NSAIDs
advertisement

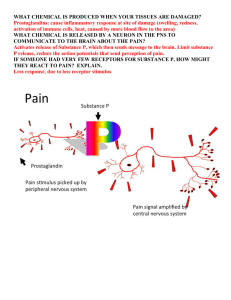
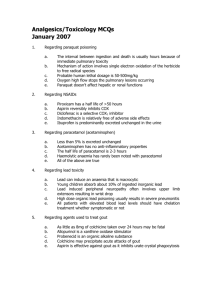
Antipyretic-analgesic and Anti-inflammatory Overview Drugs Aspirin-like drugs Aspirin is the representative drug. Non-steroidal anti-inflammatory drugs (NSAIDs) NSAIDs differ from glucocorticoids in the mechanism of anti-inflammatory action. [Shared characteristics of NSAIDs] mechanism of actions pharmacological effects adverse reactions The shared mechanism of reactions Metabolism of arachidonic acid Phospholipids phospholipase A2 glucocoids lipoxygenase Arachidonic acid COX 5-HPETE NSAIDs PGG2 PGI2 synthetase (vascular endothelium) iosmerase leukotriens PGI2 PGE2 PGH2 reductase PGF2α TXA2 synthetase (platelet) TXA2 PG is a family of polyunsaturated fatty acids, almost existing in each kind of tissue and body fluid. It can promote inflammation, pain,fever and support the function of platelet and protect the lining of stomach and regulate the resistance of peripheral vessels, etc. TXA2 : promote platelet aggregation vasoconstriction PGI2 : inhibit platelet aggregation vasodilatation gastric protection PGE2 : induce inflammation cause fever and pain cause vasodilatation PGF2α : vasoconstriction causing pain LTs : allergy contraction of bronchial smooth muscle [Introduction of COX] 1 COX exists in two enzyme isoforms: COX-1 and COX-2. Each of them has different characteristics. COX-1 COX-2 Production Constitutive Inducible Function Physiological function Pathological function gastric protection facilitate inflammation platelet aggregation cause fever and pain peripheral vessel regulation renal blood distribution NASIDs effects unwanted side effects therapeutic effects [The shared mechanism of NSAIDs] inhibit the enzyme cyclo-oxygenase (COX) and cause inhibition of biosynthesis of prostaglandins (PGs). Three major actions of NSAIDs 1. Antipyretic effect The antipyretic effect of NSAIDs locates in center. 2. Analgesic effect 3. Anti-inflammatory effect 1. Antipyretic effect Mechanism: inhibit the biosynthesis of PGs in the CNS Characteristic: NSAIDs reduce elevated temperature, whereas normal body temperature is slightly affected. 2 Table 21-2 Comparison between NSAIDs and Chlorpromazine Mechanism Effect heat-regulating center Clinic uses on NSAIDs Inhibit hypothalamic COX, decrease the generation of PGE Reduce elevated temperature, but normal body temperature is only slightly affected. Fever, rheumatic fever, chlorpromazine Directly inhibit hypothalamic heat-regulating center Changed according to the variation of environment Low environment temperature:T↓; high environment temperature:T↑ Artificial hibernation 2. Analgesic effect [Mechanism]: inhibit the synthesis of PGs in periphery [Characteristics]: most effective to mild to moderate pain (eg. toothache, neuralgia, courbature, arthralgia and dysmenorrhea) no euphoria and addiction no respiratory inhibition Table 21-2 Comparison with morphine NSAIDs morphine mechanism decreased prostaglandin Excite opioid-receptor, release P generation structure, inhibit the transformation of algesic information Clinic uses Mild-to-moderate pain All kinds of pain Narcosis respiratory inhibitory (-) (+) and addiction 3 3. Anti-inflammatory effect injury Phospholipids PLA2 AA cytokine↑ (IL-1,6,8 TNF) COX-2 COX-1 NSAIDs PGs BK inflammation [The role of PGs in inflammation] 1. They cause vasodilatation and increase vascular permeability. 