File - Jiali Luc RN to BSN Portfolio
advertisement

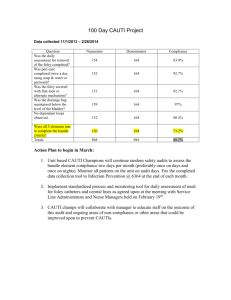
Running head: LEADERSHIP STRATEGY ANALYSIS Leadership Strategy Analysis-Quality Improvement Process Jiali Luc Ferris State University 1 LEADERSHIP STRATEGY ANALYSIS 2 Abstract Quality improvement (QI) process is an important component to prevent and decrease hospital acquired infections and nursing leadership is critical in this process. The six steps of the QI process are also correlated to nursing process, which can be applied easily to the QI process. The six steps include identifying a need, assembling a team, collecting data, establishing outcomes, making a plan, and evaluating the plan. These steps are applied to catheter associated urinary tract infection (CAUTI) prevention in the hospital setting. The QI team understands the process and incorporates this to the clinical needs and best outcomes are achieved. LEADERSHIP STRATEGY ANALYSIS 3 Leadership Strategy Analysis The quality improvement (QI) process is an ongoing process for achieving quality health care and improving customer satisfaction. The QI process involves a series of steps designed to plan, implement, and evaluate changes in healthcare activities. One of the models of the QI process resembles the nursing process (Yoder-Wiser, 2011). According to Draper, Felland, Liebhader, and Melichar (2008), the QI process will be more successful if hospitals have supportive leadership, a philosophy of quality as everyone’s responsibility, physician and nurse champions, and valuing of feedbacks from multidisciplinary teams. According to Yoder-Wiser (2011), there are six steps involved in the QI process which are identifying a need, assembling a team, collecting data, establishing outcomes, making a plan to achieve the outcomes, evaluating the plan, and making changes when needed according to outcomes. Nursing leadership is important to the QI process in hospitals. To demonstrate the QI process strategy this author applied it to the need of catheter associated urinary tract infections (CAUTI) prevention in hospital setting. Clinical Need According to the Center of Disease Control and Prevention (CDC) (2009), urinary tract infections (UTIs) are the second most common type of healthcare associated infection, and approximately 75% of UTIs are associated with a urinary catheter. The most common cause of CAUTIs is due to prolonged use of an indwelling urinary catheter. Patients receive a catheter for many reasons such as surgical need, urinary retention, neurogenic bladder, and the need to measure accurate intake and output. However, inappropriate use of urinary catheter will increase the risk of CAUTIs. According to Oman, Makic, Fink, Schraeder, Hulett, Keech, & Wald (2011), there are over 500,000 CAUTIs occur yearly in the United States, and CAUTI is the LEADERSHIP STRATEGY ANALYSIS 4 single largest sources of bacteremia in hospitalized patients leading to unnecessary antimicrobial use, prolonged hospitalizations, and increased health care costs. Furthermore, The Centers of Medicare and Medicaid Services no longer reimburse hospitals for additional care costs associated with CAUTI, and the hospitals will be held accountable for the cost related to CAUTI (Schneider, 2012). There are many risk factors that lead to CAUTI. For an example, in the acute care setting, there are many surgical patients that remain catheterized beyond 48 hours postoperatively. In addition, medical patients who have a urinary catheter without a clear indication for the need, staff who break sterile technique when inserting catheter or obtain urine sample from catheter, lack of appropriate skills for daily catheter care, and patients who do not receive education of how to take care of their catheters. Healthcare professionals that know the risk factors of CAUTIs are beneficial to decrease risks of catheter associated urinary tract infections. Reducing the number of CAUTIs has many advantages including improving patients’ satisfaction, improving quality of health care, improving reputation of the organization, and decreasing healthcare cost. Prevention of catheter associated urinary tract infections is a great topic for the QI process. Interdisciplinary Team According to Yoder-Wiser (2011), quality improvement team members should have people from different disciplines who are involved with the problem. To maximize success, the team members should clearly know their roles before starting the QI process. The members of the QI interdisciplinary team in the hospital are medical surgical service director, clinical nurse educator, infection