May 2014 - Colorado Perinatal Care Quality Collaborative (CPCQC)
advertisement

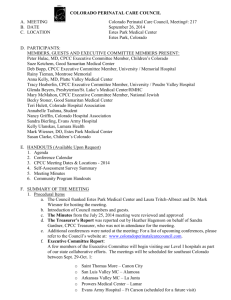
COLORADO PERINATAL CARE COUNCIL A. MEETING B. DATE C. LOCATION Colorado Perinatal Care Council, Meeting#: 215 May 16, 2014 Parkview Medical Center Pueblo, Colorado D. PARTICIPANTS: MEMBERS, GUESTS AND EXECUTIVE COMMITTEE MEMBERS PRESENT: Steve Holt, MD, Rose Medical Center, CPCC Chairman Judy Smith, Heart of the Rockies Regional Medical Center Deb Bopp, Memorial Hospital, University South Courtney Cryer, Montrose Memorial Carri Montgomery, Platte Valley Medical Center Sally Garcia, St. Anthony North Paulette Mapes, St. Mary Corwin Natasha Mondragon, Nurse Family Partnership Susan Clarke, Children's Hospital Colorado Elizabeth Whitley, MD, CDPHE Kirk Bol, CDPHE Lisa McCullough, Parkview Medical Center Jenny Lowenfish, Memorial Star Transport Stefanie Leonard, Children's Hospital Colorado Flight for Life Amber Breyfogle, Flight for Life Colorado Susan Wilczynski, St. Mary Corwin Maria Telfer, St. Mary Corwin Georgia Gardner, Nurse Family Partnership E. HANDOUTS (Available Upon Request) 1. Agenda 2. Conference Calendar 3. CPCC Meeting Dates & Locations - 2014 4. Self-Assessment Survey Summary 5. Meeting Minutes 6. Community Program Handouts F. SUMMARY OF THE MEETING 1. Procedural Items a. The Council thanked Pat Pate for hosting the meeting and providing the meeting room, snacks and refreshments. b. Introduction of Council members and guests. c. The Minutes from the March 21, 2014 meeting were reviewed and approved d. The Treasurer’s Report was provided by Sandra Gardner, CPCC Treasurer. e. Additional conferences were noted at the meeting: For a list of upcoming conferences, please refer to the Council’s website at: www.coloradoperinatalcarecouncil.com. f. Executive Committee Report: CPCC Executive Committee is looking at our current structure and continuing to define the visions and goals of CPCC for the future. We would like to focus on more state collaborative efforts and establish more key partnerships. CPCC Exec Committee is still looking for a new Chairman Elect. Dr. Liz Whitley (CDPHE) and Dr. Rachel Wright (Neonatologist, Denver Health) have now joined the Executive Committee. Pat Bohling-Smith and Vicki Lemmon have both resigned their roles on the Executive Committee, so we will be looking for a new Executive Committee member. The Executive Committee is currently working on the upcoming agenda for the July 2014 meeting. Topics will include: Marijuana - Laura Borgelt will be presenting o CPCC is considering creating a task force or sub-committee to address this issue in our state. More details to come regarding the structure of this. o We are collecting Marijuana policies/guidelines that are currently out there in your hospitals. Please forward to Heather any that you have that you are willing to share. Quality initiatives in Colorado - Paco will present o CPCC is looking at additional funding and grant opportunities to continue the state collaborative initiatives. o Presentation about what other states are doing re: quality care collaboratives and what/how Colorado is doing Accountable care update - are there any access issues for mothers and babies Other CDPHE updates, including Legislative Updates If you have any agenda topics you would like Exec Committee to consider for future meetings, please email Heather The Executive Committee is also continue to strategize about providing outreach to smaller community hospitals and working on establishing a system to reach out to Level I and II hospitals to increase meeting participation through webinars and conference calls. CPCC has defined the first wave of hospitals to reach out to: o Saint Thomas More – Canon City o San Luis Valley MC – Alamosa o Arkansas Valley MC – La Junta o Prowers Medical Center – Lamar o Evans Army Hospital – Ft Carson CPCC has received a grant through CDPHE to visit their sites. The purpose of the CPCC visit is to introduce the work of the council, become acquainted with their regional providers, and to share data specific to their regions with comparative data from regions throughout the state. Representatives from the council, which include Maternal-Fetal Medicine, Obstetrics, NurseMidwifery and a Maternal Health Specialist from the CDPHE, would like to visit their facilities in person this summer. CDPHE Maternal Mortality Review Committee Members who are interested in joining CPCC on these site visits are: Kent Heyborne, MD Amy Nacht, MSN, CNM Jessica Anderson, MSN, CNM, WHNP-BC Torri Metz, MD CPCC has also requested an additional