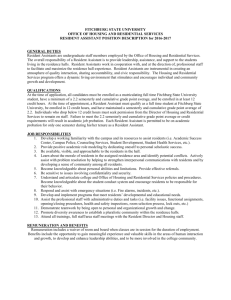
overview - community integration home (cih)
advertisement

COMMUNITY INTEGRATION HOME (CIH) OVERVIEW PROGRAM DESCRIPTION 1. PURPOSE: To provide community based residential and treatment services to Forensic Consumers with addictive diseases and mental illness transitioning from state hospitals to the community. 2. POPULATION: Adult Consumers who are served by hospital forensic services and whose legal status is either Not Guilty By Reason Of Insanity (NGRI), Civilly Committed Incompetent to Stand Trial (IST) or those who have been determined by the Forensic Team in conjunction with the criminal court to be in need of these services. 3. TREATMENT SERVICES: Mental Health Services such as medication management, day treatment, counseling and case management will be obtained through service providers in the community, generally Community Service Boards and other private providers. Substance Abuse services will be provided through contracted services in the community and will be tailored to meet each individual consumer’s needs. These services may be provided at the group home or at other locations. Twelve Step meetings in the community will be utilized. Residential rehabilitation and skill development training will occur at the group homes and at selected sites in the community, depending on the type of skill training. Residential Rehab services include budgeting, nutrition and food preparation, navigating in the community, health awareness (physical, dental health, sexually transmitted diseases etc.), interpersonal and communication skills training, medication training and support, symptom management, supportive counseling, and development of skills to access community-based services, both social and recreational. All services are individualized to the consumer’s needs. 4. LEVEL OF SUPERVISION: This program is designed to provide supervision by dedicated Resident Care Provider 24 hours per day, seven days per week when consumers are present in the group home. The level of planned skill development training or other activities at the home or in the community, such as planned outings, will determine the number of necessary staff in the group home at any given time. Consumers will not be permitted in the group home without staff supervision. A houseparent will provide coverage for those residents who are ill and are unable to attend their day program or other daytime activities. 5. TREATMENT OBJECTIVES: Overall treatment objectives and expected outcomes for the consumers are as follows: Skill development and restoration in functional areas which have previously interfered with ability to live in the community; ability to participate in educational, recreational, and social activities; employment (competitive or sheltered); ability to develop and maintain appropriate social relationships; and independent or semi-independent living. The Community Integration Home (CIH) is a residential program providing a safe structured residential environment for clients leaving Regional Hospital’s Forensic Units to transition to the community. The CIH is located in the general community (in a residential area) and serves a maximum of six clients. The program provides 7 days per week/24-hour supervision. The professional and para-professional staff provide therapeutic and supportive interventions designed to teach independent living skills in the least restrictive setting appropriate for these clients. The Team Leader works to link the client to support services in his community, as well. All clients are engaged in paid employment, work training, educational or day treatment activities during the daytime, as appropriate to their individual strengths and needs. The length of stay is variable, depending on the needs of the individual client and their response to transition to the community. As clients adjust to community living, they may participate in increasingly independent activities and privileges. These privileges afford them a residential setting that offers the greatest freedom possible, given their individual circumstances, and may permit them to transition into even less restrictive settings in the future such as Personal Care homes and Supervised apartments. DEFINITIONS NGRI – Not Guilty by Reason of Insanity. IST – Incompetent to Stand Trial Civilly-committed IST – An individual who has been found incompetent for trial, whose competence is not likely to be restored, and whom the court has committed. Transition – Movement from inpatient status to community residence with the permission of the court for trial visits. This step is often an intermediate step between inpatient status and either Conditional Release or Community Release. Conditional release – Release of an NGRI patient from inpatient status to full-time community residence with the express permission of the court for such release. These patients continue to be monitored by the REGIONAL HOSPITAL Conditional release team or designee or designee. Conditions of the release are spelled out on the Conditional Release Plan. Community release - Release of civilly- committed IST patient from inpatient status to full-time community residence with the express permission of the court for such release. Conditions of the release are spelled out on the Community Release Plan. (Generally a Bond with conditions that is monitored by a court official.) ADMISSION CRITERIA Only male clients 18 years old or older are eligible to reside at the CIH. The client will have successfully completed a course of treatment at a DHR forensic inpatient facility in the state of Georgia, and will have been deemed by the treatment team of that facility to be appropriate for transition to a less restrictive environment. The client will have a valid court order that permits overnight stays in a community residence of up to one week, or a valid conditional release/community release order that permits residence in the CIH. The client must not be actively suicidal or homicidal. The client must not meet criteria, in the view of his treatment team, for transition to a less restrictive setting than the CIH (i.e., he must not be considered appropriate for a personal care home, supervised