Resident Version
advertisement
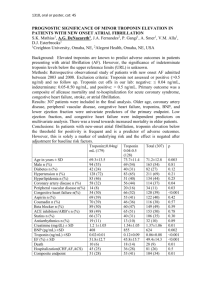
Resident Version Congestive Heart Failure Module Created by Dr. Cody S. Deen Objectives: 1. Identify history and physical exam findings consistent with Congestive Heart Failure. 2. Understand the utility of BNP for the internist. 3. Understand the different classification schemes of congestive heart failure. 3. Identify the workup and differential diagnosis of Congestive Heart Failure. 4. Identify potential complications from Congestive Heart Failure. 5. Identify medical treatments for the patient with Congestive Heart Failure. 6. Identify non-medical treatments for the patient with Congestive Heart Failure. References: 1. Crawford, Peter A. The Washington Manual Subspecialty Consult Series Cardiology Subspecialty Consult. 2004. 2. Jessup, Merriel and Susan Brozena. “Congestive Heart Failure.” NEJM (May 15, 2003. 248:2007-18.) 3. www.uptodate.com “Overview of the therapy of heart failure due to systolic dysfunction”. Wilson S Colucci, MD. Accessed on December 2007. CASE 49 year old male presents to the Emergency Department with a complaint of SOB. Patient reports that his breathing has gotten progressively worse over the last 2 months and is especially difficult when he is trying to sleep at night. He has several episodes of waking up gasping for air and is only able to fall asleep when he is sitting upright. The patient reports that he currently has SOB after walking 20 feet. Patient has only minimal white sputum. He denies fever, chills, green sputum, and sick contacts but does affirm bilateral lower extremity swelling. Social history is significant for a 60 pack year tobacco history, rare alcohol use and currently living in his van. Patient reports that his father had heart bypass surgery in his 60s. Currently, the patient has not seen a doctor in 30 years and takes no medications. Physical Exam is significant for HR=98, BP= 165/100, afebrile, RR=22 and sat= 85%RA, wt =198#. Lung exam reveals decreased breath sounds throughout and bilateral crackles at the bases, CV exam reveal an enlarged laterally displaced PMI, with a normal S1 and S2, +S3 and no murmurs. Extremities show 2-3+ pitting edema to mid-thigh bilaterally. CXR reveals bilateral small pleural effusion, and prominent pulmonary vasculature. 1. What is the likely diagnosis and what additional testing and labs would you want? 2. What class of congestive heart failure is this patient demonstrating? 3. What is the utility of BNP for diagnosing heart failure in this patient? 4. Are there other utilities of BNP in patients with congestive heart failure? Further Patient Information The patient undergoes ECG, as well as recommended screening labs. ECG reveals sinus tachycardia, LVH and q waves in V1-V4. Labs are significant for sodium of 128, a BUN of 45 a creatinine of 1.9, and a random glucose of 245. UA, LFTs, and TSH are all within normal limits. Lipid Panel reveals total cholesterol of 250, HDL of 24, and LDL of 169. Urine electrolytes ordered for elevated creatinine suggest pre-renal azotemia (FENa <1%). Echocardiogram reveals an Ejection Fraction (EF) of 35-40%, left ventricular hypertrophy, septal and anterior wall hypokinesis, normal valves, and elevated pulmonary artery and right atrial pressures. 5. What is the most likely etiology of his congestive heart failure based on this information? 6. What are additional potential causes of Congestive Heart Failure? 7. What is the next diagnostic step in evaluating this patient? The patient however is unable to lay flat and thus you must improve his symptoms before he can undergo cardiac catherization. You want to treat his heart failure but are unsure about giving a patient lasix with pre-renal azotemia. 8. What are the common physiological derangements of congestive heart failure? 9. What is the initial management of heart failure? You fluid and salt restrict the patient, requesting daily weights and strict ins and outs. You decide that by reducing the preload of the patient (with diuretics) you may effectively shorten the sarcomere length back to an ideal relationship which will allow more force to be generated during contraction thus increasing cardiac contractility and cardiac output. You give the patient 40mg of IV lasix and are pleased with his 24 hour net loss of ~2L. Repeat creatinine is 1.6 and the patient feels much better. 10. You also decide to improve his afterload by treating his blood pressure what antihypertensive would you use? 11. Which other medications have been shown to have a mortality benefit in congestive heart failure and in what setting should they be considered? After 6 days of diuresis and afterload reduction with ACE-I your patient has lost 15 pounds and is able to walk the hallway of 7 South without oxygen or SOB. You add a beta blocker to his ACE-I, ASA, and statin. The patient undergoes catherization which shows severe 3 vessel disease and he is scheduled for 3-vessel CABG later that week. He does well and you don’t see him for several years. He presents to the ED ten years later and is on maximal medical therapy (maximum ACE-I, maximum Beta blocker, aldactone 40 mg, lasix 200 mg daily, asa, statin. He has undergone an additional CABG three years prior). Currently he has SOB at all times including while resting in an upright position. His EF now is 15-20%. 