induced sputum from bench to bedside
advertisement

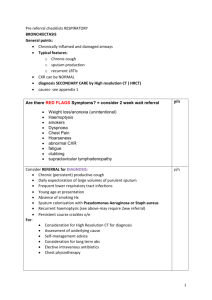
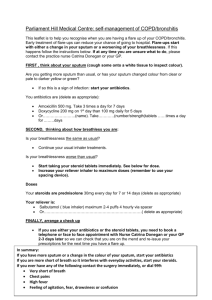
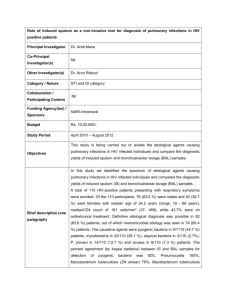
Published in : Current medicinal chemistry (2011), vol. 18, pp. 1415-1422. Status : Postprint (Author’s version) Induced Sputum in Asthma: From Bench to Bedside P. Bakakos1, F. Schleich2, M. Alchanatis1 and R. Louis2 1 st 1 Respiratory Medicine Department, University of Athens, Medical School, Athens, Greece 2 Department of Pneumology CHU Liège, GIGA I3 research group, University of Liège, Belgium Abstract During recent years there has been a growing interest in using non-invasive biomarkers to understand and monitor the airway inflammation in subjects with respiratory tract disorders and mainly asthma and chronic obstructive pulmonary disease (COPD). Sputum induction is generally a well-tolerated and safe procedure and a European Respiratory Society Task Force has published a comprehensive review on sputum methodology. Induced sputum cell count and, to a lesser extent, mediator measurements have been particularly well validated. In asthma, the sputum and the cell culture supernatant can be used for the measurement of a variety of soluble mediators, including eosinophil-derived proteins, nitric oxide (NO) derivatives, cytokines and remodellingassociated proteins. Sputum eosinophilia (> 3%) is a classic feature of asthma although half of the patients seems to be non eosinophilic. Measuring the percentage of sputum eosinophils has proved to be useful in the clinical arena in helping to predict short term response to inhaled corticosteroids (ICS) and tailor the dose of ICS in the severe patients but there is scope for the application of other induced sputum markers potentially useful in clinical practice. The widespread application of induced sputum in asthma across the spectrum of disease severity has given insight into the relationship between airway function and airway inflammation, proposed new disease phenotypes and defined which of these phenotypes respond to current therapy, and perhaps most importantly provided an additional tool to guide the clinical management of asthmatic patients. To date sputum induction is the only non-invasive measure of airway inflammation that has a clearly proven role in asthma management. Keywords : Induced sputum ; asthma ; biomarkers ; clinical applications. INTRODUCTION During recent years there has been a growing interest in using non-invasive biomarkers to understand and monitor the airway inflammation in subjects with respiratory tract disorders. Currently available data seem to underline the robustness of induced sputum as a method for assessing airway inflammation in diseases such as asthma and chronic obstructive pulmonary disease (COPD). Induced sputum samples the central airways and its cellular components (e.g. eosinophils and neutrophils), protein components (e.g. mucins and cytokines) and microbiological components (e.g. viruses and bacteria) can be used as markers of disease severity, exacerbation or progression [1]. Induced sputum cell count and, to a lesser extent, mediator measurements have been particularly well validated [2]. Normal ranges for sputum cell counts from a relatively large adult population have been published [3-5]. Sputum induction is generally a well-tolerated and safe procedure even in patients with severe obstructive airway diseases assessed either in stable condition or during an exacerbation. However, some differences in methodology still exist between various research groups. An important question, therefore, is whether those differences in methodology influence the validity and reliability of induced sputum in the assessment of airway inflammation. The widespread application of induced sputum in asthma, and across the spectrum of disease severity has given an insight into the relationship between airway function and airway inflammation, proposed new disease phenotypes and defined which of these phenotypes respond to current therapy, and perhaps most importantly provided an additional tool to guide the clinical management of asthmatic patients [6]. Published in : Current medicinal chemistry (2011), vol. 18, pp. 1415-1422. Status : Postprint (Author’s version) The aim is to identify through non-invasive or minimally invasive methods of assessment of airway inflammation the future risk of poor asthma control or exacerbations. Although induced sputum eosinophils and exhaled nitric oxide are the most widely investigated candidates for use in the clinical arena, there is scope for a great deal of improvement in their application and other biomarkers may prove to be useful or even better [7]. METHODOLOGY Since the first description of a standardised method to induce and process sputum in asthma in 1992 by Pin et al. [8], there has been an impressive increase in the number of papers in which researchers have used induced sputum to study various aspects of airways inflammation. Thus, in response to the interest in sputum analysis, a European Respiratory Society Task Force has published a comprehensive review on sputum methodology [912]. Sputum Induction and Collection Induced sputum is usually collected in the morning. Induction is performed using an ultrasonic nebuliser. Two different approaches for induction have been used: a) inhalation of the same (3-4.5%) or increasing (3, 4 and 5%) concentrations of aerosolized hypertonic saline over fixed time periods [8, 13] b) inhalation of the same concentration of hypertonic saline (4.5%) over increasing time periods [14]. The choice of technique does not seem to influence the differential sputum cell count. The duration of sputum induction has to be kept standard as it may influence the sputum cell composition. It generally ranges from 10-20 min. A sputum cell count resulting from an induction of 5 min can definitely not be compared with that of an induction of 20 min. The early sample contains more granulocytes while the proportion of mononuclear cells increases with the duration of the induction [15]. Irrespective of the induction technique used, the challenge procedure should be performed in a standardized way that includes the necessary safety procedures, as hypertonic saline can cause severe airway constriction in asthmatic subjects. Subjects should be pre-treated with inhaled short-acting β2-agonists. It has been shown that obtaining sputum from the same asthmatic subjects with or without pretreatment with salbutamol, does not influence the cellular composition [16]. It is also recommended to use isotonic instead of hypertonic saline when post bronchodilator FEV1 is < 65% predicted [17]. Using either hypertonic or isotonic saline does not change the cellular or the biochemical readouts [18,19]. The ERS Task Force conclusions regarding the safety of sputum induction could serve as guidelines, particularly for those who are inexperienced in performing sputum induction procedures [9]. Adding salbutamol into the cup of the nebuliser during the sputum induction has been shown to improve bronchoprotection in moderate to severe asthmatics [20]. Sputum Processing and Analysis Once a sputum sample has been obtained, it should be processed within 2 hours in order to ensure optimum cell counting and staining. However, placing the sample in the refrigerator at 4°C enables to delay the processing up to 9 hours after the collection without altering the cellular and some biochemical (ECP,IL-8) readouts [21]. Sputum processing and cellular analysis can be further delayed until 72 hours when the sample is fixed in dithiothreitol-formaldehyde mixture before dispersal with trypsin [22]. Basically, two techniques for processing have been described. The first approach, which effectively minimizes contamination with saliva, consists of selecting all viscid or denser portions from the expectorated sample [8,23]. The second approach involves the whole expectorate, comprising sputum plus saliva [13]. An adaptation of this method consists of trying to collect sputum and saliva separately, so as to reduce the salivary contamination