Student Nurse Workbook
advertisement

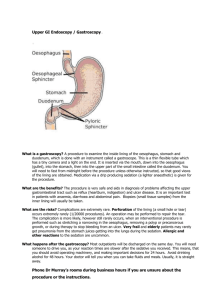
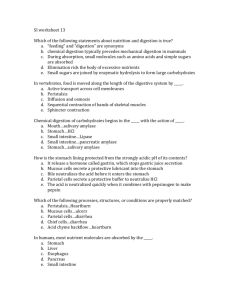
G.I.U Student workbook Nursing levels one, two and three. Amended May 2015 Worksheet one Patient care level one, two and three. 1. What kind of environment might reduce anxiety? 2. Other than analgesia, what methods of pain relief/control could you offer to the patient undergoing colonoscopy? 3. How do staff ensure that the patient’s airway is maintained during gastroscopy? 4. How can we ensure that the patient is correctly identified? 5. How might you ensure the patients privacy and dignity is maintained throughout the whole of their time on GIU? 6. What might you do to ensure the patient has sufficient information given to them before discharge? 7. When preparing for a gastroscopy what questions are asked prior to the throat being sprayed? 8. During endoscopy what should be recorded in the patients care pathway? 10. How can physical injury to a sedated patient on a trolley be prevented? Pathologies Worksheet two, level two and three 1. What disease is commonly found in the colon? 2. What advice can we give regarding this disease? 3. What is a polyp? 4. What is a stemmed polyp called? 5. Name the bacterium, found in the stomach that often causes inflammation and ulcers? 6. If a colonoscopy fails, which two investigations might be offered to the patient? Level one, two and three 7. What does EUS stand for? 8. Why might an EUS be performed? 9. What does EMR stand for? 10. What does PEG stand for? Drugs and conditions Worksheet three, level two and three. 1. What effects do anticoagulants have on the blood? 2. Name three anticoagulants? 3. Prior to endoscopy what is needed to be done if the patient has been taking Warfarin? 4. What does INR stand for? 5. What effect does oral iron medication have on the bowel? 6. How long before colonoscopy should oral iron be discontinued? 7. What is pethidine? 8. What are the common side effects of pethidine? 9. What is Midazolam? 10.What are the common side effects of Midazolam? Patient base readings Worksheet four, level one, two and three. 1. Give two reasons why blood pressure is recorded? 2. If an automatic cuff is not appropriate, what would you do? 3. When should a blood pressure cuff be cleaned? 4. When would you use a disposable cuff? 5. Can you give a reason for using pulse oximetry? 6. Name 3 sites for attaching a pulse oximetry probe? Third year students, level three. Pathologies and Interventions Worksheet five 1. Name two causes of obstruction to the biliary tree? 2. What two procedures may be carried out to gain bile drainage in a patient with common bile duct stones? 3. Name five possible complications of ERCP? 4. What is pancreatitis and its usual cause? 5. What is cholangitis and its usual cause? Workbook produced by S Baines and K Pinder, kind thanks to input from R Robinson, and Kirsty Ryles (student nurse). TERMS RELATIVE TO ENDOSCOPY Achalasia: A rare disease of the muscle of the Oesophagus (swallowing tube). The term achalasia means "failure to relax" and refers to the inability of the lower oesophageal sphincter (a ring of muscle situated between the lower oesophagus and the stomach) to open and let food pass into the stomach. As a result, patients with achalasia have difficulty in swallowing food. Anaemia: The condition of having a lower-than-normal number of red blood cells or quantity of haemoglobin. Anaemia diminishes the capacity of the blood to carry oxygen. Patients with anaemia may feel tired, fatigue easily, appear pale, develop palpitations, and become short of breath. The main causes of anaemia are bleeding. Anaemia is also often due to gastrointestinal bleeding caused by medications, including such common drugs as aspirin and ibuprofen. Anus: The opening of the rectum to the outside of the body. Barium enema: An enema using a white, chalky solution containing barium, in preparation for series of X-ray images of the lower intestine (colon). The barium outlines the colon on the X-ray film. Barrett's oesophagus: A complication of severe chronic GORD (gastrointestinal reflux disease) involving changes in the cells of the tissue that line the bottom of the oesophagus. These oesophageal cells become irritated when the contents of the stomach back up (refluxes) and there is a small but definite increased risk of adenocarcinoma (cancer) of the oesophagus. Biopsy: The removal of a sample of tissue for examination under a microscope to check for