Maternal/Fetal/Neonatal Effects of Alcohol and
advertisement
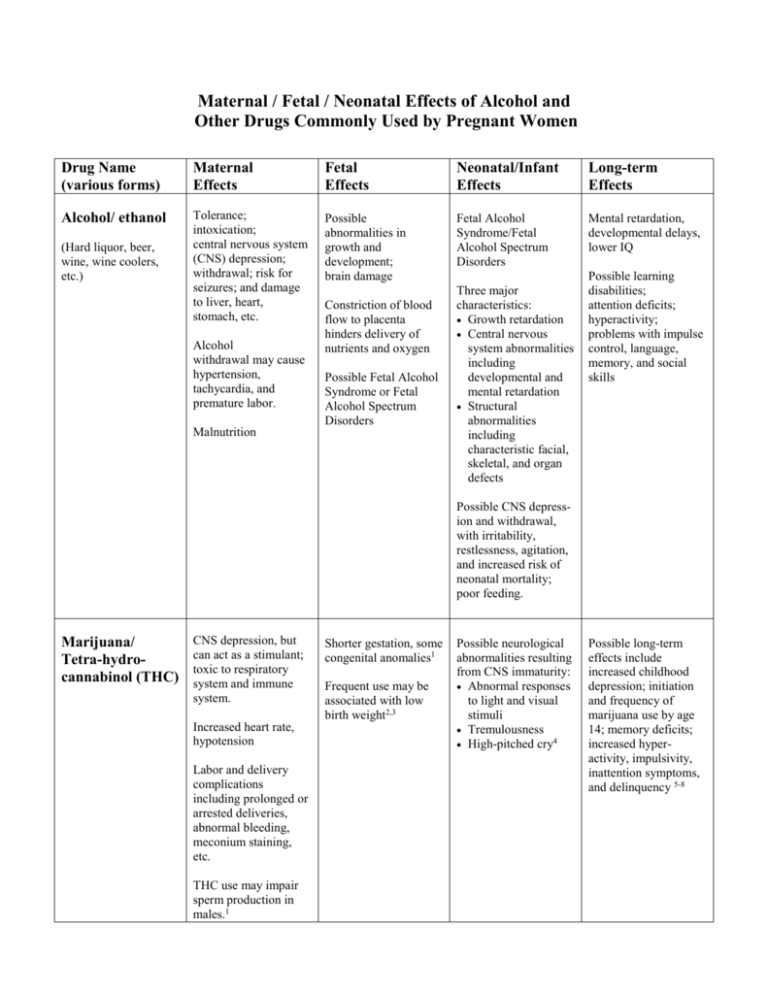
Maternal / Fetal / Neonatal Effects of Alcohol and Other Drugs Commonly Used by Pregnant Women Drug Name (various forms) Maternal Effects Fetal Effects Neonatal/Infant Effects Long-term Effects Alcohol/ ethanol Tolerance; intoxication; central nervous system (CNS) depression; withdrawal; risk for seizures; and damage to liver, heart, stomach, etc. Possible abnormalities in growth and development; brain damage Fetal Alcohol Syndrome/Fetal Alcohol Spectrum Disorders Mental retardation, developmental delays, lower IQ (Hard liquor, beer, wine, wine coolers, etc.) Alcohol withdrawal may cause hypertension, tachycardia, and premature labor. Constriction of blood flow to placenta hinders delivery of nutrients and oxygen Possible Fetal Alcohol Syndrome or Fetal Alcohol Spectrum Disorders Malnutrition Three major characteristics: Growth retardation Central nervous system abnormalities including developmental and mental retardation Structural abnormalities including characteristic facial, skeletal, and organ defects Possible learning disabilities; attention deficits; hyperactivity; problems with impulse control, language, memory, and social skills Possible CNS depression and withdrawal, with irritability, restlessness, agitation, and increased risk of neonatal mortality; poor feeding. Marijuana/ Tetra-hydrocannabinol (THC) CNS depression, but can act as a stimulant; toxic to respiratory system and immune system. Increased heart rate, hypotension Labor and delivery complications including prolonged or arrested deliveries, abnormal bleeding, meconium staining, etc. THC use may impair sperm production in males.1 Shorter gestation, some congenital anomalies1 Frequent use may be associated with low birth weight2,3 Possible neurological abnormalities resulting from CNS immaturity: Abnormal responses to light and visual stimuli Tremulousness High-pitched cry4 Possible long-term effects include increased childhood depression; initiation and frequency of marijuana use by age 14; memory deficits; increased hyperactivity, impulsivity, inattention symptoms, and delinquency 5-8 Maternal/Fetal/Neonatal Effects of Alcohol and Other Drugs Drug Name (various forms) Maternal Effects Fetal Effects Neonatal/Infant Effects Long-term Effects Prescription sedativehypnotics Tolerance, CNS depression Drug accumulates in fetus at greater levels than in mother1 Long-term effects not known Low birth weight10 Drug and metabolites may remain in newborn for days or weeks longer than in the mother. May result in lethargy, poor muscle tone, sucking difficulties, or even CNS depression1 Increased risk for cleft lip or palate11 Withdrawal may occur11 (e.g., Valium, Xanax, Halcion, etc.) Respiratory depression1 Acute withdrawal with risk of premature labor9,10 Fetal depression, abnormal heart rhythm or even death1 Increased risk for hypoglycemia and respiratory problems10 Amphetamines/ Stimulants CNS and cardiovascular stimulation: increased heart rate increased blood pressure vascular constriction Anorexia, weight loss, insomnia Possible growth retardation and fetal hypoxia Possible withdrawal or intoxication Long-term effects not known Low birth weight13 Possibility of cleft lip and palate, intrauterine fetal demise, fetal distress, and placental abruption12 Adequate studies lacking Decreased blood flow to placenta Risk of HIV/AIDS with intravenous use12 Cocaine, crack cocaine CNS and cardiovascular stimulation: increased heart rate increased blood pressure vascular constriction Pregnancy associated with increased sensitivity to cocaine12 Growth retardation3; many children experience catch-up growth and are normal weight by 6-12 months14 Fetal hypertension and distress12 Risk for intrauterine stroke1 Intoxication and/or withdrawal. Symptoms may include: irritability/agitation increased tone tremors jitters inconsolability increased respiration15 Possible developmental delays Possible long-term deficits in attention and learning17 Possible