Respiratory Allergies
advertisement

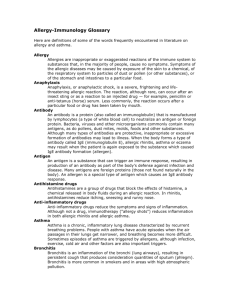
Allergic Rhinitis o Seasonal Aka hay fever Develop mannerisms Nose wrinkling Very itchy Only develop during certain seasons Pollens - most common allergens In the Philippines - season is end of Oct to February Bronchial asthma is peak during these months Molds, fungi - during autumn and winter o Perineal Chronic allergic Have it all thru the year House dust - most common Studies made Considered most allergenic allergen Compose of so many substances Secondary to house dust mite Waste product of the mite (dead cells) In the house, the dead mosquitoes, roaches - their debris becomes the house dust Why very allergenic - dead debris of insects Develop polyps Nasal polyps common with pt's with chronic allergic rhinitis Allergic siners Skin around the eyes (eyebags), have a baggy appearance with dark lines Develop lacrimation from watery renunia o Symptoms Watery renunia Sneezing episodes Usually during the morning After which develop wateria renuria Itchy Mannerisms to get rid of itchiness No fever generally May get secondarily infected Develop If do physical exam, since it's chronic The mucosa is thickened Instead of red/congested, it's pale or gray looking, boggy Example - allergy on the skin, thickening o Diagnosis Perform smear of nasal secretions See lots of eosinophilia o Treatment Use low dose inhaled steroids (steroid sprays) o Differential Diagnosis Infective rhinitis - secondary to infection Viral Bacterial Becomes purulent - have manifestations of fever, malay, etc Vasomotor rhinitis - more of a physical allergy wherein you develop manifestations of rhinitis with changes in the weather In air conditioned room, you go out. Very hot out --develop clogging of the nose Bronchial Asthma o Causes Inhalant allergens and oral ingestants can provoke attack Physical - exercise induced asthma Emotions - laughing o Symptoms Develops bronchospasms Bronchiole edema Hypersecretion o Imagine the lumen of bronchus; in bronchial asthma, there are smooth muscles around bronchus; it will try to constrict it (bronchoconstriction); have edema of the mucosa - it will become edematous; then you'll have secretion; from there you understand why pts develop dyspnea; in asthma, what's more difficult is expiratory phase In inspiration, there's expansion of the chest --expand diameter With expiration, you try to expel CO2 - more difficult Why you retain the gas inside With chronicity --increase in ap diameter --develop barrel chest If you have a tube, and air passes thru it, usually no sound if air goes in freely But if you decrease diameter of the tube, you'll hear a high pitch sound Hence you develop wheezes --- hard to whistle Since there's also secretions, air will not travel freely but will weave in and around the secretions You hear your rhonchi or sonorus and civilant trials o Treatment Give bronchodilator; steroids - anti-inflammatory - to decrease the edema Since secretions, give expectorants All these are symptomatic treatments Just treating the acute attack Not treating/curing bronchial asthma -- there is no cure You just treat the attack Pt will be exposed to allergen again even after the treatment o Desensitization procedure as discussed before But new allergies may develop o Very young and very old patients are affected Children - once over 6 years old, the bronchial asthma attacks stop for a long time; but not gone/not cured; allergic condition is in you -- is in your genes Once you get older -- the attack will return In those who have very strong tendency to allergy Chronic bronchial asthma Attacks every so often Other Allergic Conditions o Anaphylactic shock Usually secondary to something that's given parenterally (IV, sub cutaneous) Some say that it can even occur after an oral dose Esp if pt is very sensitive to allergen But usually parenteral You develop laryngeal edema Difficulty in breathing (asphyxia) Secondary from hypoxia Develop also hypotension Motor collapse Why you develop anaphyl shock Should be the second or nth dose Should be a sensitizing dose Shouldn't be first dose of allergen Don't develop reaction to first Only the 2nd or nth time of exposure Example Nurse in the ICU who is heart disease pt; given penicillin every 28 days; after so many years (6-8 years), he developed anaphylactic shock Rare Usually the 2nd exposure Bp < 60, cold sweats Treatment Give epinephrine (adrenalin) at (1:1000 concentration) 0.2 - 0.5 ml Depends on degree Can give IM, IV, sub cutaneous Other IM is faster; there are more blood vessels in the muscles than the subcutaneous tissues In pts with asthma, the bronchodilator (terbutylin) is given subcutaneously; it will take about 2-3 minutes before you see an effect But in IM, within 1 minute you'll feel effect If already an IV line there already, give it if pt has a pulse If pt in arrest (no pulse), IV ineffective circulation stopped, so what you gave won't circulate Give it every 10-15 minutes depending on degree of the shock If you gave it once, pt reacts, then stop --once is enough If ana shock is secondary to snake bite, still parenteral (bee stings), you can place a tourniquet above the site of the injection of the allergen If it's a snake bite or bee sting, you can inject your adrenaline around the bite (around site of sting) drugs you can give once you gave epinephrine Antihistamines If secretions, give steroids The medical bag always contains syringe and ampere of your adrenaline Atropine and steroids included Serum Sickness o In DeMesa's 26 years of practice, he hasn't seen case of serum sickness o Secondary to an injection of a serum Anti--serum; before, most of your immunoglobs comes from horse serum or pork; serums came from animals before Insulin - now we have human insulin Before only had pork insulin (from pigs) Antitetanus serum (ATS) Very popular Given and there's an incubation Don't develop reaction right away Example Given an injection; you don't have strong allergic tendency to that serum; may develop an urtikaria ---so you take antihistamine That's not serum sickness So test first Incubation period o o o o 7-12 days before you develop allergic illness To those with strong allergic tendency, may develop earlier but still an incubation period Manifestations Rash - urtikaria, morbiliform..etc Fever Body malay Joint pain Edema Organomegaly Self-limiting It will resolve by itself in 2-4 weeks time Why it's difficult to make diagnosis Considered strongly if there's a history of injection of serum GIT/Food Allergy o In most instances, usually not secondary to food itself It's secondary to something added to food Mostly colorings --FND yellow Any dye Colored drinks example - Tang (orange drink), Kool Aid, gatorade Lots of dye added Gatorade is water and electrolytes Not allergic to that but to the additives Fish If smoked fish, determine what they added to it that made you sick o Urtikaria rash, ab cramps, vomiting, diarrhea o Generally, cow's milk allergy Allergic to cow milk proteins Protein enters intestinal mucosa and sensitizes the pts Once sensitized, the second dose of milk --develops reaction -- cramps, rashes, diarrhea Drug Allergy o Differentiated from drug intolerance o Drug sensitization You develop sensitization (allergy) to albutimol, develop urtikarial arrest If you're also sensitive to albutimol, that person may develop diarrhea or purfura simplex The next guy may develop a steron johnson syndrome In drug allergy, you develop manifestations regardless of the drug Individualized One may develop rash, one may develop attack o Drug intolerance You develop an exaggerated pharma effect of drug Example - you're intolerant to salbutimol; even with small dose of salbutimol, you develop tachycardia (palpitation) That's the effect of the drug You're not allergic to drug, but are intolerant to it Some aren't intolerant to the drug, but others are Develop same manifestations with the same drug Both pts will develop the tachycardia if both are intolerant Shifting Exam on Tues Aug 1 o o Exam is true or false and matching 30 questions x 3 = 90 You get 10 points