of induced sputum. Whatever technique is used, the sample is put into preweighed polystyrene tube and weighed. Complete homogenisation can be achieved by the addition of equal volume a dithiothreitol (DTT) solution to the whole sample or 4 x the volume of a selected plug. Dithiothreitol breaks the disulphide bonds in mucin molecules, allowing cells to be released [24]. This is important because cells that are incompletely released from mucus tend to stain darkly, making correct identification difficult. DTT (0.1%) or its equivalent DTE (dithio-erythritol), commonly known as 10% sputalysin solution, has been shown to be more effective at dispersing cells than phosphate-buffered saline (PBS) [25]. Published in : Current medicinal chemistry (2011), vol. 18, pp. 1415-1422. Status : Postprint (Author’s version) The sample is aspirated and dispensed several times with disposable pipette and then agitated on vortex mixer for about 30 seconds. The duration of homogenisation varies between 10-30 minutes (usually 15 minutes). Homogenisation is feasible by using either a shaking water bath at 37 °C (and removing the sample periodically for brief aspiration) or a tube rocker at 22 °C [14,26]. The sample filtration is strongly recommended. Filtration through a 48-mm nylon mesh is commonly used to remove mucus and debris. A single filtration step results in a slight reduction in the total cell count (TCC). However, slide quality is improved and the differential cell count (DCC) remains unchanged. The TCC is performed manually using a haemocytometer. The cell viability is determined by the trypan blue exclusion method [13,23]. Some investigators perform the TCC before centrifugation and others after centrifugation. Because centrifugation by itself causes a reduction in total cell count, it is recommended to perform TCC before centrifugation in order to facilitate standardisation of this measurement and to allow meaningful comparisons of counts between centres and studies. In order to separate sputum cells from the fluid phase, the sample must be centrifuged at 300-1,500Xg. The duration of centrifugation is about 5-10 min. This appears adequate for the purpose of separating cells from the supernatant [13,23,25]. The supernatant can then be stored at -70°C. The next step is the cytospin preparation. The cell concentration is adjusted to 1.0X106 cells.mL-1. Then, 40-65 µL of the sample (or 400-650X103 cells) is added to each cytospin. Cytocentrifugation speeds range from 1051Xg with the most common condition being 22 Xg for 6 min [23]. There is always a risk of losing lymphocytes at lower speeds [27,28]. Cytospin staining for DCCs can be achieved using Giemsa stain. The DCC is determined by counting a minimum of 400 non-squamous cells and is reported as the relative numbers of macrophages, neutrophils, lymphocytes, eosinophils, and bronchial epithelial cells, expressed as a percentage of total nonsquamous cells. The percentage of squamous cells should always be reported separately. SPUTUM AND CELL CULTURE SUPERNATANT ANALYSIS The sputum supernatant can be used for the measurement of a variety of soluble mediators (Table 1), including eosinophil-derived proteins, tryptase, myeloperoxidase, deoxyribonucleic acid (DNA), albumin, fibrinogen, nitric oxide (NO) derivatives and cytokines, such as interleukin (IL)-5, IL-8 and tumour necrosis factor- α (TNFα) [13,29-36]. However, it has to be born in mind that dithiothreitol (DTT) causes reduction of disulfide bonds and denaturation of proteins and thus can affect the expression of cellular markers [37] or measurements of soluble mediators in sputum. After incubation of the standard solution with DTT there was loss of detectable protein mediators on immunoassay. The technique of optimized dialysis and protease inhibition of sputum DTT supernatants aids the detection of chemokines and cytokines. Thus, significantly elevated levels of IL-4, IL-5, IL-13, TNF-α, IL-6, granulocyte-macrophage colony-stimulating factor, and IL-12 were detected in sputum from subjects with severe asthma, after optimized dialysis [38]. Among severe asthmatics those with frequent exacerbations were characterized by higher levels of IL-5 and GM-CSF as compared to those with persistent airway obstruction [39]. Asthma is commonly characterised by eosinophilic airway inflammation. Several groups have reported increased levels of eosinophil cationic protein (ECP) in sputum from asthmatics when compared to healthy controls [2,13,14]. Likewise tryptase levels as a marker of mast cell activation and those of albumin as a marker of plasma exudation were found to be raised in sputum supernatant from asthmatics [35]. Cysteinyl-leukotrienes have been detected in sputum supernatants and montelukast (a leukotriene antagonist) inhibited the eosinophilic chemotactic activity in both corticosteroid-naïve and corticosteroid-treated asthmatics. Accordingly, it was suggested that cysteinyl-leukotrienes actively participate in sputum eosinophil chemotactic activity found in asthmatics irrespective of whether they are or not under treatment with inhaled corticosteroids [40]. A study, including 48 consecutive stable mild to moderate asthmatics, compared cytokine production from sputum cells in eosinophilic versus non-eosinophilic asthma. Sputum cells from asthmatics exhibiting eosinophilic airway inflammation released more IL-4 and less TNF-alpha than those of healthy subjects. By contrast, non-eosinophilic asthmatics did not distinguish from healthy subjects by abnormal cytokine release from their sputum cells [41]. Furthermore sputum cells from moderate to severe asthmatics treated with inhaled corticosteroids release less IL-6 than those of healthy subjects which could contribute to a local impaired innate immunity [42]. Published in : Current medicinal chemistry (2011), vol. 18, pp. 1415-1422. Status : Postprint (Author’s version) Table 1. Soluble Markers in Sputum Supernatant from Patients with Asthma Cytokines ↑ Tumour necrosis factor-α (TNF-α) [31,34,38] ↓ Tumour necrosis factor-α (TNF-α) (in cell culture supernatant) [41] ↑ Interleukm-4 (IL-4) [38] ↑ Interleukin-4 (IL-4) (in cell culture supernatant) [41] ↑ Interleukm-5 (IL-5) [30,34,38,39,54,71] ↑ Interleukm-6 (IL-6) [38,80] ↑ Interleukm-8 (IL-8) [14,39,61,71,80] ↑ Interleukm-12 (IL-12) [38] ↑ Interleukm-13 (IL-13) [38,54] ↑ Granulocyte/macrophage colony-stimulating factor (GM-CSF) [38,39] Mast cell-derived mediators ↑ Histamme [93] ↑ Tryptase [35,59,80] Eosinophil-derived mediators ↑ Eosinophil cationic protein (ECP) [2,13,30,33,35,36,39,59,61,64,68,71,81,82,85,93,97] ↑ Eosinophil-derived neurotoxin (EDN) [2] ↑ Eosinophil peroxidase (EPO) [33] Neutrophil-derived mediators ↑ Myeloperoxidase (MPO) [33,59,61,71] ↑ Neutrophil elastase [80,82] ↑ Human neutrophil lipocalin (HNL) [33] Remodelling-associated proteins Matrix metalloproteinases (MMPs) ↑ MMP-2 [46,47] ↑ MMP-9 [47,48,49] Tissue inhibitors of metalloproteinases (TIMPs) ↑ TIMP-1 [47,48] ~ TIMP-2 [47] ↑ Procollagen type I C-termrnal peptide (PICP) [50] ~ Collagen type I C-termrnal telopeptide (ICTP) [50] ↑ Vascular endothelial growth factor (VEGF) [51] ↑ Transforming growth factor beta 1 (TGF-β1) [52] Others ↑ Fibrmogen [2,30] ↑ Albumin [2,13,59] ↑ Mucin-like glycoprotein [88] ↑ Deoxyribonucleic acid (DNA) [32] ↑ Nitric oxide (NO) derivatives [36] ↑ Intercellular adhesion molecule-1 (ICAM-1) [35] ↑ 8-iso-PGF(2alpha) [43] ↑ = increased levels, ↓ = decreased levels, ~ = at normal range Induced sputum 8-iso-PGF(2alpha) concentrations were found to be elevated in subjects with stable asthma versus control subjects and also increased as clinical asthma pattern worsened. Moreover, sputum 8-isoPGF(2alpha) concentrations were elevated during acute asthma and decreased with recovery [43]. Patients with asthma show lower induced sputum pH than healthy subjects and those with uncontrolled asthma lower than those with controlled asthma. The pH in induced sputum may reflect a different aspect of asthma from sputum eosinophils and be related to different pathophysiologic factors [44]. Patients with refractory