Eis_-_Aspirin_-_Acetominophen
advertisement
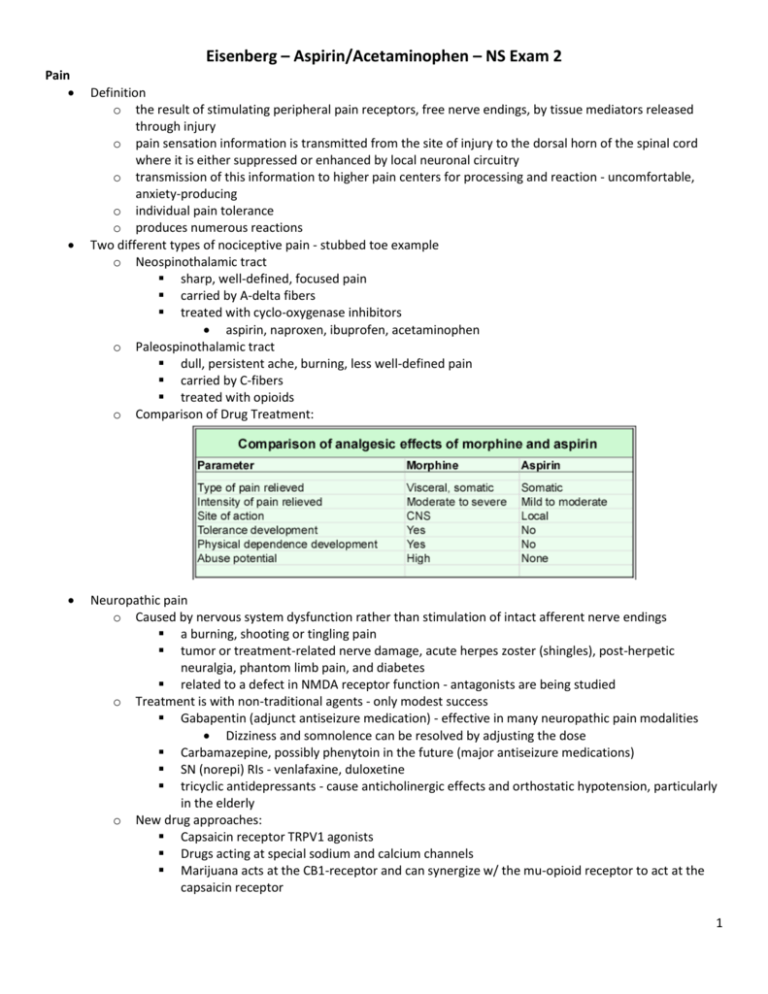
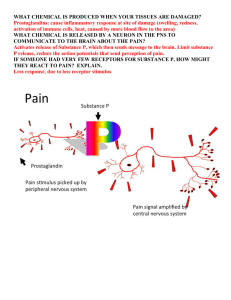
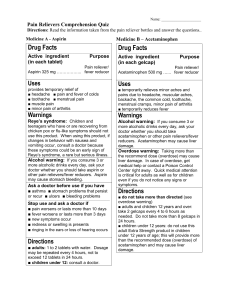
Eisenberg – Aspirin/Acetaminophen – NS Exam 2 Pain Definition o the result of stimulating peripheral pain receptors, free nerve endings, by tissue mediators released through injury o pain sensation information is transmitted from the site of injury to the dorsal horn of the spinal cord where it is either suppressed or enhanced by local neuronal circuitry o transmission of this information to higher pain centers for processing and reaction - uncomfortable, anxiety-producing o individual pain tolerance o produces numerous reactions Two different types of nociceptive pain - stubbed toe example o Neospinothalamic tract sharp, well-defined, focused pain carried by A-delta fibers treated with cyclo-oxygenase inhibitors aspirin, naproxen, ibuprofen, acetaminophen o Paleospinothalamic tract dull, persistent ache, burning, less well-defined pain carried by C-fibers treated with opioids o Comparison of Drug Treatment: Neuropathic pain o Caused by nervous system dysfunction rather than stimulation of intact afferent nerve endings a burning, shooting or tingling pain tumor or treatment-related nerve damage, acute herpes zoster (shingles), post-herpetic neuralgia, phantom limb pain, and diabetes related to a defect in NMDA receptor function - antagonists are being studied o Treatment is with non-traditional agents - only modest success Gabapentin (adjunct antiseizure medication) - effective in many neuropathic pain modalities Dizziness and somnolence can be resolved by adjusting the dose Carbamazepine, possibly phenytoin in the future (major antiseizure medications) SN (norepi) RIs - venlafaxine, duloxetine tricyclic antidepressants - cause anticholinergic effects and orthostatic hypotension, particularly in the elderly o New drug approaches: Capsaicin receptor TRPV1 agonists Drugs acting at special sodium and calcium channels Marijuana acts at the CB1-receptor and can synergize w/ the mu-opioid receptor to act at the capsaicin receptor 1 Salicylates - Aspirin History and current uses o Analgesia o Anti-inflammatory and antirheumatoid effect o Antipyretic effect – lower fever o Anticoagulant effect Activity is through the action of salycyclic acid which is freed Pharmacologic effects o Analgesia - treatment of pain Prostaglandins are products of cyclo-oxygenase(s) conversion of arachidonic acid maintains the sensitivity of the peripheral pain receptors COX-1 (ubiquitous) appears to exist in most tissues and is involved in homeostasis COX-2 is induced when inflammatory cells are activated; exists constitutively in brain and kidney Aspirin, acetaminophen, and other NSAIDS act to suppress both enzymes. The suppression of COX-1 often results in the disruption of its protective properties (i.e., gastric mucosa). Newer agents are available with more COX-2 selective antagonism. o Anti-inflammatory - antirheumatoid effect Maintains capillary wall integrity - reduces edema Inhibits the release of chemotactic factors which mobilize neutrophils to the site of injury/ inflammation Stabilizes lysosomes - prevents release of proteases (that cause tissue injury during inflamm) Inhibits the formation of oxygen-derived free radicals Largely replaced by ibuprofen and naproxen o Antipyretic effect COX inhibition in the central nervous system Inhibition of interleukin-1 (released from macrophages) o Anticoagulant effect Decreased adhesiveness of platelets irreversibly inhibits platelet COX Decrease in prothrombin level Absorption, metabolism & excretion Rapid absorption after oral administration o part from the stomach - low pH, un-ionized from o most from the small intestine because of the larger surface area - even though higher pH, less is in the un-ionized form First conversion is to free salicylic acid Excretion by glomerular filtration and tubular secretion o alkalinization of the urine will prevent reabsorption - more drug in the ionized form o increasing urine volume reduces the absorption of un-ionized drug o tubular secretion is an