Admission H&P Example: Chest Pain, Anemia, Diabetes
advertisement

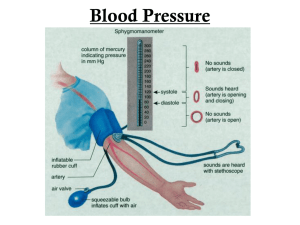
SUTTER COAST HOSPITAL EXAMPLE - ADMISSION H&P, Hassan Sheikho, M.D. [DATE OF ADMISSION automatically added by iTran] ADMISSION DIAGNOSES: 1. Chest pain, rule out myocardial infarction. 2. Microcytic anemia. 3. Diabetes mellitus, insulin dependent, uncontrolled. HISTORY: The patient is a 51-year-old white female who presented to the emergency room after sudden onset of dull chest pain. The chest pain was substernal, radiating into her left arm, arrived with rest, relieved with nitroglycerin by the paramedics. The patient also had some mild shortness of breath with it, but no nausea. The patient otherwise has no known history of coronary artery disease. No history of angina. She has multiple risk factors for coronary artery disease including obesity, diabetes mellitus, hypertension, but no known history of hypercholesterolemia and no significant family history of coronary artery disease. The patient denied any recent illness. No shaking chills. No fever, no cough, and no other upper respiratory symptoms. PAST MEDICAL HISTORY: As mentioned above plus chronic back pain. In addition, diabetes mellitus for nine years, insulin dependence, history of hypertension, history of chronic back pain, and history of allergic rhinitis. MEDICATIONS: The patient takes Lantus 70 units subcu q.h.s., lisinopril 40 mg p.o. daily, Norvasc 5 mg p.o. daily, Neurontin 300 mg p.o. daily, Flonase nasal spray 1 puff daily, Vicodin p.r.n. ALLERGIES: SULFA. FAMILY HISTORY: Noncontributory. SOCIAL HISTORY: The patient is disabled secondary to her back pain. She does not smoke and does not drink alcohol. Lives in Klamath by herself. REVIEW OF SYSTEMS: The patient denies any headache, any change in vision, no palpitations, no cough, no fever, no shaking chills. No change in bowel movement, no change in urinary output, and no rash. PHYSICAL EXAMINATION: GENERAL: The patient is anxious, but not in acute distress. VITAL SIGNS: Her blood pressure on arrival to the emergency room showed to 139/70, pulse 92, respiratory rate 20, temperature 37. HEENT: Showed no erythema or jaundice. Oropharynx clear. NECK: No lymphadenopathy. No JVD. CHEST: Bilateral crackles, mostly in the lower lobes. No wheezing. CARDIOVASCULAR: Regular rate and rhythm. No murmur. ABDOMEN: Soft, obese. Bowel sounds positive. EXTREMITIES: +1/2 pitting edema bilaterally. NEUROLOGICAL: Exam no focal weakness. LABORATORY DATA: EKG showed sinus rhythm with poor R-wave progression. Chest x-ray showed vascular congestion, otherwise noncontributory. The rest of labs showed a sodium 138, potassium 3.6, chloride 104, bicarb 26, glucose 299, BUN 13, creatinine 0.9, AST 10, ALT 36. CPK initially 48, troponin less than 0.04. White blood cells 6.9, hemoglobin 10.5, hematocrit 35.4, platelets 316, MCV 74. ASSESSMENT AND PLAN: 1. Chest pain, rule out myocardial infarction. The patient has multiple risk factors for coronary artery disease including obesity, diabetes, high blood pressure. The patient will be admitted to a monitored bed with serial EKGs, serial cardiac enzymes. Start oxygen, nitroglycerin, aspirin, beta blocker per protocol. In the meantime continue risk stratification with fasting lipids, TSH, and HBA1C. 2. Diabetes mellitus, insulin dependent, poor control. Continue with the patient's Lantus. She stated that she is allergic to short acting insulin and most oral medications. I will discuss with her primary care physician her options. 3. History of hypertension. Continue the patient's ACE inhibitor. 4. Get an echocardiogram to evaluate for clinical crackles in her lower lobes bilaterally to optimize her management.