asthma have more nitrative stress in their airways compared with patients with well-controlled asthma as shown by enhanced xanthine oxidase activities and 3-nitrotyrosine in sputum from the refractory asthma group compared with the well-controlled group [45]. Another fundamental feature of asthma is airway remodelling. Soluble remodelling-associated proteins, such as procollagen synthesis peptides, matrix metalloproteinases (MMPs), tissue inhibitors of metalloproteinases (TIMPs) and cytokines, can also be detected in the sputum supernatants. Furthermore, induced sputum samples can be obtained before and after specific allergen challenge and/or therapeutic trial. Matrix degradation enzymes Published in : Current medicinal chemistry (2011), vol. 18, pp. 1415-1422. Status : Postprint (Author’s version) and inhibitors have been measured in the induced sputum, such as MMP-2, MMP-9, TIMP-1, TIMP-2, elastase and a1-antitrypsin [46-49]. MMP-9 in induced sputum is elevated in severe asthmatics, after allergen challenge and is not affected by ICS treatment [49]. An imbalance in the MMP-9/TIMP-1 ratio may lead to excessive degradation of extracellular matrix (ECM) proteins that participate in the injury-repair process. The turnover of collagen I can also be indirectly detected in sputum supernatant through the quantification of procollagen type I C-terminal peptide (PICP) and collagen type I C-terminal telopeptide (ICTP). PICP represents synthesis of collagen while ICTP reflects collagen degradation. It has been previously reported that sputum PICP level is increased during asthma exacerbations and is correlated with sputum eosinophils [50]. Angiogenic factor, vascular endothelial growth factor (VEGF) and anti-angiogenic endostatin were measured in the sputum supernatants of asthmatics. VEGF was found to be elevated in asthmatic sputum suggesting angiogenesis [51]. TGF-betal is also involved in the pathogenesis of airway remodeling. In a recent study including 27 patients with moderate-to-severe, but stable asthma, levels of TGF-betal in induced sputum were elevated despite treatment with inhaled corticosteroids and were associated with airflow obstruction and airway wall thickening [52]. The release of GM-CSF, RANTES and IL-8 from induced sputum cells, cultured with beclomethasone dipropionate (BDP), salbutamol and formoterol either alone or in combination was significantly reduced by BDP plus salbutamol or formoterol as compared with either drug alone in 20 mild to moderate asthmatic patients. This study demonstrated a complementary mode of action between BDP and salbutamol or formoterol leading to an enhanced anti-inflammatory activity [53]. IL-13 has been detected in sputum supernatant and has been inversely correlated with the provocative concentration of methacholine causing a 20% fall in FEV1 in asthmatic patients, indicating a relationship between IL-13 and airway hyperresponsiveness (AHR) [54]. When biomarkers obtained from induced sputum were compared with those from other non-invasive methods, such as exhaled breath condensate (EBC), total protein and surfactant protein A (SPA) EBC levels were at least 100-fold lower than those measured in induced sputum [55]. This indicates that the detection of inflammatory mediators through different non-invasive methods is quite variable. CELL COUNTS The cell fraction of induced sputum clearly differs between healthy subjects and asthmatics [8,13,31,56-58]. Asthma is commonly associated with sputum eosinophilia. Overall, compared to healthy subjects, sputum from asthmatics contains increased numbers of eosinophils. The normal value for eosinophils in healthy nonsmokers has been reported as 0.4% with a 90th percentile of up to 1.1%. It is accepted that a sputum eosinophil ≥ 3% has to be considered as abnormal. The range of eosinophil counts in asthma is wide going from 0 up to 90 % [59]. Up to 70% of corticosteroid-naive subjects [60] and 40- 50% of corticosteroid-treated subjects [61,62] with currently symptomatic asthma have a sputum eosinophil count that is outside the normal range. There is at best a weak relationship between the severity of asthma as defined by lung function, airway responsiveness or symptoms and sputum eosinophil count [59,62-64]. In a cross sectional study performed in daily practice, uncontrolled asthma was shown to be associated with raised sputum eosinophilia with approximately 60 % of uncontrolled asthmatics having sputum eosinophil count ≥ 3% irrespective of their maintenance treatment [65]. High sputum eosinophil count, however, is not always associated with poor asthma control. Using a cluster analysis on a large population of asthmatics encountered in both primary and secondary care, Haldar et al. found a peculiar asthma phenotype characterized by intense eosinophilic airway inflammation but relatively poor symptomatic expression [66]. Occupational asthma is associated with similar sputum characteristics to non occupational asthma, and occupational challenges are associated with an increase in sputum eosinophilia [67,68] in much the same way as allergen challenge is. Although sputum eosinophilia is a typical feature of asthma, the increasing application of this technique has led to the recognition that inflammation in asthma is more heterogeneous than previously believed with identification of non eosinophilic asthma. A cut-off point of 3% sputum eosinophils has been suggested to distinguish eosinophilic from non-eosinophilic airway inflammation in asthma [69]. Non eosinophilic asthma is common, accounting for 25 to 55% of corticosteroid-naive asthmatics [61,62,70]. Part of, but not all, these patients are characterised by neutrophilic asthma. In contrast to eosinophil count, the sputum neutrophil cell count in healthy subjects is highly variable, usually averaging 30-35%. Consequently, what has to be considered as an abnormally high sputum neutrophil count is actually a count which is certainly above 60%. In a large population of asthmatics seen in clinical practice the proportion of neutrophilic asthma defined as a sputum neutrophil count greater than 60-65% was close to 20% [62]. Some studies [59,71], but not all [72], pointed out to a raised sputum neutrophilia in severe asthmatics. Both the percentage and the absolute sputum neutrophil Published in : Current medicinal chemistry (2011), vol. 18, pp. 1415-1422. Status : Postprint (Author’s version) counts have been associated with low postbronchodilator FEV1 which lends support to the hypothesis that neutrophilic airway inflammation has a role in the progression of persistent airflow limitation in asthma [73,74]. Based on sputum eosinophil and neutrophil proportions, airway inflammation in asthma could be categorized into four inflammatory subtypes. These subtypes were neutrophilic asthma, eosinophilic asthma, mixed granulocytic asthma and paucigranulocytic asthma. Subjects with increased neutrophils (neutrophilic asthma and mixed granulocytic asthma) were older and had increased total cell count and cell viability compared with other subtypes [75]. It is also likely that some of non eosinophilic asthmatics treated with inhaled corticosteroids have in fact residual eosinophilic inflammation in their airway wall. It seems that having macrophages with large red hued area would predict a relapse of eosinophilic airway inflammation when weaning off [76]. Menopausal asthma, which shares several characteristics of the severe asthma phenotype, has been associated with high sputum neutrophils whereas women with premenopausal asthma presented an essentially eosinophilic inflammatory pattern [77]. Obese people with asthma have poorer asthma control than non obese asthmatics. A retrospective study has found no relationship between BMI and sputum cell counts [78]. A cluster of obese women characterised by high symptom expression without sputum eosinophilia has been described recently, highlighting the possible discordance between symptom expression and airway eosinophilic inflammation [66]. Furthermore, in a recent prospective study, sputum eosinophil and neutrophil counts