active process Side/toxic effects Data for a typical year – ER contacts (ODs) o aspirin alone: 16,640 o aspirin/codeine: 5,443 o deaths: 50 CNS effects o stimulation followed by depression: confusion, dizziness, tinnitus, then delirium, psychosis, stupor and coma o nausea and vomiting - CTZ stimulation - dopaminergic 2 GI problems o gastric upset, aggravation of peptic ulcer, gastritis probably due to COX-1 inhibition Celecoxib (Celebrex) and rofecoxib (Vioxx), COX-2 inhibitors, show less upset increase fluid intake formulations with better solubility enteric coating may cause erratic absorption o gastric bleeding - usually not clinically significant Respiration and acid-base balance o Phase I – low level OD Respiration rate by direct action on medulla Uncoupling of oxidative phosphorylation increases CO2 formation which indirectly stimulates respiration; the increased metabolism increases body temperature blow off CO2 H2CO3 decreases respiratory alkalosis o Phase II – high level OD Respiration rate decreases by direct action on the medulla conserve CO2 H2CO3 increases respiratory acidosis neurogenic drive, pCO2, pO2 Effects on other systems o Increased metabolic rate increase in body temperature metabolic acidosis- pyruvic & lactic acid, sulfates & phosphates build up o Renal renal failure in patients with renal insufficiency overdose may cause acute tubular necrosis o Cardiovascular peripheral vasodilation (direct action) toxic doses depress central vasomotor centers Treatment approaches o Activated charcoal to reduce GI absorption o Alkalinize by giving bicarbonate regain proper acid-base balance aids excretion of weak acids ionizes salicylic acid reducing CNS entry o Lower body temperature by mechanical means o Fluids for replacement and to aid excretion o Supportive measures Interactions/precautions Displaces thyroid hormones and corticosteroids from plasma proteins Often given in combination with opioids Precautions in some patients o peptic ulcer, gastritis – COX-1 inhibition o blood coagulation disorders o allergies Reye’s syndrome in children o encephalopathy and hepatic injury o causal relationship is now in question o aspirin is still avoided in children 3 Review of therapy: Proven uses o analgesia o antipyretic action o inflammation o anticoagulation Proven or suggested uses o prevention of heart attacks and strokes o maintaining coronary bypass graft patency o reducing deaths from acute heart attacks o treating hypertension (toxemia) of pregnancy o preventing clots on artificial heart valves o reducing recurrences of migraine o strengthening immunity o prevention of colon cancer Acetaminophen (Tylenol): Pharmacologic effects Analgesia, antipyresis No anti-inflammatory and antirheumatic properties o inhibits cyclogenases in the brain but not at sites of inflammation in peripheral tissues Higher doses can produce sedation and euphoria Added benefits Little gastric erosion no anticoagulant effect no change in acid-base balance Does not interfere with the uricosuric effects of agents to treat gout No problem with Reye's Syndrome Side/toxic effects Acetaminophen toxicity - 50,000 ER visits annually The most common drug taken in overdose Liver - occurs 24-48 hours after overdose o hepatic lesions occur with overdose o formation of a toxic intermediate N-acetyl-p-benzoquinone imine(NAPQI) causing cell death inactivated by glutathione o cysteine or cysteamine is the specific treatment to increase glutathione o alcoholics are at special risk existing hepatic problems require more acetaminophen because it is metabolized faster - cytochrome p450 is induced dietary deficiencies reduce existing glutathione Kidney o “phenacetin nephritis” with chronic use/abuse o preliminary studies suggest that this does not occur with acetaminophen o there are reports of renal damage without hepatic damage - 8% of new dialysis patients were taking at least one dose of acetaminophen per day Blood o cyanosis, particularly with phenacetin, though rare with acetaminophen o sulfhemoglobinemia o hemolytic anemia Review of therapeutic uses Analgesia Antipyretic effect No anti-inflammatory action 4