apartment, independent living, or family residence at the time of discharge from a REGIONAL HOSPITAL). REFERRAL PROCESS Referrals are made by a Regional Hospital’s Forensic Services Department. Referrals are made via one of the following avenues, and always in the setting of a valid court order permitting such a transition: By the treatment team of a REGIONAL HOSPITAL’S Secure Units, when a client is deemed ready to begin transition to the community. By the treatment team of another Regional Hospital’s Forensic Services Department, when a client there has been deemed ready to begin transition to the community, and in the event that the client’s home community is located within the referred REGIONAL HOSPITAL catchments area. In this case, the referral will mandate a staffing between the two facilities regarding such a transition, and will not proceed unless all parties agree such a step is appropriate. By the conditional release team or designee of a REGIONAL HOSPITAL’S Forensics Service, in the event that a client has not successfully transitioned elsewhere and appears to require more residential support and structure. A member of the REGIONAL HOSPITAL treatment team will schedule a pre-transition meeting with the referred REGIONAL HOSPITAL treatment team, the Conditional Release Coordinator or designee, the CIH Team Leader and other appropriate persons to discuss the referral. In the event that a conditional release/community release patient is being referred from another placement to the CIH, REGIONAL HOSPITAL treatment team members will not attend, but the REGIONAL HOSPITAL Conditional Release Coordinator or designee will attend. If the client is assesses to meet CIH admission criteria, and is assessed to be ready to begin transition or full-time residence, and there is a vacancy at the CIH, an admission date is scheduled. The client may have a preplacement visit to the CIH prior to the admission date. ADMISSION PROCESS Once a resident is assessed to be appropriate for the CIH, a transition period generally begins during which he will receive a series of trial visits over an agreed-upon time period. Visits will become gradually longer until the client is ready to begin full-time residence. In some cases, (such as movement of an existing conditional release patient, or placement of a client for whom transition is thought to be clinically contraindicated) there will be no transition period, or a highly truncated transition period. Once an admission date is set, the client will be asked to sign paperwork for the group home, and assist in developing his treatment plan there. The resident will be required to have a physical examination within six months prior to admission to the CIH, as well as placement of a PPD or, in the event of a previously positive PPD, documentation of the most recent negative chest x-ray. The REGIONAL HOSPITAL Forensic Services staff will be responsible for providing these materials to the staff of the CIH. Residents may bring their own comforter, pillow, hygiene supplies, radios and other personal belongings to make their rooms more comfortable, although many of these are provided by the CIH. All belongings brought to the CIH by the resident must conform to the CIH guidelines. VISITING, HOME PASSES AND PHONE CONTACT Visiting Family members, attorneys, clergy and other community support individuals are encouraged to visit during routine visiting hours, as follows: Sunday and Major Holidays, 12:00 noon to 4:00 P.M. Visiting during program activities is not permitted. Attorneys may visit at any time, but are encouraged to arrange for visits by calling program staff before arrival. Special visiting hours may be arranged outside regular visiting hours. Most visits should be no longer than one hour. Passes Residents may earn the privilege of individual passes once they have successfully completed the CIH orientation phases, and provided that their court order/conditional release/community release plan permits this. Passes are contingent on the resident having shown a level of responsibility and an ability to safely handle such independence. Passes may be independent or with family / significant other. Phone calls Residents are allowed to make and receive telephone calls during unstructured time until 10 p.m. Sunday thru Thursday and until 11 p.m. on Friday and Saturday. Calls should be limited to 15 minutes as a courtesy to peers, who share this phone line. Family and referring agencies may call the group home at any time (24 hours a day) to speak with staff. TREATMENT SERVICES While at the CIH the resident can expect to receive these services: Orientation Level: An Orientation Level is established to allow residents the opportunity to earn freedom as they achieve goals related to independent living skills and show responsible, safe behavior. Psychiatric Services: Psychiatric services will be provided through the provider / community service board that services the CIH catchments area and Mental Health Center. Medications will be prescribed and monitored through this clinic. Case Management: Case management will be provided through the community service board serving the individual or through other community-based agencies. Additional support will be provided by the REGIONAL HOSPITAL Conditional Release Coordinator or designee. Recreational/Leisure Skill Development Recreational activities will be provided daily at the CIH, including games, reading materials, and hobby supplies. Residents are encouraged to pursue their own interests during their free time. Residents are required to assist in planning monthly activities with an emphasis on budgeting, accessing community resources and developing healthy leisure skills. Physical fitness is also encouraged as a part of the recreational program. A House Council comprising of the residents and Resident Care Provider will meet weekly to develop the scheduled activities upon consensus of the Council. As residents achieve higher privilege levels, they may be permitted to go on independent outings that they plan themselves. Basic Living Skills Residents will be given assistance in learning to sew, cook, launder clothes, clean house, iron, answer the telephone, use