risk for seizures16 Adapted from SAMHSA/CSAP Technical Report, No. 7, 1993. Institute for Health and Recovery, 2009 Maternal/Fetal/Neonatal Effects of Alcohol and Other Drugs Drug Name (various forms) Maternal Effects Fetal Effects Neonatal/Infant Effects Cocaine, crack cocaine (continued) Decreased blood flow to placenta Possible genito-urinary abnormalities Slower drug excretion in newborn Possible placental abruption and bleeding Necrotizing enterocolitis1 Abnormal sleep and ventilatory patterns1 Tolerance, CNS depression Intrauterine growth retardation Risk for HIV/ AIDS and other infections with injection drug use Risk of HIV/AIDS infection from mother Addiction and Neonatal Narcotic Withdrawal Syndrome. Symptoms may include: hyperactivity irritability/agitation high-pitched cry increased neuromuscular tone tremors seizure risk Long-term Effects Premature labor3,12 Possible growth retardation and fetal hypoxia12 Heroin, opiates Low birth weight3 Malnutrition 12 Acute withdrawal and risk for spontaneous abortion or premature labor18 Possible long-term neurobehavioral deficits Poor feeding Abnormal sleep and ventilatory patterns HIV/AIDS risk19 Growth retardation Cigarettes (nicotine and other compounds in smoke) CNS stimulation and respiratory damage Reduced fetal oxygen supply Smaller head circumference23 Impaired fetal growth20 Increased risk for fetal distress, fetal demise, spontaneous abortion, and premature labor21,22 Prenatal cessation reduces risk of preterm birth and delivering small for gestation age neonates24 Abnormal nursing Possible increase in disruptive behavior, oppositional defiant disorder, and serious delinquency26 Increased risk of asthma27 Possible impairment of language development28 Risk for congenital palate and heart defects25 Adapted from SAMHSA/CSAP Technical Report, No. 7, 1993. Institute for Health and Recovery, 2009 Maternal/Fetal/Neonatal Effects of Alcohol and Other Drugs This document has been adapted from Pregnancy and Exposure to Alcohol and Other Drug Use. CSAP Technical Report, No. 7, published in 1993 by the Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Prevention. Wherever possible, we have updated the references to reflect more current trends in research. References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Prevention. (1993). Pregnancy and exposure to alcohol and other drug use. CSAP Technical Report, No.7. Rockville, MD: Author. Hurd, Y.L., Wang, X., Anderson, V., Beck, O., Minkoff, H., & Dow-Edwards, D. (2005). Marijuana impairs growth in mid-gestation fetuses. Neurotoxicology & Teratology, 27, 221-229. Schempf, A.E. (2007). Illicit drug use and neonatal outcomes: A critical review. Obstetrical and Gynecological Survey, 62, 749-757. Huizink, A.C., & Mulder, E.J.H. (2005). Maternal smoking, drinking or cannabis use during pregnancy and neurobehavioral and cognitive functioning in human offspring. Neuroscience & Biobehavioral Reviews, 30, 24-41. Gray, K.A., Day, N.L., Leech, S., & Richardson, G.A. (2005). Prenatal marijuana exposure: Effect on child depressive symptoms at ten years of age. Neurotoxicology & Teratology, 27, 439-448. Day, N.L., Goldschmidt, L., & Thomas, C.A. (2006). Prenatal marijuana exposure contributes to the prediction of marijuana use at age 14. Addiction, 101, 1313-1322. Justras-Aswad, D., DiNieri, J.A., Harkany, T., & Hurd, Y.L. (in press, 2009). Neurobiological consequences of maternal cannabis on human fetal development and its neuropsychiatric outcome. European Archives of Pyschiatry & Clinical Neuroscience. Goldschmidt, L., Day, N.L., & Richardson, G.A. (2000). Effects of prenatal marijuana exposure on child behavior problems at age 10. Neurotoxicology & Teratology, 22, 325-336. Davis, R.L., Rubanowice, D., McPhillips, H., Raebel, M.E., Andrade, S.E., Smith, D., et al. (2007). Risks of congenital malformations and perinatal events among infants exposed to antidepressant medications during pregnancy. Pharmacoepidemiology & Drug Safety, 16, 1086-1094. Wikner, B.N., Stiller, C.