Seminar 11
advertisement
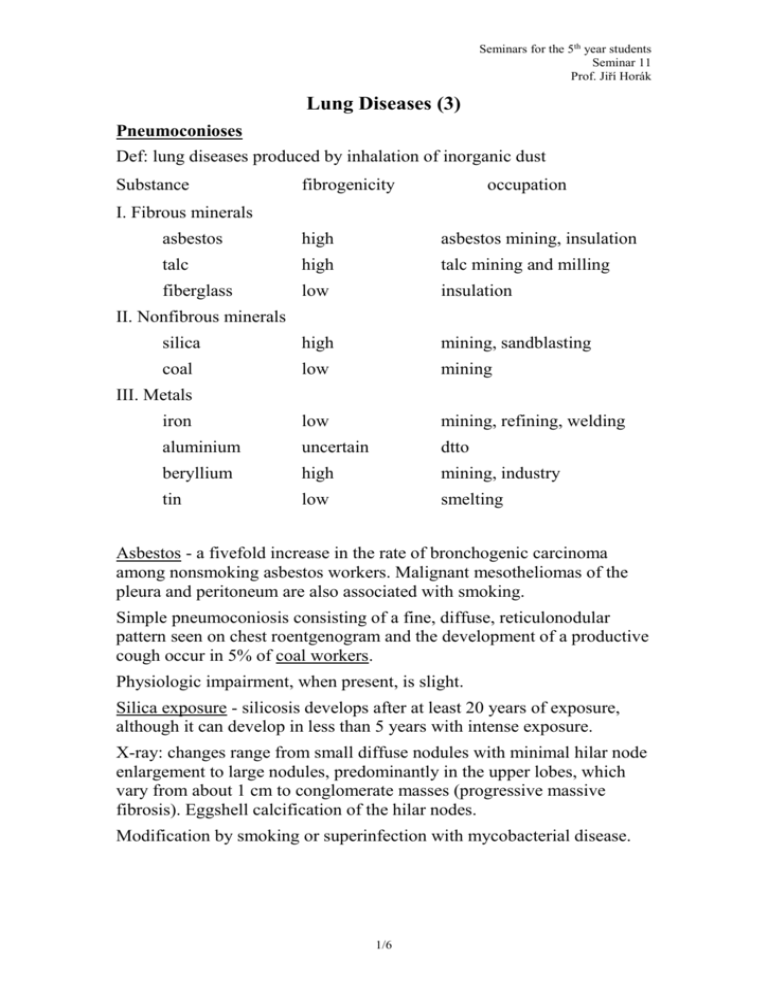
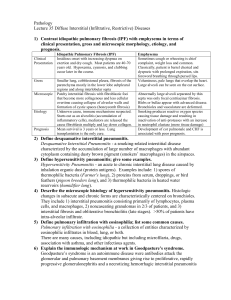
Seminars for the 5th year students Seminar 11 Prof. Jiří Horák Lung Diseases (3) Pneumoconioses Def: lung diseases produced by inhalation of inorganic dust Substance fibrogenicity occupation I. Fibrous minerals asbestos high asbestos mining, insulation talc high talc mining and milling fiberglass low insulation silica high mining, sandblasting coal low mining iron low mining, refining, welding aluminium uncertain dtto beryllium high mining, industry tin low smelting II. Nonfibrous minerals III. Metals Asbestos - a fivefold increase in the rate of bronchogenic carcinoma among nonsmoking asbestos workers. Malignant mesotheliomas of the pleura and peritoneum are also associated with smoking. Simple pneumoconiosis consisting of a fine, diffuse, reticulonodular pattern seen on chest roentgenogram and the development of a productive cough occur in 5% of coal workers. Physiologic impairment, when present, is slight. Silica exposure - silicosis develops after at least 20 years of exposure, although it can develop in less than 5 years with intense exposure. X-ray: changes range from small diffuse nodules with minimal hilar node enlargement to large nodules, predominantly in the upper lobes, which vary from about 1 cm to conglomerate masses (progressive massive fibrosis). Eggshell calcification of the hilar nodes. Modification by smoking or superinfection with mycobacterial disease. 1/6 Seminars for the 5th year students Seminar 11 Prof. Jiří Horák Th: no specific treatment, removal from the offending environment, search for mycobacterial disease, cessation of smoking, the use of oxygen to treat complicating cor pulmonale Hypersensitivity pneumonitis (extrinsic allergic alveolitis) caused by abnormal sensitivity to some organic agent 4 - 6 hours following exposure in a sensitized subject there is the onset of cough, dyspnea, fever, and malaise. Wheezing is usually absent. Phys: diffuse crackles X-ray: nodular or reticulonodular infiltrates with relative sparing of the apices. In most cases, these symptoms gradually resolve but recur on subsequent exposure. Repeated exposure - development of pulmonary fibrosis and restrictive lung disease. Hypersensitivity pneumonitis antigen source disease examples Thermophilic bacteria moldy hay farmer‘s lung Bacillus subtilis etc. water humidifier lung fungi moldy organic material, maple bark-stripper‘s water lung animal protein bird droppings pigeon breeder‘s lung amoeba water humidifier lung Pathogenesis: both immune complex and cell-mediated immune mechanisms Th: avoid or remove the offending agent. In acute situations corticosteroids Primary pulmonary hypertension a disease of young adult women. Pathogenesis: extrinsic or intrinsic stimulus in genetically predisposed individuals. Inflammatory or immunologic injury to the pulmonary endothelium results in an imbalance of locally produced vasoconstrictor 2/6 Seminars for the 5th year students Seminar 11 Prof. Jiří Horák (thromboxane, endothelin) and vasodilator (prostacyclin) factors pulmonary thrombosis in situ. Clin: progressive dyspnea and exercise limitation, syncopes, fatigue, chest pain, cor pulmonale. Dg: right heart catheterization Th: chronic anticoagulation, high doses of calcium channel blockers, prostacyclin, inhaled nitric oxide, combined heart-lung transplantation Prognosis: 20% survive 3 years Common drug-induced lung disease drug dose relation appearance I. Cancer chemotherapeutics bleomycin both acute and dose dependent pulmonary fibrosis busulfan > 600 mg pulmonary fibrosis chlorambucil >2g pulmonary fibrosis methotrexate none pneumonitis II. Analgesics and hypnotics aspirin serum level > 45 mg/dl pulmonary edema ethchlorvynol, overdose pulmonary edema propoxyphene HCl, heroin opiates and other chronic i.v. abuse