cancer cells or other abnormalities. Bowel: The small and large intestine. Caecum: The caecum, the first portion of the large bowel, situated in the lower right quadrant of the abdomen. Colitis: A term used to describe inflammation of the colon. Colon: The long, coiled, tube like organ that removes water from digested food. The remaining material, solid waste called stool, moves through the colon to the rectum and leaves the body through the anus. Also known as the large bowel and large intestine. Colonoscopy: A procedure whereby a physician inserts a viewing tube (colonoscope) into the rectum for the purpose of inspecting the colon. During colonoscopy, polyps can be removed, bleeding can be cauterized, and a biopsy can be performed if abnormal areas of the colon are seen. Diarrohea: A common condition that involves unusually frequent and liquid bowel movements. The opposite of constipation. There are many infectious and non infectious causes of diarrhoea. Persistent diarrhoea is both uncomfortable and dangerous to the health because it can indicate an underlying infection and may mean that the body is not able to absorb some nutrients due to a problem in the bowels. Treatment includes drinking plenty of fluids to prevent dehydration and taking over-the-counter remedies. People with diarrhoea that persists for more than a couple days, particularly small children or elderly people, should seek medical attention. Diverticulitis: Inflammation of the diverticula (small out pouchings) along the wall of the colon, the large intestine. (One out pouching is a diverticulum; two or more are diverticula). Dyspepsia: Indigestion. A condition characterized by upper abdominal symptoms that may include pain or discomfort, bloating, feeling of fullness with very little intake of food , feeling of unusual fullness following meals, nausea, loss of appetite, heartburn, regurgitation of food or acid, and belching. The term dyspepsia is often used for these symptoms when they are not typical of a well-described disease (for example, gastrointestinal reflux) and the cause is not clear. Dysphagia: A condition in which a patient experiences difficulty swallowing food or liquid. This difficulty swallowing can be caused by a blockage, a motility disorder, or injury to the oesophagus. Endoscope: A lighted optical instrument that is used to get a deep look inside the body. An endoscope, which may be rigid or flexible, can be used to examine organs, such as the throat or oesophagus. Specialized endoscopes are named for where they are intended to look. Examples include the cystoscope (bladder), nephroscope (kidney), bronchoscope (bronchi), laryngoscope (larynx), otoscope (ear), arthroscope (joint), laparoscope (abdomen), and gastrointestinal endoscopes. Endoscopy: Examination of the inside of the body by using a lighted, flexible instrument called an endoscope. In general, an endoscope is introduced into the body through a natural opening such as the mouth or anus. Although endoscopy can include examination of other organs, the most common endoscopic procedures evaluate the oesophagus, stomach, and portions of the intestine. Enema: Liquid injected into the rectum. An enema may be used for therapeutic (such as to stimulate evacuation of the bowels or heal inflammation of colon called colitis ) or diagnostic (such as imaging studies of the gastrointestinal tract - barium enema) purposes. Enteroscopy: The use of a flexible instrument (a "scope") to examine the small intestine, a very long hollow tube located between the stomach and colon (large intestine) and made up of the duodenum, jejunum, and ileum. Endoscopic retrograde cholangio-pancreatography: (ERCP) is a diagnostic test to examine the duodenum, the papilla of vater (a small nipple like structure with openings leading to the bile ducts and the pancreatic duct, the bile ducts and the gallbladder and the pancreatic duct. ERCP is used in diagnosing and treating the following conditions: Blockage of the bile duct by gallstones, cancer, strictures (scarring) or compression from adjacent organs or tumours . Jaundice (yellow colouring of the skin) due to obstruction of the bile duct, also causing darkening of the urine and light coloured stools. Persistent or recurrent upper abdominal pain which cannot be diagnosed by other tests. Unexplained loss of appetite and weight. Confirming the diagnosis of cancer of the pancreas or the bile duct, so that surgery or other treatment can be tailored to the disease