12. What additional non-medical therapies should be considered at this time? Discussion Outline: Heart failure work up: American College of Cardiology class I indications for the workup of heart failure include a basic metabolic panel, urinalysis, fasting glucose, lipid panel, TSH, liver function tests, and a CBC. Additionally a twelve lead ECG along with Chest x-ray and Echocardiogram should also be performed. Cardiac Catherization should be performed in any patient who has history of angina or evidence of ischemia. ?BNP. New York Heart Classification of Congestive Heart Failure Classes Class I - symptoms of HF only at activity levels that would limit normal individuals Class II - symptoms of HF with ordinary exertion Class III - symptoms of HF with less than ordinary exertion Class IV - symptoms of HF at rest Utility of BNP for diagnosing heart failure: Brain Natriuretic Peptide’s utility to diagnose congestive heart failure has been evaluated in the Breathing Not Properly Study. This study examined 1586 patients with a complaint of acute dyspnea Approximately 47% of patients enrolled had congestive heart failure and were found to have a mean BNP of 675 pg/ml compared to the group without congestive heart failure who had a mean of 110 pg/ml. Setting a normal value at 100pg/ml, the BNP had a sensitivity of 90%, a specificity of 76%, and a positive predictive value of 83%. The negative predictive value of BNP has been shown to be between 90 and 97% in multiple studies. This finding suggests that the greatest utility of a BNP may be in its ability to exclude congestive heart failure as a cause of acute dyspnea. Mortality rates associated with BNP levels suggest that patient’s with extremely high elevations in BNP may have higher risk of death during hospitalization than those with only moderately elevated BNP. Patients with BNP levels of 480- 839 pg/ml have been reported to have a 2.8% in hospital mortality compared to a 6% hospital mortality in patients with a value > 1739pg/ml Causes of Congestive Heart Failure: Causes of CHF can be divided into Diastolic Dysfunction and Systolic Dysfunction. Common causes of Systolic Dysfunction include CAD, HTN, Diabetes/ small vessel disease, valvular heart disease, toxins (ethanol, methamphetamine, cocaine, doxorubicin), infectious (coxsackie virus) and thyroid abnormalities. Common causes of Diastolic Dysfunction include HTN, hypertrophic cardiomyopathy, restrictive cardiomyopathy (amyloidosis, sarcoidosis, hemachromatosis), and constrictive pericarditis. Common physiological derangements of congestive heart failure: - Pre-renal azotemia- due to poor cardiac output and compensatory elevation in systemic vascular resistance. - Confusion and lethargy- due to poor cardiac output and compensatory elevation in systemic vascular resistance producing decreased cerebral perfusion - Exercise intolerance. - Hepatic Congestion with mild transaminitis, mild derangements in clotting, and elevated bilirubin- due to hepatic congestion from elevated right sided heart pressure. -Lower extremity edema and elevated jugular venous distention- from elevated right sided heart pressure -Pulmonary edema- due to elevated left ventricular end diastolic pressures (LVEDP) -Orthopnea, PND, pleural effusion, lower extremity edema, elevated neck veinsfrom pulmonary edema and elevated LVEDP. Management of heart failure: Initial management includes fluid restriction at 1.5cc/day, sodium restriction at 2 grams of salt per day, appropriate treatment of blood pressure (afterload reduction) with a goal <130/80, oxygen to improve oxygen delivery, and diuresis (preload reduction). Medications used in CHF and its benefits: Beta blockers- carvedilol and metoprolol have both been shown to have improvement in mortality for congestive heart failure patients. There may be some evidence that carvedilol is superior to metoprolol in severe heart failure patients (COMET trial). Usually initiated and up titrated after patient has improved to class II symptoms. Angiotensin receptor blockers/ ACE-I- Have been shown to improve mortality. Does not tend to worsen azotemia if started at low dose and slowly titrated. Usually initiated after diuretic therapy in acute heart failure. Aldactone- for patients with class III or class IV CHF and already on loop diuretics and ACE-I therapy, the RALES trial showed 30% mortality reduction at 24 months for spironolactone treated group. Hydralazine and Nitrates- A-HEFT demonstrated a mortality benefit in AfricanAmerican patients put on a combination of hydralazine plus nitrates. Previous studies had shown reduced benefit of ACE-I in African-American CHF patients. Data has been extrapolated to patients unable to tolerate ACE-I or ARB for CKD. ASA- only beneficial in patient with CAD Statins- observational and retrospective studies indicate there may be a benefit for nonischemic heart failure for lowering admission rates due to CHF exacerbations. One post hoc analysis showed decreased rate of arrhythmic deaths and overall mortality with stating therapy in non-ischemic cardiomyopathy. Digoxin- no mortality benefit, but it does improve symptoms and decreases admissions for CHF exacerbations Additional therapies to be considered: Biventricular Pacemaker- CARE-HF trial showed a modest mortality benefit and symptomatic improvement in patients with EF<35%, Class III or IV CHF and QRS>120ms. Cardiac Transplant Hospice Post Module Evaluation Please place completed evaluation in an interdepartmental mail envelope and address to Dr. Wendy Gerstein, Department of Medicine, VAMC (111). 1) Topic of module:__________________________ 2) On a scale of 1-5, how effective was this module for learning this topic? _________ (1= not effective at all, 5 = extremely effective) 3) Were there any obvious errors, confusing data, or omissions? Please list/comment below: ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ 4) Was the attending involved in the teaching of this module? Yes/no (please circle). 5) Please provide any further comments/feedback about this module, or the inpatient curriculum in general: 6) Please circle one: Attending Resident (R2/R3) Intern Medical student