the phone book, and perform other essential skills needed on a daily basis. Independent Living Skills Residents are required to take care of their own clothes and to prepare their meals (under staff supervision). Groups will be conducted, teaching residents on such topics as budgeting, balancing a checkbook, grocery shopping, accessing health care, etc. When appropriate, residents will be assisted in acquiring higher skills such as learning to apply and interview for a job or to negotiate the public transportation system. Specialty groups Special groups will be conducted to provide information such as assertiveness training, anger management, relationship building, stress management, communication skills, manners, sex education, substance abuse issues, conflict resolution, cultural awareness, nutrition and grooming. Substance abuse services These services will be provided through contracted services in the community and will be tailored to meet individual residents’ needs. A contracted provider will provide group therapy in the home 3 times per week. Residents will also receive individual therapy 3-4 times per month if needed. Community meetings Community meetings are held weekly to teach problem solving skills and to help residents learn to resolve conflicts with one another. Residents learn to negotiate chores, schedules, rules and other issues related to living in a community. Schedule The weekday and weekend schedules at CIH will be appended to this document and posted at the facility. This schedule changes to meet the needs of the residents served. Transportation Each CIH will have a vehicle on site to attend specific events in the community and to go shopping. Resident Care Provider will transport residents to and from their daytime activities as needed. Some residents will access transportation through a medical reimbursed transportation services or public transportation such as Marta. DISCIPLINE AND GRIEVANCE POLICY Rules and consequences are described specifically in the program manual. The following is a list of principles and guidelines the Community Integration Home adheres to: 1. The client’s intelligence, clinical condition and individual rights shall be considered in determining consequences for inappropriate behavior. 2. The use of consistent praise to reinforce appropriate behavior and encouragement of strengths will be routine. 3. Logical consequences will be imposed, related to inappropriate behavior, and will be carried out in a calm manner. 4. Rules will be clear, definable, and enforceable. Each resident will receive a Rule Book on admission. 5. Physical restraint will be used only when critically necessary in an emergency situation to protect a resident from imminent physical injury to himself or others. 6. Seclusion or placement of a resident in a locked room will not be used. 7. Meals and water will not be denied. 8. Denial of sleep is prohibited. 9. Denial of shelter, clothing or essential personal needs is prohibited. 10. Denial of essential program services is prohibited. 11. Verbal abuse or eliciting fear is prohibited. 12. Physical and corporate punishment is not permitted. 13. Assignment of excessive or unreasonable work tasks that are unrelated to the resident’s inappropriate behavior is prohibited. 14. Denial of communication and/or visits is prohibited. 15. Chemical or mechanical restraints are prohibited 16. Resident shall not be permitted to discipline other residents except as part of an organized therapeutic self-governing program that is conducted in accordance with written policy and supervised directly by designated staff. If a resident feels that he has been mistreated or his rights have been violated, he may make a verbal complaint to the CIH Team Leader or the REGIONAL HOSPITAL Patient Rights office. Health Services A. Medical treatment Residents are required to have a physical examination prior to admission and annually while at the CIH. Those providers who followed the client prior to discharge from REGIONAL HOSPITAL, such as Grady Hospital, public or private medical facility or residents’ personal, credited, medical care provider will provide routine medical care. B. Dental treatment Dental treatment will be provided as needed by providers in the community. Semi-annual check-ups and cleaning are recommended for all residents. C. Medical emergencies In the event of a medical emergency the resident will be transported to the appropriate Emergency Room. When possible, staff will transport the patient; however, if necessary 911 will be called and transportation will be conducted via ambulance. D. Psychiatric treatment Residents will be treated by psychiatrist and facilities as designated in their conditional / community release plan. Schedule of Fees A. Monthly room and board Clients will be assessed monthly room and board. Monthly room and board may be assessed on a sliding scale, so that clients who earn less may pay somewhat less. B. Therapeutic services Clients may be responsible for a co-payment in securing medical and psychiatric services from the county in which they reside. Some clients may be eligible for payment of medical services through Medicare or Medicaid. Discharge Planning In many cases, the Community Integration Home will act as a “stepping stone” toward a less restrictive and more autonomous living arrangement. Decisions regarding discharge will be made jointly between the CIH treatment team and the REGIONAL HOSPITAL Conditional release team or designee. Such moves always must be effected in the context of a valid court order supporting the move. If the CIH team feels that a client is nearing readiness for transition to a less restrictive placement, a representative of this team will notify the Conditional Release Coordinator or designee in order for a dialogue to begin between the hospital and the group home regarding alternate living situations. Working together, and with the client in question, these teams will determine what future placement appears most beneficial for the resident. If necessary, the hospital’s conditional release team or designee will approach the court for a new order approving the placement. Attachments: Weekday and Weekend schedules