SODIUM: THE FORGOTTEN NUTRIENT

SODIUM: THE FORGOTTEN NUTRIENT
SSE #78 VOLUME 13 (2000), NUMBER 3
Michael F. Bergeron, Ph.D., FACSM
Georgia Prevention Institute
Department of Pediatrics
Medical College of Georgia
Augusta, Georgia
KEY POINTS
Athletes lose far more sodium and chloride in sweat than any other electrolytes.
Sodium and chloride losses are greater with higher sweating rates.
Sodium and chloride losses in sweat are usually less when an athlete is acclimatized to the heat.
To completely replace body fluids after exercise, an athlete must replace the sodium and chloride that were
lost through sweating.
Sodium deficits can lead to incomplete rehydration and muscle cramps.
Excessive rapid water consumption, combined with a large sweat-induced sodium deficit, can lead to hyponatremia, a potentially deadly reduction in blood levels of sodium.
INTRODUCTION
Many athletes know the following scenario all too well: It's hot and humid, and the game, match, or race has been going on for some time. Each athlete has been working hard and is very tired but feels that a win is within grasp.
Profuse sweating reminds the athletes to drink a lot at every opportunity - and they do. Then it happens. What began as only very subtle, hardly noticeable twitches in the legs has now evolved into completely debilitating, full-blown muscle cramps. The afflicted athlete can no longer continue competing and now, once again, must seek medical attention. What happened? And why do so many other athletes not have the same problem?
Most athletes appreciate the importance of drinking plenty of fluids and the benefits of staying well hydrated. Also, considerable research proves that inadequate hydration during exercise or sport activities can readily lead to a decrease in performance and an increased risk for heat illness (Gonzalez-Alonso et al., 1997; Hargreaves &
Febbraio, 1998; Sawka, 1992; Sawka et al., 1998). Moreover, various associations have published comprehensive position statements that emphasize the importance of hydration during activity (American Academy of Pediatrics,
2000; American College of Sports Medicine, 1996; National Athletic Trainers Association, 2000). Yet, for many athletes, regular and copious water intake is not enough, in part because extensive sweating can lead to an extraordinary sodium deficit as well as a large water deficit. Thus, appropriate sodium and chloride (salt) intake should be an integral part of any rehydration plan. The importance of ingesting fluid, carbohydrate, and salt during prolonged exercise is well recognized and is underscored here as well, but the primary emphasis in this article is on rehydration after competition or a training session, especially in hot environments and particularly in those athletes who sweat profusely, lose excessive amounts of sodium in their sweat, are susceptible to heat cramps and other types of heat illness, and must train or compete again soon.
RESEARCH REVIEW
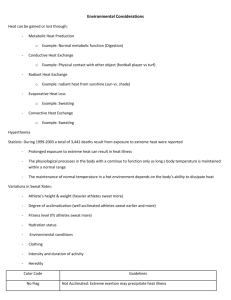
Sweat Losses and Rehydration
In warm to hot conditions, most adult athletes lose between 1 and 2.5 liters of sweat during each hour of intense competition or training. Notably, sweat rates over 3.5 liters per hour have been observed with some well-conditioned, world-class athletes who were competing in very hot and humid climates (Armstrong et al., 1986). Consequently, during a long race, match, game, or training session, it would not be difficult for many athletes to lose 10 liters of fluid or more. The degree to which one sweats depends on a number of factors, including the environmental heat stress
(i.e., temperature, humidity, and solar radiation), intensity of exercise, heat acclimatization status, and cardiorespiratory fitness. An increase in any one of these factors tends to prompt greater sweating.
Sweat is, of course, mostly water, but it also contains a number of minerals in varying concentrations (Costill, 1977).
As with fluid losses, several factors dictate the varied concentration of minerals in sweat, but most people lose far more sodium and chloride than any other electrolytes. Well-conditioned athletes who are fully acclimatized to the heat often have sweat sodium concentrations in the range of 5 to 30 millimoles per liter (i.e., 115-690 milligrams of sodium per liter of sweat) (Wenger, 1988). On the other hand, athletes who are not acclimatized to the heat typically lose much more sodium from a given volume of sweating (e.g., 40-100 millimoles or 920-2300 milligrams per liter).