-O., Bergman, U., Asker, C., & Kallen, B. (2007). Use of benzodiazepines and benzodiazepine receptor agonists during pregnancy: neonatal outcome and congenital malformations. Pharmacoepidemiology and Drug Safety, 16, 1203-1210. Iqbal, M.M., Sobhan, T., & Ryals, T. (2002). Effects of commonly used benzodiazepines on the fetus, the neonate, and the nursing infant. Psychiatric Services, 53, 39-49. Kuczkowski, K.M. (2007). The effects of drug abuse on pregnancy. Current Opinion in Obstetrics & Gynecology, 19, 578-585. Smith, L.M., LaGasse, L.L., Derauf, C., Grant, P., Shah, R., Arria, A., et al. (2006). The infant development, environment, and lifestyle study: Effects of prenatal methamphetamine exposure, polydrug exposure, and poverty on intrauterine growth. Pediatrics, 118, 1149-1156. Lumeng, J.C., Cabral, H.J., Gannon, K., Heeren, T., & Frank, D.A. (2007). Pre-natal exposures to cocaine and alcohol and physical growth patterns to age 8 years. Neurotoxicology & Teratology, 29, 446-457. Schuetze, P., Eiden, R.D., & Coles, C.D. (2007). Prenatal cocaine and other substance exposure: Effects on infant autonomic regulation at 7 months of age. Developmental Psychobiology, 49, 276289. Bauer, C.R., Langer, J.C., Shankaran, S., Bada, H.S., Lester, B., Wright, L.L., et al. (2005). Acute neonatal effects of cocaine exposure during pregnancy. Archives of Pediatrics & Adolescent Medicine, 159, 824-834. Adapted from SAMHSA/CSAP Technical Report, No. 7, 1993. Institute for Health and Recovery, 2009 Maternal/Fetal/Neonatal Effects of Alcohol and Other Drugs 17. Singer, L.T., Nelson, S., Short, E., Min, M.O., Lewis, B., Russ, S., et al. (2008). Prenatal cocaine 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. exposure: Drug and environmental effects at 9 years. The Journal of Pediatrics, 153, 105-111. Almario, C.V., Seligman, N.S., Dysart, K.C., Berghella, V., & Baxter, J.K. (in press, 2009). Risk factors for preterm birth among opiate-addicted gravid women in a methadone treatment program. American Journal of Obstetrics & Gynecology. Hamdan, A.H. (2009). Neonatal abstinence syndrome. Retrieved August 5, 2009, from http://owl.english.purdue.edu/owl/resource/560/10/. Pogodina, C., Brunner Huber, L.R., Racine, E.F., & Platonova, E. (in press, 2009). Smoke-free homes for smoke-free babies: The role of residential environmental tobacco smoke on low birth weight. Journal of Community Health. Meeker, J.D., Missmer, S.A., Vitonis, A.F., Cramer, D.W., & Hauser, R. (2007). Risk of spontaneous abortion in women with childhood exposure to parental cigarette smoke. American Journal of Epidemiology, 166, 571-575. George, L., Granath, F., Johannson, A.L.V., Anneren, G., & Cnattingius, S. (2006). Environmental tobacco smoke and risks of spontaneous abortion. Epidemiology, 17, 500-505. Winklbaur, B., Baewert, A., Jagsch, R., Rohrmeister, K., Metz, V., Jachmann, C.A., et al. (2009). Association between prenatal alcohol exposure and outcome of neonates born to opioid-maintained mothers. European Addiction Research, 15, 150-156. Polakowski, L.L., Akinbami, L.J., & Mendola, P. (2009). Prenatal smoking cessation and the risk of delivering preterm and small-for-gestation-age newborns. Obstetrics & Gynecology, 114, 318-325. Malik, S., Cleves, M.A., Honein, M.A., Romitti, P.A., Botto, L.D., Yang, S., et al. (2008). Maternal smoking and congenital heart defects. Pediatrics, 121, e810-e816. Wakschlag, L.S., Pickett, K.E., Kasza, K.E., & Loeber, R. (2006). Is prenatal smoking associated with a developmental pattern of conduct problems in young boys? Journal of the American Academy of Child & Adolescent Psychiatry, 45, 461-467. Cheraghi, M., & Salvi, S. (2009). Environmental tobacco smoke (ETS) and respiratory health in children. European Journal of Pediatrics, 168, 897-905. Sun, W., Hansen, A., Zhang, L., Lu, J., Stolzberg, D., & Kraus, K.S. (2008). Neonatal nicotine exposure impairs development of auditory temporal processing. Hearing Research, 245, 58-64. Adapted from SAMHSA/CSAP Technical Report, No. 7, 1993. Institute for Health and Recovery, 2009