Endoscopic Ultrasound :(EUS) combines endoscopy and ultrasound in order to obtain images and information about the digestive tract and the surrounding tissue and organs. Faecal: Relating to the faeces, the stool. The excrement discharged from the intestines. Faeces: The excrement discharged from the intestines. Gastric: Having to do with the stomach. Gastritis: Inflammation of the stomach. The Gastroscopy Procedure Gastroscopy: An examination of the upper digestive tract using an endoscope. It is operated by a doctor and enters the body through the mouth. A gastroscopy is performed to investigate a number of symptoms in the upper digestive tract, such as stomach or chest pain, heartburn, nausea and vomiting. Gastro-oesophageal: Pertaining to both the stomach and the oesophagus, as in the gastrooesophageal junction, the place where the oesophagus connects to the stomach. Gastro-oesophageal reflux: The return of stomach contents back up into the oesophagus. This frequently causes heartburn because of irritation of the oesophagus by stomach acid. Gastrointestinal: Adjective referring collectively to the stomach and small and large intestines. Gastrointestinal tract: The stomach and intestines. Abbreviated GI tract. GORD: Gastro-oesophageal reflux disease. GI tract: Short for gastrointestinal tract. See: Gastrointestinal tract. Haematemesis: Is the vomiting of blood. This condition occurs when there is bleeding in the oesophagus, stomach or duodenum, i.e. bleeding proximal to the duodenal-jejunal junction. It is very rare for bleeding entering the gut distal to this point to return to the stomach.The colour and volume of the vomitus is an indicator to how long the blood has been in the stomach. Dark blood or 'coffee grounds' suggests a smaller bleed which has been altered by contact with gastric acid. A large volume of bright red blood is suggestive of a rapid and sizeable haemorrhage. Haemorrhoids: Also known as piles, are swellings that contain enlarged and swollen blood vessels in or around the rectum and anus. Heartburn: An uncomfortable feeling of burning and warmth occurring in waves rising up behind the breastbone (sternum) toward the neck. It is usually due to gastro-oesophageal reflux disease (GORD), the rise of stomach acid back up into the oesophagus. Heartburn has nothing whatsoever to do with the heart. It is a popular nonmedical term. It is medically called pyrosis. Helicobacter pylori: A bacterium that causes stomach inflammation (gastritis) and ulcers in the stomach and duodenum. This bacterium is the most common cause of ulcers worldwide. H. pylori infection may be acquired from contaminated food and water or through person-to-person contact. It is common in people who live in crowded conditions with poor sanitation. This bacterium is also believed to be associated with stomach cancer (gastric adenocarcinoma) and a rare type of lymphoid tumour called gastric MALT lymphoma. Infected persons usually carry H. pylori indefinitely, often without symptoms, unless treated with antibiotics to eradicate the bacterium. Also known as ulcer bug. Hiatus Hernia: Where part of the stomach pushes up into the lower chest through a defect in the diaphragm. A valve that normally stops stomach acid rising into the oesophagus (food pipe) does not work properly in patients with hiatus hernia, and they experience pain as the acid escapes upwards from the stomach. Intestine: The long, tube like organ in the abdomen that completes the process of digestion. It consists of the small and large intestines. Large bowel: Another name for the large intestine. Melaena: Is the passage of black, tarry stools. The stools have a characteristic and offensive smell due to the presence of blood that has been digested by intestinal enzymes and bacteria. The degradation of the blood also accounts for the dark colouration. It usually implies a bleed at some point early in the gastrointestinal system proximal to the splenic flexure of the colon (usually the oesophagus, stomach or duodenum). There must be the loss of more than 60 ml of blood in the upper gastrointestinal tract before melaena occurs. Most commonly, it is caused by acute or chronic peptic ulceration; less commonly, by right-sided colonic bleeding; and rarely, by small bowel bleeding. OGD: Oesophageogastroduodenoscopy. Oesophageal: Related to the oesophagus. Oesophageal cancer: A malignant tumour of the oesophagus. The risk of cancer of the oesophagus is increased by long-term irritation of