However, some athletes can have relatively high concentrations of sodium in their sweat, no matter how fit or heat acclimatized they are, which suggests a strong genetic influence. Sweat sodium and chloride concentrations also vary with sweating rate (Wenger, 1988). As sweating rate goes up, the concentrations of these minerals in sweat usually increase as well. Again, given the impressive sweat losses that athletes often incur, it is not difficult to imagine that a sizable sodium deficit could readily develop, especially if the athlete follows a low-salt diet (e.g.,
<2,500 mg of sodium intake per day). For example, a sweat sodium loss of 2,500 to 5,000 milligrams per hour is common among many athletes with high sweating rates (e.g., 2.5 liters per hour). Over an extended match, race, or training session, this could readily translate into a 15-30% deficit in the total body exchangeable sodium, i.e., the sodium that is available for metabolism and fluid balance!
Unfortunately, it can be difficult (and often impossible) to keep up with heavy sweat losses by drinking fluids during training and competition. Consequently, rehydration after exercise often presents the athlete with a challenge as well, particularly if the athlete must compete again soon, such as during a tennis tournament. Importantly, to completely rehydrate after exercise, one must ingest more fluid (i.e., ~150%) than what is lost as sweat (as indicated by loss of body weight during exercise) because some fluid continues to be lost through urine formation during the rehydration period (Shirreffs & Maughan, 2000). However, as emphasized below, effective and safe rehydration is not always managed by simply drinking a lot of water. Sodium must be replaced as well.
Heat Cramps
Heat-related muscle cramps (heat cramps) often occur during prolonged exercise when there has been profuse and repeated sweating. Such is often the case in a football game, a triathlon, cycling race, or tennis tournament, especially in the later stages of the event (Bergeron, 1996). To completely restore body fluids, the salt lost through sweating must be replenished as well as the water (Maughan et al., 1997; Nose et al., 1988). Otherwise, a progressive and significant deficit of body water and sodium can develop. If this happens, selected motor nerve endings might become hyperexcitable due to altered mechanical stresses on the nerve endings as well as changes in the surrounding concentrations of electrolytes (Jansen et al., 1990; Layzer, 1994), resulting in seemingly spontaneous muscle contractions (i.e., cramps). Importantly, a deficit in total body sodium is often not reflected in measurements of sodium concentration in blood serum or plasma (Vaamonde, 1982). During and immediately after exercise, serum sodium concentration might be normal or slightly elevated, owing to secretion of sweat that has a relatively low concentration of sodium, reduced sodium excretion by the kidneys, and only small reductions in plasma volume. Otherwise, even if serum sodium decreases somewhat, as soon as an athlete has a chance to rehydrate and replace electrolytes, the concentration of sodium in the blood is typically normalized quite rapidly. This explains why players who suffer cramps on the court or on the field often do not exhibit abnormal electrolytes in follow-up evaluations by physicians.
So why don't more athletes cramp when they exercise for a long time or compete in several events during the same day? The key seems to be related to individual differences in sodium balance. Those who are susceptible to (and are often afflicted by) heat cramps sweat considerably, lose an extensive amount of sodium and chloride through sweating, and typically have a relatively low (or at least inadequate) daily dietary salt intake (Bergeron, 1996; Kleiner,
1993). Deficiencies in other minerals, e.g., calcium, magnesium, and potassium, can also cause muscle cramps and various neuromotor problems (Benda, 1989; Eaton, 1989; Levin, 1993; Liu et al., 1983; Miles & Clarkson, 1994;
O'Toole et al., 1993-95; Stamford, 1993). But a lack of one or more of these minerals is typically not the culprit when an athlete has cramps in the heat. Insufficient conditioning and fatigue can cause a muscle cramp (Bentley, 1996;
Schwellnus et al., 1997; Williamson et al., 1993), but the cramp is usually localized, and passive stretching, massage, or icing can often resolve it. Such is not the case with heat cramps. Immediate fluid and salt intake (orally or intravenously) is necessary. Does this mean that all athletes should load up on salt? For many, extra salt intake is appropriate when competing or training in hot conditions or any time that sweating is expected to be extensive (see
Practical Applications and Guidelines below). For cramp-prone athletes, extra salt intake may well be a necessity.
Hyponatremia
Given the strong emphasis these days on fluid intake and the importance of adequate hydration, the concept of
"water intoxication" or "overhydration" might seem somewhat inconceivable to most athletes. Yet, it is possible to drink water at a faster rate than the kidneys can excrete it. As one example, a 17-year-old, nationally ranked tennis player who was experiencing heat cramps, nausea, and weakness after playing a 4-hour match in extreme heat
(>38ºC) followed the advice of tournament medical personnel and promptly ingested a considerable amount of water.