grant from March of Dimes to provide formal outreach initiatives in this area as well. g. Website Update: Please visit www.cpcc.co. Please contact Heather Hagenson if you have any ideas or resources that can be added to the website. h. Conference Calendar: Please send Heather any 2014 conferences from your organization or in your community The following summaries are from the presentations from the May 16, 2014 meeting: I. Parkview Medical Center Perinatal Services Update Parkview presented general information regarding the perinatal services that they offer, including their successful journey to changing their neonatal level of care. II. Maternal Stabilization and Transport: Decision Making Process Presented by: Stephanie Martin, DO, Southern Colorado Maternal-Fetal Medicine Dr. Martin began her presentation by discussing the goals of maternal transport and reviewed that it's best to avoid a neonatal transport, and transfer the mother to the facility best equipped to meet her and the neonates needs. She reviewed that the Healthy People 2010 goal is 90% of Very Low Birth Weight Babies (VLBW) should be born in high-risk facility. She shared national statistics regarding VLBW babies and discussed that there are wide variations of these statistics among states. Dr. Martin discussed the Maternal Child Health (MCH) National Performance Measure 17 which evaluates the number of VLBW neonates born in high-risk facility. Based on this data from 52 states and jurisdictions: 15 states essentially had unchanged rates 23 states had improved rates Average improvement 8% Colorado in this group 14 states showed lower rates 4 of these remained below the all-state rate of 75% VLBW inborn Average decline 9% Iowa had notable increase Dr. Martin reviewed the data from Colorado and shared that the rate has improved 8.9% overall from 2000-2008. The most recent rate (2008) shows that 80.5% of VLBW born in high-risk facility, while the 20% of babies not born in high-risk facility was due to being in urban areas where competition is high and neonatal transport is readily available. Dr. Martin also discussed the barriers to maternal transport and the regionalization of care and how EMTALA plays a role in these transfers as well. She reviewed the indications for maternal transfer, including other reasons for transfer such as complying with insurance contract requirements or when a pregnant woman seeks emergency care at a facility without obstetrical services. Dr. Martin also discussed the contraindications for maternal transfer. She identified the key components to a successful transfer: Good communication between the referring facility, transport team, and receiving facility. Written documentation or, ideally, recorded conversation with typed transcript. Timely response/arrival by the transport team Experienced and trained transport personnel to assess patient status and determine appropriateness of transport Ability to provide a rapid mode of transport to the receiving facility She then reviewed the different aspects of maternal transfers including mode of transport, documentation, communication between the transferring provider and the receiving facility and role responsibility. Dr. Martin also discussed the care provided to mothers in route and the required guidelines and certifications necessary for a maternal transport. Dr. Martin concluded her presentation by reviewing the important areas regarding maternal transports: Maternal transport should be considered if the facility does not have sufficient resources to meet maternal and/or neonatal medical needs Outcomes for premature neonates are improved if delivery occurs at an appropriate level facility versus neonatal transport to the appropriate facility The maternal transport should be coordinated between the transferring and receiving facility and the patient accompanied by appropriately trained medical personnel An understanding of, and compliance with, EMTALA guidelines and relevant state statutes is essential when transporting patients For a copy of this presentation, please contact Heather Hagenson at heather@coloradoperinatalcarecouncil.com III. Neonatal Stabilization and Transport: Decision Making Process Presented by: Mary Laird, MD, Pediatrix Medical Group, Colorado Springs, CO Dr. Laird began her presentation by reviewing the different aspects of neonatal transport. She reviewed the outcomes and statistics of VLBW babies after inter-facility transfers. She reviewed the different tasks that are required of the referring hospital staff once the neonatal transfer decision has been made. Dr. Laird