the oesophagus, such as from smoking, heavy alcohol intake, and Barrett esophagitis. Very small tumours in the oesophagus usually do not cause symptoms. As a tumour grows, the most common symptom is difficulty in swallowing. There may be a feeling of fullness, pressure, or burning as food passes down the oesophagus. Cancer of the oesophagus can also cause indigestion, heartburn, vomiting, and frequent choking on food. Because of these problems, weight loss is common. Oesophageal cancer can be diagnosed through a barium X-ray study of the oesophagus and endoscopy and biopsy of the tumour. Treatment includes chemotherapy and sometimes surgery. Oesophagogastroduodenoscopy: Also known as OGD or upper endoscopy. A procedure that enables the examiner (usually a gastroenterologist) to examine the oesophagus (the swallowing tube), stomach, and duodenum (the first portion of small bowel) using a thin flexible tube (a "scope") that can be looked through or seen on a TV monitor. Percutaneous endoscopic gastrostomy: An endoscopic medical procedure in which a tube (PEG tube) is passed into a patient's stomach through the abdominal wall, most commonly to provide a means of feeding when oral intake is not adequate. Peptic ulcer: An ulcer in the lining of the stomach, duodenum, or oesophagus. Peptic ulcers affect millions of people in the UK yearly. Ulcer formation is related to Helicobacter pylori bacteria in the stomach, use of anti-inflammatory medications, and cigarette smoking. Peptic ulcer pain may not correlate with the presence or severity of ulceration. Complications of peptic ulcers include bleeding, perforation, and blockage of the stomach (gastric obstruction). Diagnosis is made via barium X-ray or endoscopy. Treatment involves use of antibiotics to eradicate H. pylori, elimination of risk factors, and prevention of complications. Polyp: A mass of tissue that develops on the inside wall of a hollow organ, such as the colon. Rectum: The last 6 to 8 inches of the large intestine. The rectum stores solid waste until it leaves the body through the anus. Reflux: The term used when liquid backs up into the oesophagus from the stomach. Sigmoidoscopy: A procedure in which a physician inserts a viewing tube (colonoscope) into the rectum for the purpose of inspecting the lower colon and rectum. If an abnormal area is detected, a biopsy can be performed. Small bowel: Another name for the small intestine. Small intestine: The part of the digestive tract that extends from the stomach to the large intestine. Stomach: The digestive organ that is located in the upper abdomen, under the ribs. The upper part of the stomach connects to the oesophagus, and the lower part leads into the small intestine. When food enters the stomach, muscles in the stomach wall create a rippling motion (peristalsis) that mixes and mashes the food. At the same time, juices made by glands in the lining of the stomach help digest the food. After about 3 hours, the food becomes a liquid and moves into the small intestine, where digestion continues. Terminal Ileum: Is the most distal part of the small intestine. It connects to the cecum, the pouch between the small and the large intestine, via the ileocaecal valve. Tumour: An abnormal mass of tissue. Tumours are a classic sign of inflammation, and can be benign or malignant (cancerous). There are dozens of different types of tumours. Their names usually reflect the kind of tissue they arise in, and may also tell you something about their shape or how they grow. Ulcer: A lesion that is eroding away the skin or mucous membrane. Ulcers can have various causes, depending on their location. Ulcers in the gastrointestinal tract were once attributed to stress, but most are now believed to be due to infection with the bacterium Helicobacter pylori. GI ulcers, however, are often made worse by stress, smoking, and other non-infectious factors. Varices: Result from dilated veins in the walls of the lower part of the oesophagus and sometimes the upper part of the stomach. Bleeding varices are a life-threatening complication of portal hypertension (increased blood pressure in the portal vein caused by liver disease). Increased pressure causes the veins to balloon outward. The vessels may rupture, causing vomiting of blood and bloody stools or tarry black stools. If a large volume of blood is lost, signs of shock will develop. Any cause of chronic liver disease can cause bleeding varices. Information supplied by Carrie Cumbers (RGN)