Back in his hotel room, he experienced a seizure and slipped into a coma. It took more than two days in the hospital before he recovered and his serum electrolytes were stabilized. The initial blood chemistry profile revealed a serum sodium level of 118 millimols per liter (normal range at rest: 136-145). Thus, he was classified as severely hyponatremic. Although hyponatremia, per se, implies only that there is a relative excess of water compared to sodium, this particular adolescent athlete also likely had a sweat-induced sodium deficit from playing the previous match. Subsequent testing in similar environmental conditions showed that this athlete had a high sweating rate
(~2.5 liters per hour) and an estimated sweat sodium loss of over 20,000 milligrams (50 grams of sodium chloride) during four hours of competitive tennis (Bergeron, unpublished observations). The precise mechanism underlying hyponatremia is somewhat unclear, but in sports it seems to be brought on by extensive sweating coincident with and/or followed by repeatedly ingesting low-sodium or sodium-free fluids (e.g., water) for several hours or more
(Armstrong et al., 1993; Barr et al., 1991; Hiller, 1989; Speedy et al., 1999; Vrijens & Rehrer, 1999). In the study reported by Vrijens and Rehrer (1999), the subjects ingested fluids to just match their sweat rates, so athletes need not drink excessive amounts of sodium-free beverages to become hyponatremic. Accordingly, hyponatremia can readily occur in a number of sports or exercise activities.
So how does an athlete avoid developing hyponatremia? It is important to recognize several potential predisposing factors. Those with greater than average sweating rates and extensive sweat sodium losses may be at high risk.
Such athletes are the ones most likely to develop a sodium deficit that is fostered by these characteristics in combination with an inappropriately low salt intake. However, excessive drinking of plain water (or other sodium-free fluids such as soft drinks) before, during, and after exercise may be the most important cause of hyponatremia. In addition, some have suggested that women may be more likely to develop symptomatic hyponatremia because they are smaller and have a greater potential for fluid retention and maintenance of body weight during long-term exercise
(Noakes, 1992; Speedy et al., 1999). Thus, to prevent hyponatremia, one should consume an appropriate amount of fluid (i.e., only enough to maintain or restore normal body hydration status or to minimize an exercise-induced fluid deficit) and adequate salt before, during, and after competition and training (see Practical Applications and
Guidelines below), particularly when competing or training for a long duration or multiple times on successive days in the heat.
Compared to marathons, triathlons, and other ultra-endurance events (Speedy et al., 1999), the reported incidence of hyponatremia in tennis, soccer, football, or other similar duration sports and activities is very low. However, a low reported incidence does not preclude its existence, and the case described above should not be considered unique.
Furthermore, the severity of hyponatremia covers a wide spectrum (Mulloy & Caruana, 1995; Vaamonde, 1982). With some mild cases of hyponatremia, an athlete might experience nothing more than fatigue, apathy, slight nausea, and
a headache. These symptoms are not uncommon during hot-weather events. Severe hyponatremia, leading to incoordination, confusion, and seizure, is a dangerous threat to any athlete - its seriousness and likelihood should not be underestimated.
PRACTICAL APPLICATIONS AND GUIDELINES
When an athlete competes or trains in a hot environment, maintaining fluid and sodium balance is a challenge. This is also true for laborers or military and service personnel (e.g., firefighters) who sweat considerably while working.
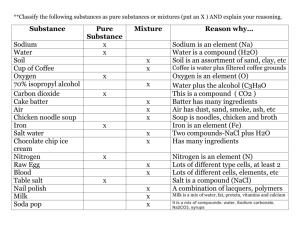
Simply adding salt to the diet (or eating high-salt foods) can help to prevent a sodium deficit and maintain or restore hydration. Even sports drinks and other beverages with a low concentration of sodium can help maintain a higher plasma sodium level (Vrijens & Rehrer, 1999). Examples of good sodium and chloride sources include the following:
Salt: 1/4 teaspoon (or 1.5 grams) has 590 mg of sodium.
Salted pretzels (483 mg sodium/stick)
Tomato juice (882 mg sodium/cup)
Sodium-containing sport drinks (e.g. Gatorade contains 110 mg sodium/8 oz)
Chicken noodle soup (1107 mg sodium/cup - 8 oz)
Tomato sauce (1481 mg sodium/cup)
Cheddar cheese/shredded (701 mg sodium/cup)
Pepperoni pizza (817 mg sodium/slice)
However, rather than just relying on salting foods or choosing salt-containing dietary items (which can lead to considerable uncertainty regarding how much salt is ingested), it is often more effective to follow a more specific plan.