psychotropic drugs pulmonary fibrosis and vasculitis III. Antibiotics nitrofurantoin acute hypersensitivity pneumonitis sulfonamides chronic pulmonary fibrosis, Löffler‘s syndrome Sarcoidosis Def: systemic disease of unknown etiology characterized by noncaseating granulomas found diffusely throughout the body. It occurs most commonly in the 20s and 30s. 3/6 Seminars for the 5th year students Seminar 11 Prof. Jiří Horák Pathogenesis: T-cell activation Lab: increased percentage of lymphocytes in bronchoalveolar lavage fluid is a marker of alveolitis Pathol: organs involved: lungs, skin, lymph nodes, liver, spleen, eyes, joints, CNS, muscles Clin: lungs - progressing cough and shortness of breath, pulmonary fibrosis with respiratory insufficiency Löfgren‘s syndrome - fever, arthralgias, bilateral hilar adenopathy, erythema nodosum skin - lupus pernio (papules, plaques and subcutaneous nodules of the nose) or plaques CNS - cranial nerve palsies, diabetes insipidus, subacute meningitis joints – arthritis eyes – uveitis, conjunctivitis, retinal involvement, keratoconjuntivitis sicca (when lacrimal and salivary glands are involved) → steroid Th peripheral lymphadenopathy and/or splenomegaly granulomatous hepatitis heart - arrhythmias, conduction disturbances hypercalcemia with nephrocalcinosis or nephrolithiasis Dg: transbronchial biopsy during bronchoscopy, X-ray, liver biopsy, Kveim test. Pulmonary function tests: restriction + decreased diffusion capacity. Depressed tuberculin reaction. Th: corticosteroids, ketoconazole for hypercalcemia Prognosis: complete resolution of symptoms and chest radiographic changes within 1 - 2 years. Persistent mild abnormality in a minority of patients. In 10% severe progressive disease with pulmonary fibrosis or significant extrapulmonary involvement. ARDS (Adult Respiratory Distress Syndrome; non-cardiogenic pulmonary edema) ARDS can occur as the result of direct lung injury (e.g. aspiration of gastric acid contents, viral pneumonia) or as part of MODS. Conditions associated with ARDS - shock (traumatic, septic, etc.) 4/6 Seminars for the 5th year students Seminar 11 Prof. Jiří Horák - infection (pneumonia – viral, bacterial, pneumocystis carinii; G- sepsis) - trauma (fat emboli, head injuries, lung contusion) - aspiration (gastric contents, fresh or salt water) - drug overdose (narcotics, barbiturates) - metabolic disorders (poancreatitis, uremia) - inhaled toxins (O2, smoke, corrosives) - blood disorders (DIC, massive blood transfusions) - miscellaneous (radiation, eclampsia, raised intracranial pressure, seizures, high altitude) The Multiple Organ Dysfunction Syndrome (MODS): the presence of altered organ function in an acutely ill patient such that homeostasis cannot be maintained without intervention. Microcirculation is the primary target of injury. Pathogenesis: alveolar-capillary membrane injury → ↑ permeability of endothelium and epithelium → interstitial and alveolar edema → ↓ surfactant alveolar and airway filling and closure ↓ compliance, intrapulmonary shunting hypoxemia ARDS – diagnostic criteria: - proper clinical setting (pneumonia, shock etc.) - PaO2 to FiO2 ratio is ≤ 200 on FiO2 > 0.60 (FiO2 = fractional concentration of inspired O2) - diffuse pulmonary infiltrates on chest radiography - pulmonary artery wedge pressure ≤ 18 mm Hg (normal left atrial pressure) 5/6 Seminars for the 5th year students Seminar 11 Prof. Jiří Horák Th: - Swan-Ganz catheter into the pulmonary artery - intubation and mechanical ventilation (oxygenation with the use of high tidal volumes and PEEP) - maintaining fluid balance (PAWP 6 – 8 cm H2O) - sepsis is the commonest cause of death → antibiotics - corticosteroids are not indicated Outlook: 50 – 70% mortality, nearly 100% mortality in ARDS as a part of MODS Of those who survive most recover normal lung function ------------------------ 6/6