were found similar in obese and non obese asthma although there was an inverse correlation between sputum eosinophils and waist circumference and a trend for a similar relationship for body mass index (BMI) [79]. Subjects with severe acute asthma may exhibit marked sputum eosinophilia or predominant neutrophilia depending on the triggers that precipitate asthma attack [80]. Massive allergen exposure is associated with raised sputum eosinophil count [81] while viral infections more often result in neutrophilic infiltration [82]. Compared to COPD patients, patients with chronic asthma usually showed higher sputum eosinophil and lower neutrophil percentages [33,83] even though some COPD patients exhibited high sputum eosinophil count [84,85]. Induced sputum has been compared to bronchial wash, bronchoalveolar lavage (BAL) and bronchial biopsies. It has to be realized that these techniques might sample different locations within the bronchial tree, and that it is, therefore, difficult to establish with certainty what the "gold standard" is, to which sputum has to be compared. Comparative studies indicate that sputum contains more neutrophils but fewer macrophages and lymphocytes than BAL fluid [58,86-88]. However, the cellular distribution of sputum, and especially the relative eosinophil numbers, correlates relatively well with the eosinophil numbers in bronchial washes or BAL. INDUCED SPUTUM IN CHILDREN Non-invasive techniques are the ideal, especially in children, given the necessity of safe and repeatable measurements to monitor treatment efficacy and disease progression. Although perhaps less successful than in adults, the technique of induced sputum has been applied in children. The inflammatory response in childhood asthma is characterized by elevated numbers of sputum eosinophils, and eosinophil cationic protein concentration, as well as increased nitric oxide and hydrogen peroxide levels in exhaled breath. Sputum eosinophils correlate with objective markers of disease severity in steroid-naive children with asthma, and in severe asthma [89]. DISCUSSION From bench to bedside - association of induced sputum with diagnosis, response to treatment, level of control and exacerbations. Knowledge of inflammatory phenotype is useful because it relates to treatment response, mechanistic pathways involved in disease pathogenesis and future disease risk. Clinically useful applications of induced sputum analysis have been suggested to be the detection of non-adherence to corticosteroid therapy, assessment of adequacy of inhaled corticosteroid therapy, long-term therapy management in asthma and oral corticosteroid dose adjustment in refractory asthma. It can also be used to study the dose-response effect of inhaled corticosteroids and may be useful to establish the relative potency of different corticosteroid formulations and delivery devices [6]. Published in : Current medicinal chemistry (2011), vol. 18, pp. 1415-1422. Status : Postprint (Author’s version) Induced sputum eosinophil percentage has been shown to be a good aid in the diagnosis of mild to moderate asthma with normal baseline lung function [90]. Under these circumstances sputum eosinophils with a cut-off of 1 % clearly performed better than the variation of peak flow, the extent of bronchodilation after salbutamol or the blood eosinophil count but slightly less than methacholine challenge. In another study using the same type of patients, sputum eosinophils with a cut-off of 3% performed equally to FeNO but once again much better than peak flow variation [91]. However, latest GINA guidelines do not suggest yet the routine use of induced sputum in the diagnostic approach of bronchial asthma, claiming that sputum eosinophilia has not been evaluated prospectively as an aid in asthma diagnosis. An important element in the content validity of induced sputum is the responsiveness to intervention or the capacity of the technique to reflect changes in the degree of airway inflammation. The composition of sputum has indeed been shown to respond to factors known to affect the degree of airway inflammation. Following an allergen inhalation challenge, an increase in the percentage of eosinophils in sputum from atopic asthmatics has been shown [92-96]. Conversely, treatment with systemic or inhaled steroids reduces sputum eosinophil numbers and ECP levels [30,97,98]. The short-term response to inhaled corticosteroids in corticosteroid naive patients differs markedly according to the sputum eosinophil count, with little evidence of improvement in symptoms and airway responsiveness in subjects with a baseline sputum eosinophil count of < 3% [70]. The response to inhaled corticosteroids appears to be particularly poor in patients with high sputum neutrophil count [62]. In contrast, asthmatics with sputum eosinophilia have a favourable response to corticosteroids, even in ex-smokers and current smokers [99]. Sputum eosinophilia was positively correlated with the degree of clinical improvement to inhaled corticosteroids and was more closely related to clinical response than FeNO, sputum or peripheral blood eosinophilic cationic protein [100]. A recent placebo-controlled cross-over trial of inhaled mometasone, 400 µg qd for 8 weeks, in subjects characterized as either having eosinophilic or non eosinophilic asthma prior to study entry has confirmed that a favorable response to corticosteroids was reserved to asthmatics with sputum eosinophilia [101]. These findings suggest that measuring the underlying airway inflammation might provide a better guide regarding the need for corticosteroid treatment than the assessment of functional abnormality. However, long term studies looking at other parameters such as exacerbation rate are urgently required before denying the utility of inhaled corticosteroids in non eosinophilic asthmatics. Categorising subjects according to the presence of sputum eosinophilia might be particularly useful in asthmatics that are symptomatic despite treatment with inhaled corticosteroids since the additional treatment options (long acting beta2-agonists, higher-dose inhaled corticosteroids, leukotriene antagonists and theophylline) differ in their effects on eosinophilic airway inflammation [102-105]. Sputum cell counts may be useful to study the potential anti-inflammatory effects of drugs like theophylline, long-acting betaadrenoceptor agonists, leukotriene antagonists and newer drugs in development. Little et al. found that in patients with asthma, a sputum eosinophil count >4% had a 68% positive predictive value with a sensitivity of 59% and specificity of 76% for an improvement in FEV1 >15% after a 2-week course of oral corticosteroids [106]. In a recent study, high-dose oral corticosteroids reduced sputum eosinophil counts in patients with severe refractory asthma but this effect was observed only in asthmatics with baseline eosinophilia [107]. A recent study conducted in daily practice has shown that uncontrolled asthmatics were associated with raised sputum eosinophilia and raised bronchial hyperresponsiveness to methacholine but not raised FeNO. Approximately 60% of asthmatics with ACQ (Asthma Control Questionnaire) >1.5 exhibit sputum eosinophil count > 3% [65]. Both FeNO and sputum eosinophils were found to be useful for titrating inhaled corticosteroids in asthmatic patients in order to achieve better long-term control of the disease. In a study in which unstable eosinophilic asthmatics were treated by raising the dose of inhaled corticosteroids according to FeNO and induced sputum eosinophil levels, both inflammatory markers decreased over time but with a different kinetic, FeNO decrease being more dramatic than that of sputum eosinophil count after 3 months. The change in FeNO and sputum eosinophil count correlated after 6 months. Concomitant to these changes, a reduction in symptoms and bronchial hyperresponsiveness were observed compared to baseline [108]. Another important part of the natural history of asthma is exacerbations. There is now strong evidence from two independent studies supporting the importance of