outlined the preparation and stabilization steps necessary for the best outcomes. She reviewed a sample timeline, and shared the different flight times and ambulance drive times between the various Colorado hospitals in the southern region to Memorial Children's Hospital. Dr. Laird outlined that the transport mode requests will be collaborative between sending and receiving facilities and considerations include: What does the patient need? How quickly will the team reach the patient? Will the patient benefit from a reduced out-of-hospital time? Weather considerations? “Code 3” or “Lights and Sirens” Time saved vs. additional risk She shared information from a national conference from 2013 about pediatric and neonatal transports and the consensus conference paper that identified that time of delivery of definitive care is more important than the speed of transfer and will require a specialized team that is equipped to deliver definite care outside tertiary care centers. Adult air transport services and EMS crews are often not trained or equipped to deliver interventions for a pediatric or neonatal patient. Dr. Laird then discussed CAMTS. CAMTS is an organization of non-profit organizations dedicated to improving the quality and safety of medical transport services, with 20 current member organizations each of which sends one representative to the CAMTS Board of Directors. The Commission offers a program of voluntary evaluation of compliance with accreditation standards demonstrating the ability to deliver service of a specific quality. The Commission believes that the two highest priorities of an air medical or ground inter-facility transport service are patient care and safety of the transport environment. Dr. Laird reviewed the education and training that is required for this accreditation. She outlined the team composition and provided the credentials of the Memorial Star Neonatal Transport team. She identified the quality measures that are necessary for monitoring the care and operations of the service. Dr. Laird presented case reviews and shared that this is an important step in monitoring the service that they provide. At Memorial Children's, they have a multi-disciplinary, physician led case review process that has created an environment that is collaborative and not punitive in order to identify any challenges of neonatal transports. She concluded her presentation by providing a summary of the importan...These include: If VLBW infant must be born, better in tertiary care center Some VLBW babies will still be born in hospitals without level III/IV NICUs and preparation for this event is critical Care of infant at birth, prior to leaving birth hospital, and on transport is critical to outcomes Referring hospital and transporting/accepting hospital share responsibility Neonatal transport teams are made up of highly trained dedicated professionals supported by professional/accrediting organizations and their hospital For a copy of this presentation, please contact Heather Hagenson at heather@coloradoperinatalcarecouncil.com IV. Southern Colorado Data Update Presented by: Ed Donovan. MD, Neonatologist, CPCC Consultant Kirk Bol, MSPH, CDPHE Vital Statistics Unit – Health Statistics Section Kirk Bol and Dr. Donovan jointly presented the southern Colorado data. It was first presented that the data was analyzed from the Health Statistics and Evaluation Branch of CDPHE through birth certificates, death certificates, fetal death certificate (20+ wks gestation), linked birth/infant deaths and the PRAMS survey (Pregnancy Risk Assessment Monitoring System). They reviewed the relevant measures that accounted for each of the data sources. They reviewed the various data briefs (HealthWatch) areas that CDPHE is monitoring (for more information about this, go to: http://www.chd.dphe.state.co.us/topics.aspx?q=Health_Statistics_Publications). Dr. Donovan then reviewed the Colorado Perinatal Outcomes according to 7 different regions. He reviewed the data for each of these regions, in addition to Colorado as a whole, for antenatal steroids among births 24-34 weeks and prematurity (<37 weeks) for these areas as well. He offered questions and insight into the data and stressed the importance of continuing to review and monitor this data. A copy of the presentation can be found on the CPCC website at www.cpcc.co V. The meeting was adjourned. The next Council meeting is scheduled for July 25, 2014 at the Colorado Department of Public Health and Environment in Denver, CO from 9am – 12pm. Respectfully Submitted, Heather Hagenson, CPCC Coordinator