly during the study from 154/80mmHg (142-170/74-90) to 144/77mmHg (135-160/69-84) (IQR; p<0.001) see figure. An additional 31 patients (20%) achieved the BP targets. Mean number of antihypertensive medications increased from 1.9 to 2.5 and use of Angiotensin modifying drugs was increased from 66% to 86%. A total of 467 treatment interventions were made with 211 (45%) of these in primary care. Importantly, those patients with optimal BP at study start and receiving standard care showed worsening BP control (see fig). 36 of these 67 patients (54%) were outside BP guidelines at the end of the study. Conclusions. A dedicated Specialist Nurse can improve BP control and the use of Angiotensin modifying medication by utilising a collaborative approach between primary and secondary care. A structured programme encompassing screening and treatment intensification for complications of diabetes and bridging the gap between care sites may lead to improved patient outcome.