monitoring airway inflammation by sputum induction to reduce asthma exacerbations. In a randomized placebo-controlled trial, 74 subjects with asthma were assigned to either a management strategy aimed at normalizing their sputum eosinophil count or standard clinical care. Patients in the sputum management group had significantly fewer severe asthma exacerbations than patients in the control group, and significantly fewer patients were admitted to hospital with asthma. The reduction in exacerbations was achieved without an increase in the total corticosteroid dose in the sputum management group. Published in : Current medicinal chemistry (2011), vol. 18, pp. 1415-1422. Status : Postprint (Author’s version) The monitoring of airway inflammation in the sputum management group identified a group of patients with non eosinophilic asthma whose sputum eosinophil counts remained within the normal range and in this group the dose of corticosteroids was reduced without evidence of deterioration [109]. In another 2-year follow-up multicenter, randomized, parallel-group effectiveness study of 117 asthmatics, patients who entered into a treatment directed at normalizing the sputum eosinophil count also showed a reduction in exacerbations and increased the time to first exacerbation by 213 days. This benefit was not at the expense of increased therapy in the intervention group. In this study, the inflammatory phenotype of the exacerbations was characterized and it was in the sputum management group where eosinophilic, but not non eosinophilic exacerbations were reduced. Interestingly, non eosinophilic exacerbations were more common. The reduction in exacerbations was more apparent in those with severe disease [110]. This suggests that it is probably most appropriate to apply this technique to the management of difficult-to-treat or refractory asthma. In another study, including patients with refractory eosinophilic asthma (sputum eosinophils >2% despite inhaled steroid treatment) it was shown that intramuscular administration of triamcinolone almost completely abolished sputum eosinophils. This suggests that persistent sputum eosinophilia despite extensive antiasthma treatment is not a refractory phenomenon but may still be sensitive to high-dose systemic corticosteroids and implies that these patients with severe asthma need additional or alternative anti-inflammatory treatment to combat the eosinophilia and associated poor prognosis [111]. This was confirmed by two recent placebo controlled studies using mepolizumab (anti-IL-5) in refractory eosinophilic asthma, showing a consistent reduction of asthma exacerbations in the mepolizumab group [112,113] together with a corticosteroid sparing effect in one study [112]. A field that attracts attention is the relationship between induced sputum cell counts and other non invasive markers such as FeNO and EBC pH. Although a FeNO level of 42 ppb generally reflects sputum eosinophil count ≥ 3% with a satisfying accuracy, high dose of inhaled corticosteroids, atopy and smoking may alter the FeNO thresholds. Those patients receiving high dose of inhaled corticosteroids (1000 µg fluticasone/day) had a threshold of 27 ppb and those who were current smokers a threshold of 28 ppb while the best threshold in non atopic patients was 30 ppb. Combining these variables together leads to the conclusion that the thresholds predicting significant sputum eosinophilia range from 15 ppb in a smoking non atopic asthmatic receiving high doses of inhaled corticosteroids to 58 ppb in a non smoking atopic asthmatic not treated with high doses of inhaled corticosteroids [114]. In another recent study including patients with severe refractory asthma, FeNO levels > 19 ppb may already predict sputum eosinophilia > 3% while values < 19 ppb suggest a sputum neutrophilia > 40% irrespective of the presence of eosinophils [115]. The inclusion of sputum induction in the management of asthma is cost-effective. Economic analysis shows that the healthcare-related savings as a consequence of the reduction in asthma exacerbations outweighs the cost of sputum induction and processing [109]. Sputum induction requires laboratory support, but all of the equipment is available in a routine pathology laboratory and minimal training is required. Therefore, sputum induction should be available as a routine test in specialist centers to evaluate and manage patients with severe or difficult-to-treat asthma, as its value seems to be greater in those with severe asthma. To date sputum induction is the only non-invasive measure of airway inflammation that has a proven role in the management of moderate-to-severe asthma. Regular monitoring of airway inflammation in this disease group may be required for optimal treatment and in particular in those patients with discordance between airway inflammation and symptom expression. ABBREVIATIONS ACQ AHR BAL BDP COPD DCC DNA DTT DTE EBC ECP FeNO FEV1 GINA = = = = = = = = = = = = = = Asthma Control Questionnaire Airway hyperresponsiveness Bronchoalveolar lavage Beclomethasone dipropionate Chronic obstructive pulmonary disease Differential cell count Deoxyribonucleic acid Dithiothreitol Dithioerythritol Exhaled breath condensate Eosinophil cationic protein Fraction Exhaled Nitric Oxide Forced Expiratory Volume in 1 second Global INitiative for Asthma Published in : Current medicinal chemistry (2011), vol. 18, pp. 1415-1422. Status : Postprint (Author’s version) GM-CSF ICS ICTP ILMMPs NO PBS 8-iso-PGF PICP TCC TGF-beta TIMPs TNF-α VEGF = = = = = = = = = = = = = = Granulocyte macrophage - colony stimulating factor Inhaled corticosteroids Collagen type I C-terminal telopeptide InterleukinMatrix metalloproteinases Nitric oxide Phosphate buffered saline 8-iso-prostaglandin F Procollagen type I C-terminal peptide Total cell count Tumor growth factor- beta Tissue inhibitors of metalloproteinases Tumor necrosis factor alpha Vascular endothelial growth factor REFERENCES [1] Nicholas, B.; Djukanovic, R. Induced sputum: a window to lung pathology. Biochem. Soc. Trans., 2009, 37, 868-72. [2] Pizzichini, E.; Pizzichini, M.M.; Efthimiadis, A.; Evans, S.; Morris, M.M.; Squillace, D.; Gleich, G.J.; Dolovich, J. Hargreave, F.E. Indices of airway inflammation in induced sputum: reproducibility and validity of cell and fluid-phase measurements. Am. J. Respir. Crit. Care Med., 1996, 154, 308-17. [3] Belda, J.; Leigh, R.; Parameswaran, K.; O'Byrne, P.M.; Sears, M.R.; Har- greave, F.E. Induced sputum cell counts in healthy adults. Am. J. Respir. Crit. Care. Med., 2000, 161, 475-8. [4] Spanevello, A.; Confalonieri, M.; Sulotto, E; Romano, E; Balzano, G.; Migliori, G.B.; Bianchi, A.; Michetti, G. Induced sputum cellularity. Reference values and distribution in normal volunteers. Am. J. Respir. Crit. Care. Med., 2000, 162, 1172-4. [5] Thomas, R.A.; Green, R.H.; Brightling, C.E.; Birring, S.S.; Parker, D.; Wardlaw, A.J.; Pavord, I.D. The influence of age on induced sputum differential cell counts in normal subjects. Chest, 2004, 126, 1811-4. [6] Brightling, C.E. Clinical applications of induced sputum. Chest, 2006, 129, 1344-8. [7] Taylor, D.R. Risk assessment in asthma and COPD: a potential role for biomarkers? Thorax, 2009, 64, 261-4. [8] Pin, I; Gibson, P.G.; Kolendowicz, R.; Girgis-Gabardo, A.; Denburg, J.A.; Hargreave, F.E.; Dolovich, J. Use of induced sputum cell counts to investigate airway inflammation in asthma. Thorax, 1992, 47, 25-9. [9] 9s-18s. Pizzichini, E.; Pizzichini, M.M.; Leigh, R.; Djukanovic, R.; Sterk, P.J. Safety of sputum induction. Eur. Respir. J. Suppl., 2002, 37, [10] Efthimiadis, A.; Spanevello, A.; Hamid, Q.; Kelly, M.M.; Linden, M.; Louis, R.; Pizzichini, M.M.; Pizzichini, E.; Ronchi, C.; Van Overvel, F.; Djukanovic, R. Methods of sputum processing for cell counts, immunocytochemistry and in situ hybridisation. Eur. Respir. J. Suppl., 2002, 37, 19s-23s. [11] Djukanovic, R.; Sterk, P.J.; Fahy, J.V.; Hargreave, F.E. Standardised methodology of sputum induction and processing. Eur. Respir. J. Suppl., 2002, 37, 1s-2s. [12] Vignola, A.M.; Rennar, S.I.; Hargreave, F.E.; Fah, J.V.; Bonsignore, M.R.; Djukanovic, R.; Sterk, PL