For many serious athletes, this could involve consuming a selected volume of a salt-containing beverage such as a sports drink at regular intervals (e.g., 2-3 times a day), along with other fluids and foods throughout a training or competition period. Compared to drinking plain water, this ensures additional fluid intake and better fluid retention because of the salt content of the drink. When an athlete has to compete several times during the day and sweat losses are great, a sports drink should be consumed between events or matches in addition to an appropriate amount of other fluid and food that can be tolerated and rapidly digested. For those athletes who are especially prone to heat cramps, it may be helpful to add additional salt, e.g., 1/2 teaspoon/32 oz, to the sports drink; this is a convenient and reasonably palatable way to get at least an additional 1180 milligrams of sodium. For these people, salt pills work too, but it is important to have adequate fluid intake at the same time. Specifically, salt pills are likely to be more effective and better tolerated if the pills are ground up and mixed with an appropriate amount of fluid prior to consumption (e.g., 2-3 tablets per liter of fluid). Alternatively, using GatorLYTES™, a new prepackaged electrolyte mix, may be a more convenient and precise way to assemble an appropriately balanced and effective electrolyte solution to help prevent heat cramps from developing. Heavy sweaters, especially those prone to heat cramps, should also make a special effort to drink sodium-containing fluids during exercise and sports activities. For example, using GatorLYTES™ during play or adding a little salt to one's on-court sport drink (e.g., 1/4-1/2 teaspoon per 32 ounces) can be even more effectual in preventing heat cramps and maintaining sodium balance for these particular athletes.
Importantly, any plan for increasing dietary salt intake should include appropriate and adequate fluid intake. This point should not be under-emphasized. For years (and again recently by some athletic trainers and football programs) pickle juice consumption has been endorsed and promoted as effective in prevention and treatment of muscle cramps. Pickle juice has about the same sodium content as seawater (~500 mmol/liter). And while drinking a lot of pickle juice could certainly provide considerable sodium to one's diet, the associated distastefulness and intolerance of large quantities (i.e., more than several ounces) limits the amount of sodium that one can actually consume this way. More importantly, drinking small amounts of pickle juice does not provide the necessary amount of accompanying fluid that is required for effectively restoring fluid and electrolyte balance. Without adequate fluid intake, the athlete remains at risk for overheating and poorer performance.
Dietary methods for altering salt intake should be tested prior to a competition period so that the athlete becomes accustomed to the food and fluid selections and intake patterns and knows what to expect. Also, such a dietary plan should be individually designed. In other words, it is best to determine an athlete's specific rates of sweating and electrolyte losses under selected conditions so that a suitable and sufficient strategy can be implemented to ensure adequate rehydration and electrolyte balance. After all, a dietary plan to replace 2000 milligrams of sodium, for example, is going to be very different than one designed to offset a 15,000-milligram daily sodium deficit. For most people with normal blood pressure, even excessive salt intake will likely not pose a health threat (Taubes 1998) off the court or field. Thus, for the majority of healthy athletes, consuming more salt-containing fluids and food during periods of training or competition in the heat will at worst be harmless and may indeed enhance well being and performance.
SUMMARY
Large sweat losses often mean extensive sodium losses. Such sodium losses can result in incomplete rehydration and may predispose the athlete to heat cramps during subsequent exercise. Moreover, rehydration with sodium-free fluids such as water can lead to hyponatremia in certain individuals. Thus, any time considerable sweating occurs or is anticipated, appropriate fluid intake with an accompanying increase in dietary salt can help prevent problems related to a sweat-induced sodium deficit and incomplete or inappropriate rehydration.
REFERENCES
American Academy of Pediatrics (2000). Climatic Heat Stress and the Exercising Child and Adolescent. Pediatrics 106: 158-159.
American College of Sports Medicine (1996). Position stand on exercise and fluid replacement. Med. Sci. Sports Exerc. 28: i-vii.
Armstrong, L.E., R.W. Hubbard, B.H. Jones, and J.T. Daniels (1986). Preparing Alberto Salazar for the heat of the 1984 Olympic Marathon.
Physician Sportsmed. 14: 73-81.
Armstrong, L.E., W.C. Curtis, R.W. Hubbard, R.P. Francesconi, R. Moore, and E.W. Askew (1993). Symptomatic hyponatremia during prolonged exercise in heat. Med. Sci. Sports Exerc. 25: 543-549.