2. They also coordinate with BK and cell adhension molecules, amplifing inflammatory effect. [Mechanism of anti-inflammation] 1. Inhibit biosynthesis of PGs in inflammatory sites 2. Inhibit the expression of some cell adhesion molecules 3.Additional possible mechanisms –inhibition of leukocyte chemotaxis –down regulation of interleukin-1 production –decrease the production of free radicals and superoxide –interference with calcium-mediated intracellular events. Section 1 Salicylates Aspirin (ASA) [Process in the body] 1. Absorption: * absorbed rapidly, tpeak=1~2 hours, t 1/2=15min * from stomach but mostly from the upper small intestine 2. Distribution: (metabolite-salicylate) * distribute widely throughout most body tissues, including articular cavity, cerebrospinal fluid and placenta. * is extensively bound to albumin , PPBR highly reaching 80%-90% 3. Metabolism and excretion Most of the salicylates are metabolized in the liver.The product will be excreted by urine,influenced by urine pH. in alkaline urine up to 85% in acidic urine as low as 5% In salicylate acute intoxication, we can reduce the blood concentration and increase the excretion of free salicylates by alkalizing the urine with sodium bicarbonate. [Pharmacological effect and clinical use] 1. Analgesic and antipyretic effect 4 one of the most frequently employed drugs in reducing pain and body temperature. it widely used in headache, toothache,neuralgia, courbature, dysmenorrhea, cold and fever,etc. 2. Anti-inflammation and anti-rheumatic effect relieve the symptoms of redness, swelling, heat and pain caused by inflammation. In high doses, it can be responsible for the treatment of rheumatoid fever, rheumatoid arthritis and other inflammatory joint conditions. [clinical uses] general inflammation rheumatoid and rheumatic arthritis and other inflammatory joint conditions . differential diagnosis and therapy of acute rheumatoid fever 3. Effect on platele Low doses of aspirin produce an effect of anticoagulation. This is due to its irreversible inhibition of platelet COX to reduce the production of TAX2 in platelet. But high doses of aspirin may play an opposite effect. Because high doses of aspirin inhibit PG synthetase directly in vessel endothelium, so as to reduce the synthesis of PGI2. PGI2 is the antagonizer of TAX2, and its reduction may stimulate clot formation. [Clinical uses] ( in low doses ) ① prevent thrombosis ② myrocardial infarction ③ transient cerebral ischemic attack 4.Others (1)Alzheimer,s disease(AD): AD is related to the over-expression of COX-2 in brain. Aspirin 100 mg p.o. daily has repression effect on AD (2)Pregnancy-induced hypertension syndrome and preeclampsia: is related to the increase of the ratio of TXA2 to PGI2 in blood Aspirin 40-100mg p.o. daily can reduce the danger of preeclamapsia [Adverse Reactions] 1. Gastrointestinal effects: At the usual dosage, aspirin’s main adverse reaction is gastric upset. The ingestion of aspirin sometimes result in epigastric distress, nausea, and vomiting. Aspirin also causes gastric ulcer, or even gastrointestinal hemorrhage (on high-dose). 1) stimulate stomach mucous: epigastric distress Directly stimulation By inhibiting COX 2) irritate chemoreceptor trigger zone(CTZ):nausea and vomiting [prevention] * take aspirin after meals, or followed by antacids * take aspirin with endogenous enteric tablet Patients with ulcer should stop aspirin therapy. contraindication: gastric ulcer. 2. Aggravation of bleeding tendency Symptom and Cause * usual dose: inhibit platelet aggregation and prolong the bleeding time * high dose or in long term: 5 inhibit the formation of thrombinogen and prolong the clotting time contraindication * severe hepatic damage * hypoprothrombin-vitamin k deficiency * hemophilia * Aspirin therapy should be stopped 1 week prior to surgery. 3. Allergic effect:angioedema , urticaria, bronchospasm, bronchial asthma ,shock. Aspirin-asthma : a hypersensitive reaction not based on antigen-antibody reaction inhibiting COX →reducing synthesis of PGs → analysing AA into LTs↑ → bronchospasm →bronchial asthma Therapy It can’t be cured by adrenaline, but antihistamine drug and glucocorticoid have good therapy effects. Caution: history of hypersensitivity, asthma and nasal polypus. 