TB_7-2 - I-Tech
advertisement

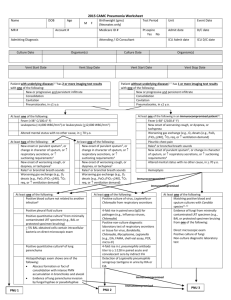
Unit 7 Treatment of TB: B Family Case Botswana National Tuberculosis Programme Manual Training for Medical Officers B Family Background You’ll remember that… • Mrs. B has HIV and starts on IPT • Her husband, Mr. B, presents at the clinic with a cough, and has recently had contact with his uncle who has TB • Though his exam is mostly normal, he gives a spot sputum sample and is told to come back the next day Unit 7: Case Study Slide 2 B Family Case (1) • Mr. B weighs 58kg • After you examine Mr. B and take an initial spot sputum sample, Mr. B returns the next day (day 2) with his morning specimen • You obtain another spot sample and all 3 samples are sent to the lab for acid-fast staining (direct microscopy) • You ask Mr. B to return in 3 days Unit 7: Case Study Slide 3 B Family Case (2) • When he returns (day 5), Mr. B is feeling worse • He reports loss of appetite and seeing blood in his sputum • His results are: • Sputum AFB positive (scanty) x 1 • 2 sputum negative • HIV positive • Mr. B is TB positive • With the new BNTP manual, ONE positive sputum specimen is adequate for the diagnosis of TB (previously, 2 positives were needed) Unit 7: Case Study Slide 4 B Family Case: Question 1 1. How do you manage Mr. B’s case? 2. Does Mr. B qualify for HIV treatment? Unit 7: Case Study Slide 5 B Family Case: Answer 1 (1) 1. Start Category I treatment • FDC • • • 4 tablets (R150/H75/Z400/E275) daily Make sure all patients are weighed at initiation of treatment Single drugs • Isoniazid (INH) 300mg daily, Rifampicin (R) 600mg daily, Pyrazinamide (Z) 2000mg daily, Ethambutol (E) 1200mg daily Unit 7: Case Study Slide 6 B Family Case: Answer 1 (2) • • • • • Educate the patient Provide counselling Start cotrimoxazole, 400/80mg, 2 tabs daily Take blood for CD4 Take baseline bloods: FBC, Chemistry (renal function, electrolytes, LFT) • Refer him to the nearest HIV site 35 km away • Ask him to return for ART assessment and to review results Unit 7: Case Study Slide 7 B Family Case: Answer 1 (3) 2. All HIV positive TB patients qualify for HIV treatment • • Treatment start time is variable Review BNTP manual Unit 7: Case Study Slide 8 B Family Case: Question 2 (1) • • • • 2 weeks later, Mr. B returns to the clinic Haemoglobin is 8.0 CD4 is 300 You provide him with iron supplements and continue to monitor him until completion of TB treatment 6 months later • At completion of treatment, he is considered cured Unit 7: Case Study Slide 9 B Family Case: Question 2 (2) • 5 months after completing TB treatment (month 11), Mr. B. returns to the clinic complaining of cough, difficulty swallowing and pain in his feet • He looks moderately ill • He says he never followed up with the HIV clinic because the hospital is too far for him to travel and he doesn’t have the taxi fare What should you do now for Mr. B? Unit 7: Case Study Slide 10 B Family Case: Answer 2 • Obtain a sputum specimen on the spot and send it for microscopy Unit 7: Case Study Slide 11 B Family Case: Question 3 What other tests should the medical officer order? Unit 7: Case Study Slide 12 B Family Case: Answer 3 • Other tests ordered by the MO • • • • • • 2 more sputum specimens Sputum for culture FBC Repeat CD4 Chemistry : LFTs, creatinine, BUN, electrolytes Chest X-ray • NOTE: ESR is not helpful in diagnosis and is not recommended Unit 7: Case Study Slide 13 B Family Case: Question 4 • CXR shows reticular nodular pattern • Examination shows: • • • • • Wt 52kg T 38.2 RR 26 HR 118 White patches on soft palate Unit 7: Case Study • Cervical lymphadenopathy • Course lung sounds • Enlarged liver Based on these results, what should be the next step of Mr. B’s treatment? Slide 14 B Family Case: Answer 4 • Admit Mr. B • Start him on: • • • • Crystalline penicillin & cotrimoxazole, 4SS tabs Fluconazole, 200mg daily x 14 Paracetamol, 500mg TDS-PRN IV fluids Unit 7: Case Study Slide 15 B Family Case: Question 5 What is Mr. B being presumptively treated for? Unit 7: Case Study Slide 16 B Family Case: Answer 5 • PCN and cotrimoxazole are to treat bacterial pneumonia and as a prevention for PCP • Fluconazole, at 200mg daily x 14, is to treat oesophageal candidiasis • NOTE: It is not appropriate to use fluconazole for oral candidiasis Unit 7: Case Study Slide 17 B Family Case: Question 6 Tests show: • 1 sputum smear positive • 2 sputum smear negative • CD4 50 • ALT 75 • AST 77 • • • • • • Alk Phos 150 Total bili – O/S Hb 7.6 WBC 3.0 Platelets 75 Na 125 How do you manage Mr. B’s case? Unit 7: Case Study Slide 18 B Family Case: Answer 6 (1) • Continue X-PCN x 10 days • For bacterial pneumonia coverage • Change cotrimoxazole dose to 2 tabs daily for prophylaxis • CXR was not indicative of PCP, so cotrimoxazole treatment dosage was stopped Unit 7: Case Study Slide 19 B Family Case: Answer 6 (2) Send a sputum specimen for culture and drug susceptibility testing Start TB treatment immediately • FDC • 4 tablets (R150/H75/Z400/E275) daily + Streptomycin, 1g IM daily • Single drugs • Streptomycin, 1g IM daily, Isoniazid, 300mg daily, Rifampicin, 600mg daily, Pyrazinamide, 2000mg daily, Ethambutol, 1200mg daily Unit 7: Case Study Slide 20 B Family Case: Question 7 (1) Botswana National HIV Programme states: • If CD4 <100, start 1-2 weeks after initiating TB treatment • If CD4 100-200, start 2-3 weeks after initiating TB treatment • If CD4 >200, start treatment after completion of ATT • HAART • AZT/3TC (Combivir) + Efavirenz Unit 7: Case Study Slide 21 B Family Case: Question 7 (2) • • • • Mr. B is discharged after 5 days and is referred to IDCC for HIV management and a local clinic for DOT Mr. B. presents to the IDCC with laboratory results from the hospital the following week He attends a counselling session with DOTS supporter He is started on ART Unit 7: Case Study Slide 22 B Family Case: Question 7 (3) 1. What ART regimen is he started on and when does he begin treatment? 2. What lab test is important in choosing an ART regimen? Unit 7: Case Study Slide 23 B Family Case: Answer 7 1. Combivir + Efavirenz • 2 weeks after initiating ATT 2. Haemaglobin • If Mr. B’s Hb is <7.5, he will be started on d4T instead of AZT (AZT causes bone marrow suppression, which leads to anaemia) Unit 7: Case Study Slide 24