control nurse, CAUTI champion facilitator, managers from each department and Registered Nurse champion representatives from each unit throughout the hospital. Each LEADERSHIP STRATEGY ANALYSIS 5 problem for the QI process requires different amounts of meeting times and input is needed from each discipline. For the CAUTIs prevention problem, monthly meetings are set on Monday and primarily involve all members from the QI process team. All registered nurses are welcome to join the meeting, even if they are not a member of the QI team. The RN facilitator of the QI process always makes an agenda for the meeting, the nurse educator shares the most evidence-based practices related to CAUTI prevention, the infection control nurse reports the number of CAUTIs in each unit and the Registered Nurse champion will share the information learned from the meeting with the unit, and make sure nurses follow evidence-based practice regarding to CAUTI. Data Collection Method Foley catheter use is monitored everyday in each department. The charge nurse collects the number of catheters used in each unit and reports to the department manager. Every nurse needs to assess and understand what the indication for his or her patients who have catheters. If patient has a catheter that does not meet the criteria set by the hospital policy, then the nurse needs to communicate with the physician to obtain an order to discontinue the catheter or justify in writing why one is needed. The hospital designs a member from the QI process to collect data related to CAUTI. An algorithm flow chart is used to determine if the urinary tract infection is related to urinary catheter use. According to the hospital’s flow chart, the infection is CAUTI if the criteria are met. The hospital used the criteria according Center Disease Control to track the numbers of CAUTIs, and these criteria as follow: 1. The urine culture was not taken same day or before Foley catheter was inserted. 2. Patient had a Foley catheter discontinued at anytime in the 48 hours prior to Specimen collection. LEADERSHIP STRATEGY ANALYSIS 6 3. Patient has at least one of the follow symptoms: fever greater than 100.04 Fahrenheit or 38 Celsius, urgency, frequency, dysuria, suprapubic tenderness, and costovetebral angle pain or tenderness. 4. Urine culture has less than or equal to 100,000 CFU. Urinalysis has least one of the Follow symptoms: positive dipstick for leukocyte esterase, positive dipstick for nitrite, greater than 2 WBC, and bacteria or yeast observed. (CDC, 2009) Establishes Outcomes There are national and corporate benchmarks that the hospitals are expected to meet. The corporate benchmark is use to monitor the hospital’s progress to reduce CAUTIs. According to the CDC (2009), the five-year national prevention target will be 25 percent. Hospital performance is measured against the center for Medicare and Medicaid services quality standards. Monthly reports are submitted for comparison and targets. The reason for the quality measure is because CAUTIs are preventable. According to Elpern, Killen, Ketchem, Wiley, Patel, and Lateef (2009), the most important intervention is limiting catheter use and removing catheters as soon as indications for their use are no longer present. The hospitals incorporate the most evidence-based practice of urine “8” catheter bundle and guideline from Center Disease Control to prevent CAUTIs. The summary of the bundles includes: 1. Good hand hygiene and Universal Precautions. 2. Nurses will insert catheters only when necessary and ordered by physician-attempt alternatives using caregiver teamwork. 3. Pericare. 4. Obtain UA after inserting catheter only if criteria are met. 5. Secure catheter to patient’s body using tape or Velcro strap device: allow slack in LEADERSHIP STRATEGY ANALYSIS 7 catheter to avoid tension on urethra, secure tubing to top of inner thigh to prevent movement and urethral traction, and secure tubing to bed using clip. 6. Keep system closed, do not break the seal between the catheters and bag. 7. Prevent backflow: position the tubing and bag below the bladder, and empty urine in tubing into the bag is the bag will be lifted above the bladder. 