Standardised methodology of sputum induction and processing. Future directions. Eur. Respir. J. Suppl., 2002, 37, 51s-5s. [13] Fahy, J.V.; Liu, L; Wong, H.; Boushey, H.A. Cellular and biochemical analysis of induced sputum from asthmatic and from healthy subjects. Am. Rev. Respir. Dis., 1993, 147, 1126-31. [14] Richter, K.; Holz, O.; Jorres, R.A.; Mucke, M.; Magnussen, H. Sequentially induced sputum in patients with asthma or chronic obstructive pulmonary disease. Eur. Respir. J., 1999, 14, 697-701. [15] Holz, O.; Jorres, R.A.; Koschyk, S.; Speckin, P.; Welker, L.; Magnussen, H. Changes in sputum composition during sputum induction in healthy and asthmatic subjects. Clin. Exp. Allergy, 1998, 28, 284-92. [16] Cianchetti, S.; Bacci, E.; Ruocco, L.; Bartoli, M.L.; Carnevali, S.; Dente, F.L.; Di Franco, A.; Giannini, D.; Scuotri, L.; Vagaggini, B.; Paggiaro, PL. Salbutamol pretreatment does not change eosinophil percentage and eosino-philic cationic protein concentration in hypertonic saline-induced sputum in asthmatic subjects. Clin. Exp. Allergy, 1999, 29, 712-8. Published in : Current medicinal chemistry (2011), vol. 18, pp. 1415-1422. Status : Postprint (Author’s version) [17] ten Brmke, A.; de Lange, C.; Zwmderman, A.H.; Rabe, K.F.; Sterk, PL; Bel, E.H. Sputum induction in severe asthma by a standardized protocol: predictors of excessive bronchoconstriction. Am. J. Respir. Crit. Care. Med., 2001, 164, 749-53. [18] Cianchetti, S.; Bacci, E.; Ruocco, L.; Bartoli, M.L.; Ricci, M.; Pavia, T.; Dente, F.L.; Di Franco, A.; Vagaggini, B.; Paggiaro, PL. Granulocyte markers in hypertonic and isotonic saline-induced sputum of asthmatic subjects. Eur. Respir. J., 2004, 24, 1018-24. [19] Cataldo, D.; Foidart, J.M.; Lau, L.; Bartsch, P,; Djukanovic, R.; Louis, R. Induced sputum: comparison between isotonic and hypertonic saline solution inhalation in patients with asthma. Chest, 2001, 120, 1815-21. [20] Delvaux, M.; Henket, M.; Lau, L.; Kange, P.; Bartsch, P.; Djukanovic, R,; Louis, R. Nebulised salbutamol administered during sputum induction improves bronchoprotection in patients with asthma. Thorax, 2004, 59, 111-5. [21] Efthimiadis, A.; Jayaram, L.; Weston, S.; Carruthers, S.; Hargreave, F.E. Induced sputum: time from expectoration to processing. Eur. Respir. J., 2002, 19, 706-8. [22] Kelly, M.M.; Hargreave, F.E.; Cox, G. A method to preserve sputum for delayed examination. Eur. Respir. J., 2003, 22, 996-1000. [23] Pizzichini, E.; Pizzichini, M.M.; Efthimiadis, A.; Hargreave, F.E.; Dolovich, J. Measurement of inflammatory indices in induced sputum: effects of selection of sputum to minimize salivary contamination. Eur. Respir. J., 1996, 9, 1174-80. [24] Cleland, W.W. Dithiothreitol, a new protective reagent for SH groups. Bio- chemistry, 1964, 3, 480-2. [25] Louis, R.; Shute, J.; Goldring, K.; Perks, B.; Lau, L.C.; Radermecker, M.; Djukanovic, R. The effect of processing on inflammatory markers in induced sputum. Eur. Respir. J., 1999, 13, 660-7. [26] Spanevello, A.; Beghe, B.; Bianchi, A.; Migliori, G.B.; Ambrosetti, M.; Neri, M.; Ind, P.W. Comparison of two methods of processing induced sputum: selected versus entire sputum. Am. J. Respir. Crit. Care. Med., 1998, 157, 665-8. [27] Fleury-Feith, L; Escudier, E.; Pocholle, M.L; Carre, C.; Bernaudin, J.F. The effects of cytocentrifugation on differential cell counts in samples obtained by broncho alveolar lavage. Acta Cytol., 1987, 31, 606-10. [28] Mordelet-Dambrine, M.; Arnoux, A.; Stanislas-Leguern, G.; Sandron, D.; Chretien, J.; Huchon, G. Processing of lung lavage fluid causes variability in bronchoalveolar cell count. Am. Rev. Respir. Dis., 1984, 130, 305-6. [29] in ', V, de Gouw, H.W.; Smits, H.H.; Sont, J.K.; Hiemstra, P.S.; Sterk, PL; Bel, E.H. Repeatability of cellular and soluble markers of inflammation in induced sputum from patients with asthma. Eur. Respir. J., 1996, 9, 2441-7. [30] Pizzichini, M.M.; Pizzichini, E.; Clelland, L.; Efthimiadis, A.; Mahony, L; Dolovich, L; Hargreave, F.E. Sputum in severe exacerbations of asthma: kinetics of inflammatory indices after prednisone treatment. Am. J. Respir. Crit. Care. Med., 1997, 155, 1501-8. [31] Keatmgs, V.M.; Collins, P.D.; Scott, D.M.; Barnes, PL Differences in interleukin-8 and tumor necrosis factor-alpha in induced sputum from patients with chronic obstructive pulmonary disease or asthma. Am. J. Respir. Crit. Care. Med., 1996, 153, 530-4. [32] Fahy, J.V.; Steiger, D.L; Liu, L; Basbaum, C.B.; Finkbeiner, W.E.; Boushey, H.A. Markers of mucus secretion and DNA levels in induced sputum from asthmatic and from healthy subjects. Am. Rev. Respir. Dis., 1993, 147, 1132-7. [33] Keatings, V.M.; Barnes, P.J. Granulocyte activation markers in induced sputum: comparison between chronic obstructive pulmonary disease, asthma, and normal subjects. Am. J. Respir. Crit. Care. Med., 1997, 155, 449-53. [34] Keatings, V.M.; O'Connor, B.J.; Wright, L.G.; Huston, D.P; Corrigan, C.J.; Barnes, PL Late response to allergen is associated with increased concentrations of tumor necrosis factor-alpha and IL-5 in induced sputum. J. Allergy. Clin. Immunol., 1997, 99, 693-8. [35] Louis, R.; Shute, J.; Biagi, S.; Stanciu, L.; Marrelh, F.; Tenor, H.; Hidi, R.; Djukanovic, R. Cell infiltration, ICAM-1 expression, and eosinophil chemotactic activity in asthmatic sputum. Am. J. Respir. Crit. Care Med., 1997, 155, 466-72. [36] Kanazawa, H.; Shoji, S.; Yamada, M.; Fujii, T.; Kawaguchi, T.; Kudoh, S.; Hirata, K.; Yoshikawa, J. Increased levels of nitric oxide derivatives in induced sputum in patients with asthma. J. Allergy. Clin. Immunol., 1997, 99, 624-9. [37] Popov, T.; Gottschalk, R.; Kolendowicz, R.; Dolovich, J.; Powers, P.; Hargreave, F.E. The evaluation of a cell dispersion method of sputum examination. Clin. Exp. Allergy, 1994, 24, 778-83. [38] Erin, E.M.; Jenkins, G.R.; Kon, O.M.; Zacharasiewicz, A.S.; Nicholson, G.C.; Neighbour, H.; Tennant, R.C.; Tan, A.J.; Leaker, B.R.; Bush, A.; Jose, P.J.; Barnes, P.J.; Hansel, T.T. Optimized dialysis and protease inhibition of sputum dithiothreitol supernatants. Am. J. Respir. Crit. Care. Med., 2008, 177, 132-41. [39] Dente, F.L.; Carnevali, S.; Bartoli, M.L.; Cianchetti, S.; Bacci, E.; Di Franco, A.; Vagaggini, B.; Paggiaro, P. Profiles of pro inflammatory cytokines in sputum from different groups of severe asthmatic patients. Ann. Allergy Asthma Immunol., 2006, 97, 312-20. Published in : Current medicinal chemistry (2011), vol. 18, pp. 1415-1422. Status : Postprint (Author’s version) [40] Hemelaers, L.; Henket, M.; Sele, J.; Bureau, F.; Louis, R. Cysteinyl-leukotrienes contribute to sputum eosinophil chemotactic activity in asthmatics. Allergy, 2006, 61, 136-9. [41] Quaedvlieg, V.; Henket, M.; Sele, J.; Louis, R. Cytokine production from sputum cells in eosinophilic versus non-eosinophilic asthmatics. Clin. Exp. Immunol, 2006, 143, 161-6. [42] Manise, M.; Schleich, F.; Gusbin, N.; Godinas, L.; Henket, M.; Antoine, N.; Corhay, J.L.; Louis, R. Cytokine production from sputum cells and blood leukocytes in asthmatics according to disease severity. Allergy, 2010, 65, 889-96. [43] Wood, L.G.; Garg, M.L.; Simpson, J.L.; Mori, T.A.; Croft, K.D.; Wark, P.A.; Gibson, RG. Induced sputum 8-isoprostane concentrations in inflammatory airway diseases. Am. J. Respir. Crit. Care. Med., 2005, 171, 426-30. [44] Kodric, M.; Shah, A.N.; Fabbri, L.M.; Confalonieri, M. An investigation of airway acidification in asthma using induced sputum: a study of feasibility and correlation. Am. J. Respir. Crit Care. Med., 2007, 175, 905-10. [45] 60. Sugiura, H.; Komaki, Y.; Koarai, A.; Ichinose, M. Nitrative stress in refractory asthma. J. Allergy. Clin. Immunol., 2008, 121, 355- [46] Maisi, R; Prikk, K.; Sepper, R.; Pirila, E.; Salo, T.; Hietanen, J.; Sorsa, T. Soluble membrane-type 1 matrix metalloproteinase (MT1-MMP) and gelatinase A (MMP-2) in induced sputum and bronchoalveolar lavage fluid of human bronchial asthma and bronchiectasis. APMIS, 2002, 110, 771-82. [47] Suzuki, R.; Kato, T.; Miyazaki, Y.; Iwata, M.; Noda, Y.; Takagi, K.; Nakashima, N; Torii, K. Matrix