Proposed Treatment
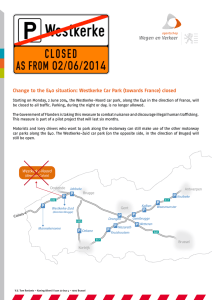
advertisement
Systemic Chlamydia Pneumoniae Infection And Long Term Combination Antibiotic Treatment (A Personal Treatment Plan) After decades of work with Chlamydia pneumoniae (Cpn) at Vanderbilt University, Dr. Charles Stratton has helped establish the theoretical basis, and helped establish various combination antibiotic protocols (CAP), for a variety of illnesses caused by Cpn. Other doctors at Vanderbilt, as well as Dr. David Weldon in the UK, Dr. Michael Powell in Sacramento, and others have been successfully treating a variety of illness with CAP regimens that last for 1-3 years. Multiple antibiotics are needed because Cpn has a complex life-cycle involving 3 distinct forms plus multiple transition paths between forms that require different methods of attack. Multi-year protocols are required because the two intracellular forms are hard to kill and because host cell death ensues when the intracellular forms are killed, releasing significant amounts of toxins as well as risking organ failure if too many host cells are killed at once. Cpn in CFID/FMS/ME/CFS patients is, according to Dr. Stratton, the most challenging to treat as it takes longer, people have more "brisk" reactions to meds, tend to have built up bigger bacterial loads in tissues, and have more pervasive organ involvement of Cpn, in addition to more porphyria, and have been sicker longer. In general, antibiotics are introduced slowly and reactions observed before increasing doses and adding additional antibiotics. Secondary porphyria is a significant complication in many Cpn infections, particularly in liver infections, and tends to worsen as Cpn-infected cells are killed because accumulated intracellular porphyrins are released into the blood stream. Antibiotics that have the most powerful killing effects on intracellular Cpn forms are therefore added in the latter phases of CAP, and are pulsed so that both cell death and porphyrin release are controlled, and so that the body has time to eliminate the porphyrins and replace the cells. Testing for Cpn is problematic, particularly serum antibody testing, which is very unreliable for intracellular infection. Even Cpn DNA/RNA PCR testing is problematic unless it is carefully done by experts. Essentially, reliable commercial versions of proper Cpn DNA/RNA PCR testing are not yet available. Therefore, Cpn diagnosis is frequently based on clinical observation, and observation of empirical treatment results of CAP treatment. Anti-porphyria regimes are critical for those prone to the secondary porphyria reactions. These regimes are based on primary porphyria care, and include: avoidance of alcohol, tobacco, porphyriogenic drugs, and other porphyria triggers, a high-carbohydrate low-tryptophan diet, large amounts of fluids to wash out water-soluble porphyrins, and an agent such as activated charcoal or cholestyramine to absorb lipid-soluble porphyrins to prevent their enterohepatic recirculation. Dr. Stratton has shown that auto-antibodies against the porphyrins can develop and that cross reaction with Vitamin B12 can result in a subclinical autoimmunemediated Vitamin B12 deficiency, and thus high-dose oral or injectable B12 is recommended. Vitamin D deficiency has been associated with several conditions related to Cpn infection, and almost everyone living 30 degrees north or south of the equator are deficient in vitamin D, and a minimum of 1000 units of vitamin D are recommended. Antioxidants at high dosages (preferably taken twice per day) help to mitigate the effects of free radicals produced by porphyrins. Examples of suitable antioxidants include but are not limited to Vitamin C (e.g., 1 gram per dosage; 10 g daily maximum); Vitamin E (e.g., 400 units per dosage; 3000 daily maximum); LCarnitine (e.g., 500 mg per dosage; 3 g daily maximum); coenzyme Q-10 (e.g., 30 mg per dosage; 200 mg daily maximum); biotin (e.g., 5 mg per dosage; 20 mg daily maximum); lipoic acid (e.g., 400 mg per dosage; 1 g daily maximum); selenium (e.g., 100 mg per dosage; 300 ag daily maximum); glutamine (e.g., from 2 to about 4 g per dosage); glucosamine (e.g., from about 750 to about dosage); and chondroitin sulfate (e.g., from about 250 to about 500 mg per dosage). Testing recommended prior to CAP includes: 1. 2. 3. 4. CBC & Differential Liver function tests (AST, ALT) Uric acid Serum iron studies (typically depleted by Cpn: low iron levels are more diagnostic, and are not necessarily indicators to supplement, which may actually increase Cpn infection). 5. RBC ALA Dehydratase & PbG Deaminase (Uroporphyrinogen Synthase) 6. Vitamin B-12 level 7. Homocystein levels 8. Serum methymalonate level 9. Vitamin D levels 10.Thyroid panels (standard plus free T4, free T3, reverse T3) [Endocrine disturbances common in Cpn and associated diseases] 11.Serum creatinine 12.24-hour urine and 24-hour stool specimens for porphyrins Proposed Combination Antibiotic Protocol (CAP) The proposed CAP is based on several published CAPs. Antibiotics are chosen for efficacy against the various stages of Cpn, as well as tolerability, generally low side-effect profile, and low impact on liver. Antibiotics are added one at a time, starting with low does and increasing doses as tolerability effects are established. Powerful RB killers are added last, and are usually pulsed. The following CAP is proposed: Start with NAC 1.5 gm b.i.d (kills the EB stage). Add amoxicillin (another EB killer). Work up to 500 mg b.i.d. Based on tolerability to amoxicillin, start building up to 250 mg M,W,F Zithromax (azithromycin). Azithromycin is primarily bacteriostatic, though apparently kills some RB stage also. Is also immunomodulatory. Based on tolerability to azithromycin, build up to 100 mg b.i.d. Vibramycin (doxycycline hyclate). Doxycycline is primarily bacteriostatic, though apparently kills some RB stage also. Is also immunomodulatory. Both zith and doxy are used in combination to avoid possible antibacterial resistance. Based on tolerability of the above combination, build up to 500 mg b.i.d Flagyl (metronidazole) (5 days on, 2 weeks off). Metronidzole is a potent RB killer, and is pulsed because RB death results in host cell death and the release of intracellular porphyrins. (Alternatively, Tindamax [tinidazole] can be used instead of metronidazole. 500mg b.i.d, pulsed on the same schedule as metronidazole.) Rifadin (rifampin/rifampicin) at the end. This is a very potent RB killer and can be very tough on the liver, is reputedly a porphyriogenic drug, and should generally be used only after Cpn has largely been cleared from the liver and the liver substantially recovered. Antibiotic Prescriptions 500 mg b.i.d. Amoxil (amoxicillin); 500 mg capsules; 60/month; 180/90-days 250 mg Zithromax (azithromycin) (M, W, F); 250 mg capsules; 15/month; 45/90-days 100 mg b.i.d. Vibramycin (doxycycloine hyclate); 100 mg capsules; 60/month; 180/90 days 500 mg b.i.d Flagyl (metronidazole) (5 days on, 2 weeks off); 500 mg tablets; 20/month; 60/90-days or 500 mg b.i.d Tindamax (tinidazole) (5 days on, 2 weeks off); 500 mg tablets; 20/month; 60/90-days Anti-Porphyria Prescriptions 16 gm b.i.d. Cholestyramine; 378gmoral suspension (168 gm cholestyramine) cans; 3 cans/month; 9 cans/90-days 1000 mcg q.d. B-12 Injections; 10 cc vials; 3 vials/month; 9 vials/90-days; 36 vials/year 365 syringes/year; 3cc 1 inch, 22 gauge needles.