Comments
advertisement

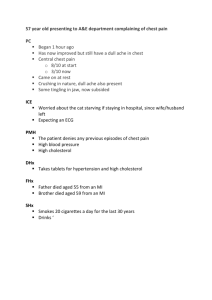
Chief Complaint: Severe chest tightness and dizziness since last night. Present Illness: This 64 y/o female patient has the past history of type 2 DM, essential HTN, CRF, CAD (TVD) post CABG, and CHF Fc III. For many years, she has the symptoms of dizziness in the evening, and chest tightness at midnight causing her awake from sleep, without any precipitating factors. The frequency is about once a week. But these symptoms always subsided in a few minutes without any treatment, or sometimes, with NTG sublingual use; so she just ignored them. DOE (climbing stairs) was also noted, but orthopnea, and PND were denied. This time, she suffered from severe chest tightness accompanying dizziness and didn’t get improved despite 2 pills NTG on 02/06 midnight. Legs swelling was also noted then. But sweating, radiating pain, nausea and vomiting were all denied. Therefore, she was sent to our ER and after some examination and treatment, she was admitted for further evaluation and treatment. Dr Buttrey’s rewrite: CC: 64 yo female c/o dizziness for [How long?] PI: The patient has had a long history of intermittent dizziness in the evening and chest tightness at midnight awaking her from sleep, occurring about once a week. In the past, the symptoms always subsided in a few minutes, either without any treatment or with sublingual NTG. She was diagnosed with CAD (TVD) [When? Previous MI?] and underwent CABG [When? With what results?] and has had CHF Fc III [When?]. She notes DOE (climbing stairs [How many flights?]) but denies orthopnea and PND. The night before admission at midnight, she had severe chest tightness, accompanied by dizziness, and which didn’t improve despite 2 NTG. She also noted [?] bilateral ankle edema [Sudden onset?] but denied sweating, radiating pain, nausea or vomiting [SOB, palpitation?]. She came to our ER [where EKG and/or enzymes showed what?] Therefore, she was sent to our ER and after some examination and treatment, she was admitted for further evaluation and treatment. The patient has a history of Type 2 DM and essential HTN (see PMH). [Smoking, hyperlipidemia, FH of CAD, sedentary life style?] Missing data: The duration of the symptoms in the CC—we know when they began (midnight) but not how long they persisted. More detail on her past CAD history, i.e., when diagnosed and treated, results of the CABG, whether symptoms have been stable or worsening. The degree of DOE. Clarification on the CHF functional class—always or on occasion in the past? Important findings in the ER. Other CAD risk factors. Comments Content: I’d call this a “bare bones” HPI. It gives us enough information to know that we might be dealing with an acute coronary syndrome (ACS), but more data is required, both to deepen our understanding of her condition in the past and to determine what is needed for optimal treatment of the current episode and in the future. Also, there seems to be an assumption that this is indeed ACS, but I wonder whether other diagnoses were or should have been considered, e.g., was there anything suggestive of a pulmonary embolus or other non-cardiac cause underlying her symptoms? Perhaps not, but there isn’t enough information in the history to exclude those with confidence. Duration of symptoms is extremely important. There’s a difference between several minutes and several hours of chest tightness. The fact that you wrote that her symptoms began at midnight indicates you know the importance of timing, but you then also need to state when she arrived in the ER and whether she was still symptomatic on arrival. Another question about timing is when the past events related to her CAD occurred, as well as how things have been since then. By noting CHF Fc III, do you mean she’s chronically that disabled, or was that simply a diagnosis at one point in the past. If she can climb stairs at all, her CHF might normally be class II or better. Also, the way it’s written, it sounds as if the edema occurred suddenly. That’s unusual, but it’s possible. Is it what you meant? Your mention of associated symptoms is good, though I’d usually want to hear as well whether there was SOB and palpitation in someone with suspected ischemic heart disease. Similarly, other known risk factors should be mentioned, whether present or absent. Note that I have added “(see PMH)” after the DM and HTN. They should be described more fully in the PMH, including the degree of control (i.e., what her BP and HgA1c usually are). While our first priority is managing this woman’s acute presentation, we should be looking for ways to improve her overall status. Is she receiving the medications she ought to be on? If so, does she take them as directed? Is there any way her treatment could be improved so as to improve her functional status? The other issue is to investigate any factors that might account for her acute problem, e.g., infection, arrhythmia, unusual exertion, dietary indiscretion, running out of medicines, emotional stress, etc. “Therefore, she was sent to our ER and after some examination and treatment, she was admitted for further evaluation and treatment.” This sentence tells us almost nothing except that someone thought she was sick enough to be admitted. Either tell us the relevant findings in the ER, including their initial diagnosis, or don’t write about them at all. Also, we know that patients are usually admitted “for further evaluation and treatment,” so don’t bother writing it. The only time you need to explain the reason for the admission is if isn’t clear from the rest of the HPI. English: so she just ignored them: This is OK, although it sounds a bit as if we’re blaming the patient. I prefer something like “the symptoms weren’t bothersome enough for her to see a doctor.” severe chest tightness accompanying dizziness: “severe chest tightness accompanied by dizziness.” The way you have written it is correct if you mean that the most severe symptom was dizziness and the chest tightness accompanied it but was less troublesome. However, I think your primary focus is on the chest tightness. didn’t get improved: “didn’t improve” legs swelling: We usually say “ankle edema” or “pedal edema” (pedal means feet). If it’s severe, state how much, e.g., edema to the knees, etc. Also, be sure to note whether unilateral or bilateral. I assume you meant bilateral by writing “legs.” Unfortunately, that’s grammatically incorrect! The noun leg (or ankle, as we commonly say) is functioning as an adjective modifying swelling (or edema). As such, it has to be singular, not plural. So you must add another word—unilateral or bilateral—to indicate its location.