metalloproteinases and tissue inhibitors of matrix metalloproteinases in sputum from patients with bronchial asthma. J. Asthma, 2001, 38, 477-84. [48] Vignola, A.M.; Riccobono, L.; Mirabella, A.; Profita, M.; Chanez, P.; Bellia, V.; Mautino, G.; D'accardi, P.; Bousquet, J.; Bonsignore, G. Sputum metalloproteinase-9/tissue inhibitor of metalloproteinase-1 ratio correlates with airflow obstruction in asthma and chronic bronchitis. Am. J. Respir. Crit. CareMed., 1998, 158, 1945-50. [49] Mattos, W.; Lim, S.; Russell, R.; Jatakanon, A.; Chung, K.F.; Barnes, P.J. Matrix metalloproteinase-9 expression in asthma: effect of asthma severity, allergen challenge, and inhaled corticosteroids. Chest, 2002, 122, 1543-52. [50] Nomura, A.; Uchida, Y.; Sakamoto, T.; Ishii, Y; Masuyama, K.; Morishima, Y; Hirano, K.; Sekizawa, K. Increases in collagen type I synthesis in asthma: the role of eosinophils and transforming growth factor-beta. Clin. Exp. Allergy, 2002, 32, 860-5. [51] Asai, K.; Kanazawa, H.; Kamoi, H.; Shiraishi, S.; Hirata, K.; Yoshikawa, J. Increased levels of vascular endothelial growth factor in induced sputum in asthmatic patients. Clin. Exp. Allergy, 2003, 33, 595-9. [52] Yamaguchi, M.; Niimi, A.; Matsumoto, H.; Ueda, T.; Takemura, M.; Matsuoka, H.; Jmnai, M.; Otsuka, K.; Oguma, T.; Takeda, T.; Ito, I; Chm, K.; Mishima, M. Sputum levels of transforming growth factor-beta 1 in asthma: relation to clinical and computed tomography findings. J. Investig. Allergol. Clin. Immunol., 2008, 18, 202-6. [53] Profita, M.; Gagliardo, R.; Di Giorgi, R.; Pompeo, F.; Gjomarkaj, M.; Nicolini, G.; Bousquet, L; Vignola, A.M. Biochemical interaction between effects of beclomethasone dipropionate and salbutamol or formoterol in sputum cells from mild to moderate asthmatics. Allergy, 2005, 60, 323-9. [54] Park, S.W.; Jangm, H.K.; An, M.H.; Mm, J.W.; Jang, A.S.; Lee, J.H.; Park, C.S. Interleukin-13 and interleukin-5 in induced sputum of eosinophilic bronchitis: comparison with asthma. Chest, 2005, 128, 1921-7. [55] Simpson, J.L.; Wood, L.G.; Gibson, P.G. Inflammatory mediators in exhaled breath, induced sputum and saliva. Clin. Exp. Allergy, 2005, 35, 1180-5. [56] Chodosh, S. Examination of sputum cells. N. Engl. J. Med., 1970, 282, 854- 7. [57] Gibson, P.G.; Girgis-Gabardo, A.; Morris, MM.; Mattoh, S.; Kay, J.M.; Dolovich, J.; Denburg, J.; Hargreave, F.E. Cellular characteristics of sputum from patients with asthma and chronic bronchitis. Thorax, 1989, 44, 693-9. [58] Maestrelh, P.; Saetta, M.; Di Stefano, A.; Calcagni, P.G.; Turato, G.; Ruggieri, M.P; Roggeri, A.; Mapp, C.E.; Fabbri, L.M. Comparison of leukocyte counts in sputum, bronchial biopsies, and bronchoalveolar lavage. Am. J. Respir. Crit. Care Med., 1995, 152, 192631. [59] Louis, R.; Lau, L.C.; Bron, A.O.; Roldaan, A.C.; Radermecker, M.; Djukanovic, R. The relationship between airways inflammation and asthma severity. Am. J. Respir. Crit. Care. Med., 2000, 161, 9-16. [60] Louis, R.; Sele, J.; Henket, M.; Cataldo, D.; Bettiol, J.; Seiden, L.; Bartsch, P. Sputum eosinophil count in a large population of patients with mild to moderate steroid-naive asthma: distribution and relationship with methacholine bronchial hyperresponsiveness. Allergy, 2002, 57, 907-12. Published in : Current medicinal chemistry (2011), vol. 18, pp. 1415-1422. Status : Postprint (Author’s version) [61] Gibson, P.G.; Simpson, J.L.; Saltos, N. Heterogeneity of airway inflammation in persistent asthma : evidence of neutrophilic inflammation and increased sputum interleukin-8. Chest, 2001, 119, 1329-36. [62] Green, R.H.; Brightling, C.E.; Woltmann, G.; Parker, D.; Wardlaw, A.J.; Pavord, I.D. Analysis of induced sputum in adults with asthma: identification of subgroup with isolated sputum neutrophilia and poor response to inhaled cortico steroids. Thorax, 2002, 57, 875-9. [63] Iredale, M.J.; Wanklyn, S.A.; Phillips, I.P; Krausz, T.; Ind, P.W. Non- invasive assessment of bronchial inflammation in asthma: no correlation between eosinophilia of induced sputum and bronchial responsiveness to inhaled hypertonic saline. Clin. Exp. Allergy, 1994, 24, 940-5. [64] Ronchi, M.C.; Piragmo, C.; Rosi, E.; Stendardi, L.; Tanmi, A.; Galh, G.; Duranti, R.; Scano, G. Do sputum eosinophils and ECP relate to the severity of asthma? Eur. Respir. J., 1997, 10, 1809-13. [65] Quaedvlieg, V.; Sele, J.; Henket, M.; Louis, R. Association between asthma control and bronchial hyperresponsiveness and airways inflammation: a cross-sectional study in daily practice. Clin. Exp. Allergy, 2009, 39, 1822-9. [66] Haldar, P.; Pavord, I.D.; Shaw, D.E.; Berry, M.A.; Thomas, M.; Brightling, C.E.; Wardlaw, A.J.; Green, R.H. Cluster analysis and clinical asthma phenotypes. Am. J. Respir. Crit. Care. Med., 2008, 178, 218-24. [67] Obata, H.; Dittrick, M.; Chan, H.; Chan-Yeung, M. Sputum eosinophils and exhaled nitric oxide during late asthmatic reaction in patients with western red cedar asthma. Eur. Respir. J., 1999, 13, 489-95. [68] Lemiere, C.; Pizzichini, M.M.; Balkissoon, R.; Clelland, L.; Efthimiadis, A.; O'Shaughnessy, D.; Dolovich, J.; Hargreave, F.E. Diagnosing occupational asthma: use of induced sputum. Eur. Respir. J., 1999, 13, 482-8. [69] Simpson, J.L.; McElduff, P.; Gibson, P.G. Assessment and reproducibility of non-eosinophilic asthma using induced sputum. Respiration, 2010, 79, 147-51. [70] Pavord, I.D.; Brightling, C.E.; Woltmann, G.; Wardlaw, A.J. Non-eosinophilic cortico steroid unresponsive asthma. Lancet, 1999, 353, 2213-4. [71] Jatakanon, A.; Uasuf, C; Maziak, W.; Lim, S.; Chung, K.F.; Barnes, P.J. Neutrophilic inflammation in severe persistent asthma. Am. J. Respir. Crit. Care Med., 1999, 160, 1532-9. [72] Berry, M.; Hargadon, B.; Morgan, A.; Shelley, M.; Richter, J.; Shaw, D.; Green, R.H.; Brightling, C.; Wardlaw, A.J.; Pavord, I.D. Alveolar nitric oxide in adults with asthma: evidence of distal lung inflammation in refractory asthma. Eur. Respir. J., 2005, 25, 986-91. [73] Shaw, D.E.; Berry, M.A.; Hargadon, B.; McKenna, S.; Shelley, M.J.; Green, R.H.; Brightling, C.E.; Wardlaw, A.J.; Pavord, I.D. Association between neutrophilic airway inflammation and airflow limitation in adults with asthma. Chest, 2007, 132, 1871-5. [74] Little, S.A.; Macleod, K.J.; Chalmers, G.W.; Love, J.G.; McSharry, C.; Thomson, N.C. Association of forced expiratory volume with disease duration and sputum neutrophils in chronic asthma. Am. J. Med., 2002, 112, 446-52. [75] Simpson, J.L.; Scott, R.; Boyle, M.J.; Gibson, P.G. Inflammatory subtypes in asthma: assessment and identification using induced sputum. Respirology, 2006, 11, 54-61. [76] Kulkarm, N.S.; Hollins, R; Sutcliffe, A.; Saunders, R.; Shah, S.; Siddiqui, S.; Gupta, S.; Haldar, P.; Green, R.; Pavord, I.; Wardlaw, A.; Brightling, C.E. Eosinophil protein in airway macrophages: a novel biomarker of eosinophilic inflammation in patients with asthma. J. Allergy. Clin. Immunol., 2010, 126, 61-9. [77] Foschmo Barbaro, M.P; Costa, V.R.; Resta, O.; Prato, R.; Spanevello, A.; Palladino, G.P; Martinelli, D.; Carpagnano, G.E. Menopausal asthma: a new biological phenotype? Allergy, 2010, 65, 1306-12 [78] Todd, D.C.; Armstrong, S.; D'Silva, L.; Allen, C.J.; Hargreave, F.E.; Pa- rameswaran, K. Effect of obesity on airway inflammation: a cross-sectional analysis of body mass index and sputum cell counts. Clin. Exp. Allergy, 2007, 37, 1049-54. [79] Lessard, A.; Turcotte, H.; Cormier, Y.; Boulet, L.P. Obesity and asthma: a specific phenotype? Chest, 2008, 134, 317-23. [80] Fahy, J.V.; Kim, K.W.; Liu, J.; Boushey, H.A. Prominent neutrophilic in- flammation in sputum from subjects with asthma exacerbation. J. Allergy. Clin. Immunol., 1995, 95, 843-52. [81] Wark, P.A.; Simpson, J.; Hensley, M.J.; Gibson, P.G. Airway inflammation in thunderstorm asthma. Clin. Exp. Allergy, 2002, 32, 1750-6. [82] Wark, P.A.; Johnston, S.L.; Moric, I; Simpson, J.L.; Hensley, M.J.; Gibson, P.G. Neutrophil degranulation and cell lysis is associated with clinical severity in virus-induced asthma. Eur. Respir. J., 2002, 19, 68-75. [83] Ronchi, M.C.; Piragmo, C.; Rosi, E.; Amendola, M.; Duranti, R.; Scano, G. Role