1 - Kentucky Medical Association
advertisement
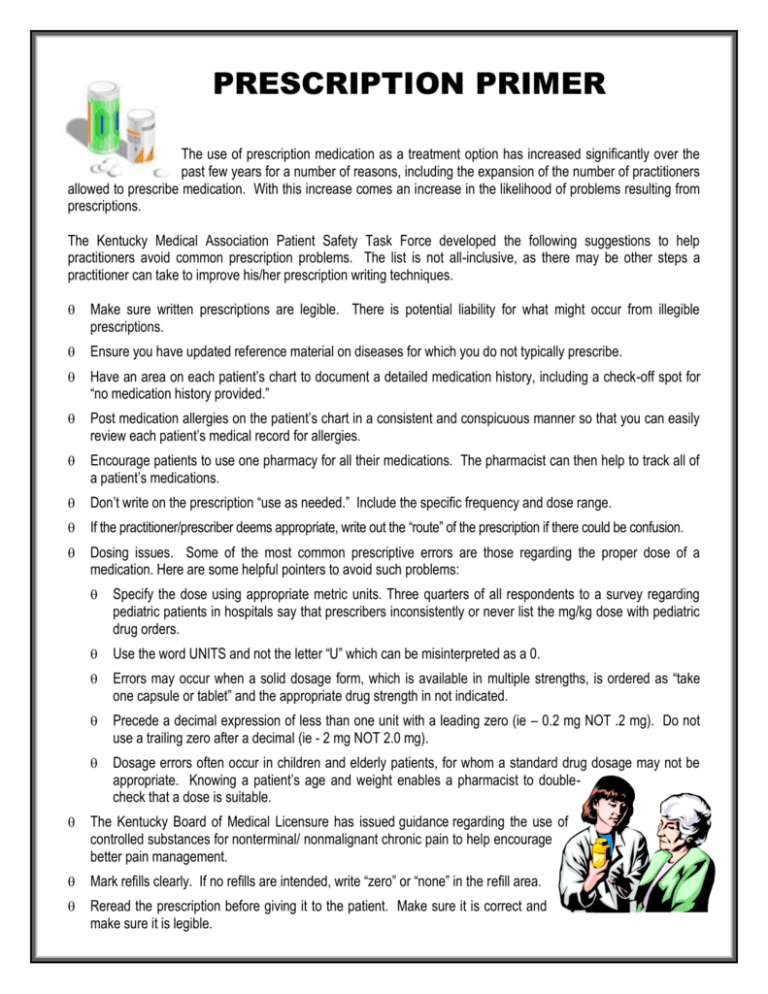
PRESCRIPTION PRIMER The use of prescription medication as a treatment option has increased significantly over the past few years for a number of reasons, including the expansion of the number of practitioners allowed to prescribe medication. With this increase comes an increase in the likelihood of problems resulting from prescriptions. The Kentucky Medical Association Patient Safety Task Force developed the following suggestions to help practitioners avoid common prescription problems. The list is not all-inclusive, as there may be other steps a practitioner can take to improve his/her prescription writing techniques. Make sure written prescriptions are legible. There is potential liability for what might occur from illegible prescriptions. Ensure you have updated reference material on diseases for which you do not typically prescribe. Have an area on each patient’s chart to document a detailed medication history, including a check-off spot for “no medication history provided.” Post medication allergies on the patient’s chart in a consistent and conspicuous manner so that you can easily review each patient’s medical record for allergies. Encourage patients to use one pharmacy for all their medications. The pharmacist can then help to track all of a patient’s medications. Don’t write on the prescription “use as needed.” Include the specific frequency and dose range. If the practitioner/prescriber deems appropriate, write out the “route” of the prescription if there could be confusion. Dosing issues. Some of the most common prescriptive errors are those regarding the proper dose of a medication. Here are some helpful pointers to avoid such problems: Specify the dose using appropriate metric units. Three quarters of all respondents to a survey regarding pediatric patients in hospitals say that prescribers inconsistently or never list the mg/kg dose with pediatric drug orders. Use the word UNITS and not the letter “U” which can be misinterpreted as a 0. Errors may occur when a solid dosage form, which is available in multiple strengths, is ordered as “take one capsule or tablet” and the appropriate drug strength in not indicated. Precede a decimal expression of less than one unit with a leading zero (ie – 0.2 mg NOT .2 mg). Do not use a trailing zero after a decimal (ie - 2 mg NOT 2.0 mg). Dosage errors often occur in children and elderly patients, for whom a standard drug dosage may not be appropriate. Knowing a patient’s age and weight enables a pharmacist to doublecheck that a dose is suitable. The Kentucky Board of Medical Licensure has issued guidance regarding the use of controlled substances for nonterminal/ nonmalignant chronic pain to help encourage better pain management. Mark refills clearly. If no refills are intended, write “zero” or “none” in the refill area. Reread the prescription before giving it to the patient. Make sure it is correct and make sure it is legible. For verbal prescriptions, have the filler read the prescription back to you. Monitor patients for side effects, allergies, etc, especially with controlled substances. Educate patients about their medications. emphasizing what is medically significant. Ho w t o M a na ge Your M e d ica t io n s Practitioners should counsel patients on their medications, The KMA Patient Safety Task Force has developed an informational flyer entitled "How to Manage Your Medications" for patients to help them avoid common medication errors. If you would like a copy of the flyer to give to your patients or hang in your office, contact the Kentucky Medical Association. A p ub li ca tio n o f t he Kent ucky Medica l Asso ciati on Patie nt Sa fety Ta sk Force CONFUSING ABBREVIATIONS Abbreviations in one health care setting may have a different meaning in another setting. Below are some common abbreviations that could lead to misinterpretation, especially if poorly written. Abbreviation Intended Meaning U µg Q.D. Q.O.D. SC or SQ TIW D/C HS cc AU, AS, AD Common Error Mistaken as a zero or a four (4), resulting in overdose. Also mistaken for "cc" (cubic centimeters) when poorly written. Micrograms Mistaken for "mg" (milligrams), resulting in overdose. Latin abbreviation for The period after the "Q" has sometimes been mistaken for an "I," and the drug has been every day given "QID" (four times daily) rather than daily. Latin abbreviation for Misinterpreted as "QD" (daily) or "QID" (four times daily). If the "O" is poorly written, it every other day looks like a period or "I." Subcutaneous Mistaken as "SL" (sublingual) when poorly written. Three times a week Misinterpreted as "three times a day" or "twice a week." Medications have been prematurely discontinued when D/C (intended to mean Discharge; "discharge") was misinterpreted as "discontinue" because it was followed by a list of also discontinue drugs. Half strength Misinterpreted as the Latin abbreviation "HS" (hour of sleep). Cubic centimeters Mistaken as "U" (units) when poorly written. Latin abbreviation for both ears, left ear, Misinterpreted as the Latin abbreviation "OU" (both eyes), "OS" (left eye), "OD" (right eye). right ear Units This information developed by the Kentucky Medical Association Patient Safety Task Force should not be considered as a substitute for the professional judgement of medical practitioners and it does not establish a standard of medical practice. It is offered only as a suggestion. Kentucky Medical Association Patient Safety Task Force 4965 US Hwy 42, Suite 2000 Louisville, Kentucky 40222 Copyright © 2001 by the Kentucky Medical Association Patient Safety Task Force.