8. Nurse will assess and document the need for a catheter daily, and remove as soon as possible. (Gould, Umscheid, Agarwal, Kuntz, and Pegues, 2009) Most hospitals use the catheter care bundle to decrease the risk of CAUTIs. However, the most important thing to remember is to avoid the insertion of catheter, if possible, in order to prevent CAUTIs. Implementation Strategies The process for data collection and implementation from the data are as follows: The infection control nurse reports the rate for CAUTIs in a QI meeting of the previous month of the hospital. The QI team checks to see which department has the most cases of CAUTIs, and then they work as a team to investigate factors leading to more CAUTIs in that unit. The QI team will check on patients’ medical record to see how long each patient has a catheter, and the indication for it. The unit champion makes sure all the staff including patient care technicians understands the eight ways to decrease CAUTIs. After reviewing the data and the findings indicate staff do not follow the catheter care bundle, education will be provided and enforced. According to Yoder-wiser (2011), Quality Improvement process stresses improving the system rather than assigning blame to employees. Open communication and education of staff are important to success in a change process. LEADERSHIP STRATEGY ANALYSIS 8 As a result, once the issue of CAUTI prevention is known, a plan is implemented. If staff lacks education regarding CAUTI prevention, an education section will be provided. If policies and procedures need to be changed, they are changed accordingly. Communication among staff is most critical at all times especially during implementation stage. Open communication is encouraged because the QI process will be successful only when feedback and input is received from all staff, especially staff caring for patients. Evaluation Measuring improvement prevention of CAUTI is done by audits. The QI team continues to check on data or numbers of CAUTIs to see if the number of CAUTIs have been decreased or increased. If the number of CAUTIs has increased or no improvements are made in the consecutive months, it is a good indication that the process is not working and needs to change (Yoder-wiser, 2011). As a result, the team continues to gather and evaluate data to see what the obstacles were that lead to the outcome not being met. Once the problem has been identified, revisions in the implementation plan change accordingly. The QI team continues to monitor the data again, and if the outcomes are met that means that the actions plan is in the right direction and normal monitoring continues from that point on. Scholarship The acute care hospital use standards of care to achieve the desired outcomes. These clinical practice guidelines are based on the most current evidence based practice standard. Furthermore, the hospital follows the recommended prevention guideline provided from Center Disease Control and Prevention. It is very important for healthcare systems to use the most up to date evidence based practice to promote quality and safety patient care. Conclusion LEADERSHIP STRATEGY ANALYSIS 9 Catheter associated urinary tract infections are most common hospital acquired infection. Hospitals use solid evidence based practice intervention; the rate of CAUTIs can be decreased dramatically. The QI process is important for prevention or reduction of infection. The hospital requires strong nursing leadership in a driving force of the QI process. LEADERSHIP STRATEGY ANALYSIS 10 References Center for Disease Control and Prevention. (2009). Catheter-associated urinary tract infections Retrieved from: http://www.cdc.gov/HAI/ca_uti/uti.html Draper, D. A., Felland, L. E., Liebhaber, A., & Melichar, L. (2008). The role of nurses in hospital quality improvement (HSC Research Brief No. 3). Retrieved from Center for Studying Health System Change website: http://www.hschange.com/CONTENT/972/ Elpern, E. H., Killeen, K., Ketchem, A., Wiley, A., Patel, G., & Lateef, O. (2009). Reducing use of indwelling urinary catheters and associated urinary tract infections. American Journal of Critical Care, 18(6), 535-541, doi: 10.4037/ajcc2009938 Gould, C. V., Umscheid, C. A., Agarwal, R. K., Kuntz, G., & Pegues, D. A. (2009). Guideline for prevention of catheter-associated urinary tract infections 2009. Center for Disease control and Prevention. Retrieved from: http://www.cdc.gov/hicpac/pdf/cauti/cautiguideline2009final.pdf Oman, K. S., Makic, M. B. F., Fink, R., Schraeder, N., Hulett, T., Keech, T., & Wald, H. (2011). Nurse-directed interventions to reduce catheter-associated urinary tract infections. American Journal of Infection Control, 1-6. Schneider, M. A. (2012). Prevention of catheter-associated urinary tract infections in patients with hip fractures through education of nurses to specific catheter protocols. Orthopaedic Nursing, 31 (1), 12-18. Yoder-Wiser, P. S. (2011). Leading and managing in nursing (5th ed.). St Louis, MO: Elsevier Mosby LEADERSHIP STRATEGY ANALYSIS 11