of sputum differential cell count in detecting airway inflammation in patients with chronic bronchial asthma or COPD. Thorax, 1996, 51, 1000-4. Published in : Current medicinal chemistry (2011), vol. 18, pp. 1415-1422. Status : Postprint (Author’s version) [84] Brightling, C.E.; Monteiro, W.; Ward, R.; Parker, D.; Morgan, M.D.; Wardlaw, A.J.; Pavord, I.D. Sputum eosinophilia and shortterm response to prednisolone in chronic obstructive pulmonary disease: a randomised controlled trial. Lancet, 2000, 356, 1480-5. [85] Louis, R.E.; Cataldo, D.; Buckley, M.G.; Sele, J.; Henket, M.; Lau, L.C.; Bartsch, P.; Walls, A.F.; Djukanovic, R. Evidence of mast-cell activation in a subset of patients with eosinophilic chronic obstructive pulmonary disease. Eur. Respir. J., 2002, 20, 325-31. [86] Keatings, V.M.; Evans, D.J.; O'Connor, B.J.; Barnes, P.J. Cellular profiles in asthmatic airways: a comparison of induced sputum, bronchial washings, and bronchoalveolar lavage fluid. Thorax, 1997, 52, 372-4. [87] Grootendorst, D.C.; Sont, J.K.; Willems, L.N.; Klum-Nelemans, J.C.; Van Krieken, J.H.; Veselic-Charvat, M.; Sterk, P.J. Comparison of inflammatory cell counts in asthma: induced sputum vs bronchoalveolar lavage and bronchial biopsies. Clin. Exp. Allergy, 1997, 27, 769-79. [88] Fahy, J.V.; Wong, H.; Liu, J.; Boushey, H.A. Comparison of samples col- lected by sputum induction and bronchoscopy from asthmatic and healthy subjects. Am. J. Respir. Crit. Care. Med., 1995, 152, 53-8. [89] Gibson, P.G.; Henry, R.L.; Thomas, P. Noninvasive assessment of airway inflammation in children: induced sputum, exhaled nitric oxide, and breath condensate. Eur. Respir. J., 2000, 16, 1008-15. [90] Hunter, C.J.; Brightling, C.E.; Woltmann, G.; Wardlaw, A.J.; Pavord, I.D. A comparison of the validity of different diagnostic tests in adults with asthma. Chest, 2002, 121, 1051-7. [91] Smith, A.D.; Cowan, J.O.; Filsell, S.; McLachlan, C.; Monti-Sheehan, G.; Jackson, P.; Taylor, D.R. Diagnosing asthma: comparisons between exhaled nitric oxide measurements and conventional tests. Am. J. Respir. Crit. Care. Med., 2004, 169, 473-8. [92] Pin, I; Freitag, A.P.; O'Byrne, P.M.; Girgis-Gabardo, A.; Watson, R.M.; Dolovich, J.; Denburg, J.A.; Hargreave, F.E. Changes in the cellular profile of induced sputum after allergen-induced asthmatic responses. Am. Rev. Respir. Dis., 1992, 145, 1265-9. [93] Fahy, J.V.; Liu, J.; Wong, H.; Boushey, H.A. Analysis of cellular and biochemical constituents of induced sputum after allergen challenge: a method for studying allergic airway inflammation. J. Allergy Clin. Immunol., 1994, 93, 1031-9. [94] Gauvreau, G.M.; Doctor, J.; Watson, R.M.; Jordana, M.; O'Byrne, P.M. Effects of inhaled budesonide on allergen-induced airway responses and airway inflammation. Am. J. Respir. Crit. Care. Med., 1996, 154, 1267-71. [95] Wong, B.J.; Dolovich, J.; Ramsdale, E.H.; O'Byrne, P.; Gontovmck, L.; Denburg, J.A.; Hargreave, F.E. Formoterol compared with beclomethasone and placebo on allergen-induced asthmatic responses. Am. Rev. Respir. Dis., 1992, 146, 1156-60. [96] Pizzichmi, MM.; Kidney, J.C.; Wong, B.J.; Morris, M.M.; Efthimiadis, A.; Dolovich, J.; Hargreave, F.E. Effect of salmeterol compared with beclomethasone on allergen-induced asthmatic and inflammatory responses. Eur. Respir. J., 1996,9,449-55. [97] Claman, DM.; Boushey, H.A.; Liu, J.; Wong, H.; Fahy, J.V. Analysis of induced sputum to examine the effects of prednisone on airway inflammation in asthmatic subjects. J. Allergy. Clin. Immunol., 1994, 94, 861-9. [98] Gibson, P.G.; Hargreave, F.E.; Girgis-Gabardo, A.; Morris, M.; Denburg, J.A.; Dolovich, J. Chronic cough with eosinophilic bronchitis: examination for variable airflow obstruction and response to corticosteroid. Clin. Exp. Allergy, 1995, 25, 127-32. [99] Bacci, E.; Cianchetti, S.; Bartoli, M.; Dente, F.L.; Di Franco, A.; Vagaggini, B.; Paggiaro, P. Low sputum eosinophils predict the lack of response to beclomethasone in symptomatic asthmatic patients. Chest, 2006, 129, 565-72. [100] Meijer, R.J.; Postma, D.S.; Kauffman, H.F.; Arends, L.R.; Koeter, G.H.; Kerstjens, H.A. Accuracy of eosinophils and eosinophil cationic protein to predict steroid improvement in asthma. Clin. Exp. Allergy, 2002, 32, 1096-103. [101] Berry, M.; Morgan, A.; Shaw, D.E.; Parker, D.; Green, R.; Brightling, C.; Bradding, P.; Wardlaw, A.J.; Pavord, I.D. Pathological features and inhaled cortico steroid response of eosinophilic and non-eosinophilic asthma. Thorax, 2007, 62, 1043-9. [102] Kips, J.C.; O'Connor, B.J.; Inman, M.D.; Svensson, K.; Pauwels, R.A.; O'Byrne, P.M. A long-term study of the antiinflammatory effect of low-dose budesonide plus formoterol versus high-dose budesonide in asthma. Am. J. Respir. Crit. Care Med., 2000, 161, 996-1001. [103] Turner, M.O.; Johnston, P.R.; Pizzichini, E.; Pizzichini, M.M.; Hussack, P.A.; Hargreave, F.E. Anti-inflammatory effects of salmeterol compared with beclomethasone in eosinophilic mild exacerbations of asthma: a randomized, placebo controlled trial. Can. Respir. J., 1998, 5, 261-8. [104] Pizzichmi, E.; Leff, J.A.; Reiss, T.F.; Hendeles, L.; Boulet, L.P; Wei, L.X.; Efthimiadis, A.E.; Zhang, J.; Hargreave, F.E. Montelukast reduces airway eosinophilic inflammation in asthma: a randomized, controlled trial. Eur. Respir. J., 1999, 14, 12-8. [105] Louis, R.; Bettiol, J.; Cataldo, D.; Sele, J.; Henquet, M.; Radermecker, M. Effect of a 4-week treatment with theophylline on sputum eosinophilia and sputum eosinophil chemotactic activity in steroid-naive asthmatics. Clin. Exp. Allergy, 2000, 30, 1151-60. Published in : Current medicinal chemistry (2011), vol. 18, pp. 1415-1422. Status : Postprint (Author’s version) [106] Little, S.A.; Chalmers, G.W.; Macleod, K.J.; McSharry, C.; Thomson, N.C. Non-invasive markers of airway inflammation as predictors of oral steroid responsiveness in asthma. Thorax, 2000, 55, 232-4. [107] Dente, F.L.; Bacci, E.; Bartoli, M.L.; Cianchetti, S.; Costa, F.; Di Franco, A.; Malagrino, L.; Vagaggini, B.; Paggiaro, P. Effects of oral prednisone on sputum eosinophils and cytokines in patients with severe refractory asthma. Ann. Allergy. Asthma. Immunol., 2010, 104, 46470. [108] Malerba, M.; Ragnoli, B.; Radaeli, A.; Tantucci, C. Usefulness of exhaled nitric oxide and sputum eosinophils in the long-term control of eosinophilic asthma. Chest, 2008, 134, 733-9. [109] Green, R.H.; Brightling, C.E.; McKenna, S.; Hargadon, B.; Parker, D.; Bradding, P.; Wardlaw, A.J.; Pavord, I.D. Asthma exacerbations and sputum eosinophil counts: a randomised controlled trial. Lancet, 2002, 360, 1715-21. [110] Jayaram, L.; Pizzichini, M.M.; Cook, R.J.; Boulet, L.P; Lemiere, C.; Pizzichini, E.; Cartier, A.; Hussack, P.; Goldsmith, C.H.; Laviolette, M.; Parameswaran, K.; Hargreave, F.E. Determining asthma treatment by monitoring sputum cell counts: effect on exacerbations. Eur. Respir. J., 2006, 27, 483-94. [111] ten Brinke, A.; Zwinderman, A.H.; Sterk, P.J.; Rabe, K.F.; Bel, E.H. "Refractory" eosinophilic airway inflammation in severe asthma: effect of parenteral cortico steroids. Am. J. Respir. Crit. Care Med., 2004, 170, 601-5. [112] Nair, P.; Pizzichini, M.M.; Kjarsgaard, M.; Inman, M.D.; Efthimiadis, A.; Pizzichini, E.; Hargreave, F.E.; O'Byrne, P.M. Mepolizumab for prednisone-dependent asthma with sputum eosinophilia. N. Engl J. Med, 2009, 360, 985-93. [113] Haldar, P.; Brightling, C.E.; Hargadon, B.; Gupta, S.; Monteiro, W.; Sousa, A.; Marshall, R.P; Bradding, P.; Green, R.H.; Wardlaw, A.J.; Pavord, I.D. Mepolizumab and exacerbations of refractory eosinophilic asthma. N. Engl. J. Med, 2009, 360, 973-84. [114] Schleich, F.N.; Seidel, L.; Sele, J.; Mamse, M.; Quaedvheg, V.; Michils, A.; Louis, R. Exhaled nitric oxide thresholds associated with a sputum eosinophil count >=3% in a cohort of unselected patients with asthma. Thorax, 2010, 65, 1039-44. [115] Tseliou, E.; Bessa, V.; Hillas, G.; Delimpoura, V.; Papadaki, G.; Roussos, C.; Papiris, S.; Bakakos, P.; Loukides, S. Exhaled nitric oxide and exhaled breath condensate pH in severe refractory asthma. Chest, 2010, 138, 107-13.