4. Salicylism: large dose(>5g) *symptom:With higher doses, patients may experience “salicylism”(special reaction of salicylates)—headache,vertigo,vomiting,tinnitus,sight and hearing failure,hyper-ventilation, acid-base imbalance and even mental disorder * therapy: sodium bicarbonate. 5.Rey’s syndrome * symptom: Children, who are infected by viral disease given aspirin to relieve heat, may be caused Reye’s syndrom. It is shown as severe hepatic dysfunction and encephalopathy. Although it is still in a low incidence, its prognosis is not optimistical. * Prevention: * restriction in children infected with influenza, varicella, and other virus. * substitute aspirin with acetaminophen Drug Interactions 1. Compete the banding to plasma albumin Replace dicoumarol enhance its anticoagulation effect even cause hemorrhage Replace tolbutamide and cause hypoglycemia Replace glucocorticoids enhance its anti-inflammatory effect also enhance its effect of inducing ulcer 2.Compete the autosecretion carriers in renal tubular valproate,furosemide, penicililn, methotrexate and other weak alkaline drugs Section 2 Acetaminophen( Paracetamol) [Pharmacological actions] * similar analgesic and antipyretic effects to aspirin, no significant anti-inflammatory effect * inhibit synthesis of PG in CNS more effectively than in periphery [Clinical uses]: substitutor for antipyretic and analgesic effects of aspirin in: * those patients with gastric complaints * those for whom prolongation of bleeding time would be a disadvantage * Children with viral infections or chicken pox [Adverse reactions]: * Usual dose is safe 6 Frequent symptoms include nausea, vomiting , skin rash, and drug fever. mucous membrane damage occur occasionally. * large doses: hepatic damage Section 3 Other organic anti-inflammatory acids Indomethacin [Pharmacological actions] * the most powerful COX inhibitor,also inhibit PLA2 and PLC * marked anti-inflammatory and anti-pyretic effects [Clinical uses] * rheumatic and rheumatoid arthritis * ankylosing spondylitis * gout * cancerous fever * other unmanageable fever [Adverse effect] ① gastrointestinal effect ② central nervous system effect ③ Hematopoietic system reactions ④ Allergy: In severe patients it can induce asthma. Aspirin-asthma patients is forbidden from the therapy of indomethacin. Sulindac • * half potency of indomethacin • * similar actions and indications to indomethacin • * mainly used for rheumatic arthritis, osteoarthritis • * fewer adverse effects Phenylbutazone & Oxyphenbutazone Pharmacological actions: * strong anti-inflammatory and anti-rheumatic effects * weak antipyretic and analgesic effects Clinical uses * rheumatic and rheumatoid arthritis,* ankylosing spondylitis Ibuprofen • naproxen, ketoproten • * effective COX inhibitor • * slightly gastrointestinal effects • * well tolerant • * widely used in the therapy of rheumatic arthritis and osteoarthritis Piroxicam and Meloxicam 1.Piroxicam * Efficacy of inhibition of COX is similar to indomethacin. * similar therapeutic effects and fewer adverse reactions than aspirin * Main advantage: plasma t1/2 = 50 hours,permits one-daily dosing 2. Meloxicam 7 • • • * One of COX-2 inhibitors * similar indications to piroxicam * strong anti-inflammatory effect and few adverse reactions section 4 selective COX-2 inhibitor Celecoxib * highly selective COX-2 inhibitor,COX-2: COX-1 =375:1 * effective for rheumatic and rheumatoid arthritis, osteoarthritis, postoperational pain and toothache * few adverse effects Nimesulide • *A new type of NSAIDs • * highly selective COX-2 inhibitor • *strong anti-inflammatory effect and few adverse reactions • *used in therapy of rheumatoid arthritis, osteoarthritis, backleg pain, and toothache 8