outline3294
advertisement

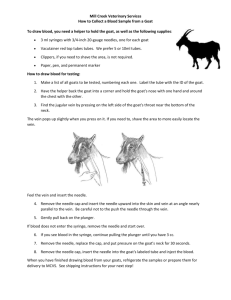
Outline Station 1: 1. Supplies A. Sodium fluorescein (5cc of 10% concentration, 2cc of 25% concentration) B. 5cc syringe with 23-gauge butterfly tubing infusion set C. Alcohol pads D. Band-Aids, tape E. Gauze pads (2 x 2) F. Tourniquets 1. Rubber tubing for most patients; works best for large arms 2. Velcro type works best for children or hairy arms G. Disposable latex gloves H. Sharps container for needle disposal I. Ice packs (if infiltration occurs) J. Emesis basin 2. Contraindications A. Pregnancy and nursing mothers B. Known hypersensitivity from previous angiography procedures C. Extreme apprehension D. When diagnosis and treatment are obvious 3. Legal Consent Form A. Make sure the patient is aware of what the procedure is and what is about to take place B. Have patient sign consent form (preferably before eyes are dilated) C. Tell patient that their skin will be yellow for 1-2 hours and their urine will be bright yellow for 1-2 days Station 2: 1. Venipuncture A. The procedure for entering a vein with a needle or catheter B. Purpose 1. To draw blood from a donor or for laboratory testing 2. To administer fluids such as nutrients, drug and contrast mediums (such as sodium fluorescein) 3. To maintain an open vein in case of emergency C. Considerations for vein selection 1. Availability of sites, number of veins visible 2. Size of needle 3. Frequency of venipuncture required by the patient D. Selection of vein 1. Antecubital vein preferred because it is large, readily accessible, and well supported by connective and muscular tissue 2. Veins on the back of the hand are poorly supported causing them to roll easily and injection here is more painful because the skin is thinner and more sensitive 3. Choose large veins that can accept a good size needle and choose sites distal to venous junctions E. Needle insertion techniques 1. When vein is prominent, needle is inserted directly into the vein at a 30 to 45 angle 2. When a vein is small, the needle can be inserted slightly to one side of the vein and then directed into the vein about ½ inch beyond the injection site 3. Bevel-Up a. Causes less trauma to the vein b. Usually less discomfort for the patient c. If needle and vein have approximately the same diameter, the bevel-up position is more likely to cause perforation of the vein 4. Bevel-Down a. Used when entering a relatively small vein with a large needle b. Less likelihood of blockage of bevel should the vein collapse upon removing the tourniquet 2. Simulator Arms A. Composed of synthetic skin and self-sealing veins that simulate the human arm B. Set-up for intravenous injection: 1. Use distilled water as a substitute for alcohol/injectable medications 2. Fill a 3cc syringe with colored distilled water to simulate fluorescein 3. Apply tourniquet to upper arm 4. Insert butterfly needle into antecubital vein 5. Open cap to allow “blood” to flow back through tubing 6. Attach syringe to the end of tubing 7. Remove tourniquet 8. Push bolus of fluorescein into vein at a rate of 1cc/sec 9. Repeat on vein on back of hand but tie tourniquet around wrist Station 3: 1. Emergency Supplies A. Oxygen B. Smelling salts C. Epinephrine (0.3mg for IM injection, EpiPen) D. Diphenhydramine tablets (25mg or 50mg tablets Benadryl) E. Sphygmomanometer and stethoscope F. Airway device 2. Complications of venipuncture and fluorescein angiography A. Extravasation of blood (hematoma) into surrounding tissue from piercing of posterior wall of the vein or insufficient pressure at injection site after withdrawing the needle 1. Tx: apply pressure to injection site after needle withdrawal B. Infiltration of dye into surrounding extravascular tissue from needle dislodgment during injection, perforation of vein wall, or burst vein from too rapid injection into a small vein 1. Tx: ice pack to injection site C. Nausea or vomiting 1. Tx: reassurance and have patient take several deep breaths, nausea usually passes quickly 2. Cool damp towel to forehead 3. For patients with known hypersensitivity from a previous reaction to fluorescein injection give 12.5mg promethazine (Phenergan) or 25-50mg diphenhydramine (Benadryl) p.o. 1 hour prior to procedure D. Urticaria (hives) and Pruritus (itching) 1. Tx: systemic administration of antihistamine (Benadryl 25-50mg p.o) 2. Severe hives and itching may require IM administration of epinephrine (0.3mg in EpiPen for adults or 0.15mg in EpiPen Jr. for children) 3. Monitor patient’s breathing pattern as this can precede anaphylactic shock 4. Use epinephrine subcutaneously for bronchodilation if needed (0.2-0.5mg, then every 20min to 4hrs as needed) E. Syncope (loss of consciousness) 1. Usually a vasovagal response 2. Tx: place patient in a supine position with legs elevated 3. Cool moist towel to forehead 4. Smelling salts 5. Give reassurance, consider hypoglycemia in diabetic patients F. Anaphylactic shock 1. Monitor and maintain airway 2. Tx: administer oxygen if necessary, epinephrine HCL 1:1000 0.2-0.5ml subcutaneously or IM with EpiPen 3. CPR if necessary 3. OSHA Standards/Universal Precautions A. The OSHA Standards requires physicians to offer the hepatitis B vaccination series to all medical personnel who have occupational exposure to blood, blood by-products, and certain body fluids B. All human blood and certain body fluids should be treated as if known to be infectious for HIV, HBV, and other blood borne pathogens C. Bandage cuts and other lesions on the hands before gloving D. Wash hands as soon as possible after removing gloves E. Do not bend, break, or shear contaminated needles (OSHA:1910.1030.d.2.vii) F. Place contaminated sharps in a puncture-resistant, leak proof container (OSHA:1090.1030.d.4iii.A.i) 4. Set-up for intramuscular injection (EpiPen): A. DO NOT INJECT ANY SUBSTANCE INTO SIMULATOR ARM MUSCLE B. Attach a 25 gauge needle onto a 5cc syringe C. Insert needle into deltoid area of arm D. Pull back on plunger to check for a “flashback” of blood (intramuscular injection) E. Inject into the deltoid