Barr, S.I., D.L. Costill, and W.J. Fink (1991). Fluid replacement during prolonged exercise: effects of water, saline, or no fluid. Med. Sci.
Sports Exerc. 23: 811-817.
Benda, C. (1989). Outwitting muscle cramps - is it possible? Physician Sportsmed. 17: 173-178.
Bentley S. (1996). Exercise-induced muscle cramp: proposed mechanisms and management. Sports Med. 21: 409-420.
Bergeron, M.F. (1996). Heat cramps during tennis: a case report. Int. J. Sport Nutr. 6: 62-68.
Costill, D.L. (1977). Sweating: its composition and effects on body fluids. Ann. N.Y. Acad. Sci. 301: 160-174.
Eaton, J.M. (1989). Is this really a muscle cramp? Postgrad. Med. 86: 227-232.
Gonzalez-Alonso, J., R. Mora-Rodriguez, P.R. Below, and E.F. Coyle (1997). Dehydration markedly impairs cardiovascular function in hyperthermic endurance athletes during exercise. J. Appl. Physiol. 82: 1229-1236.
Hargreaves, M., and M. Febbraio (1998). Limits to exercise performance in the heat. Int. J. Sports Med. 19: S115-S116.
Hiller, W.D.B. (1989). Dehydration and hyponatremia during triathlons. Med. Sci. Sports Exerc. 21: S219-S221.
Jansen, P.H.P., E.M.G. Joosten, and H.M. Vingerhoets (1990). Muscle cramp: main theories as to aetiology. Eur. Arch. Psychiatr. Neurol.
Sci. 239: 337-342.
Kleiner, S.M. (1993). Workouts worth their salt: replacing what you sweat away. Physician Sportsmed. 21: 25-26.
Layzer, R.B. (1994). The origin of muscle fasciculations and cramps. Muscle Nerve 17: 1243-1249.
Levin, S. (1993). Investigating the cause of muscle cramps. Physician Sportsmed. 21: 111-113.
Liu, L., Borowski, G., and L.I. Rose (1983). Hypomagnesemia in a tennis player. Physician Sportsmed. 11: 79-80.
Maughan, R.J., J.B. Leiper, and S.M. Shirreffs (1997). Factors influencing the restoration of fluid and electrolyte balance after exercise in the heat. Br. J. Sports Med. 31: 175-182.
Miles, M.P., and P.M. Clarkson (1994). Exercise-induced muscle pain, soreness, and cramps. J. Sports Med. Phys. Fit. 34: 203-216.
Mulloy, A.L., and R.J. Caruana (1995). Hyponatremic emergencies. Med. Clin. N. Amer. 79: 155-168.
National Athletic Trainers Association (2000). Position statement: fluid replacement for athletes. J. Athl. Train. 35: 212-224.
Nose, H., G.W. Mack, X. Shi, and E.R. Nadel (1988). Role of osmolality and plasma volume during rehydration in humans. J. Appl. Physiol.
65: 325-331.
Noakes, T.D. (1992). The hyponatremia of exercise. Int. J. Sport Nutr. 2: 205-228.
O'Toole, M.L., P.S. Douglas, R.H. Laird, and W.D.B. Hiller (1995). Fluid and electrolyte status in athletes receiving medical care at an ultradistance triathlon. Clin. J. Sport Med. 5: 116-122.
O'Toole, M.L., P.S. Douglas, C.M. Lebrun, R.H. Laird, T.K. Miller, G.C. Miller, and W.D.B. Hiller (1993). Magnesium in the treatment of exertional muscle cramps (abstract). Med. Sci. Sports Exerc. 25: S19.
O'Toole, M.L., C.M. Lebrun, R.H. Laird, J. James, B.N. Campaigne, P.S. Douglas, and W.D.B. Hiller (1994). Magnesium for athletes resistant to usual IV treatment (abstract). Med. Sci. Sports Exerc. 26: S205.
Sawka, M.N. (1992). Physiological consequences of hypohydration: exercise performance and thermoregulation. Med. Sci. Sports Exerc. 24:
657-670.
Sawka, M.N., W.A. Latzka, R.P. Matott, and S.J. Montain (1998). Hydration effects on temperature regulation. Int. J. Sports Med. 19: S108-
S110.
Schwellnus, M.P., E.W. Derman, and T.D.Noakes (1997). Aetiology of skeletal muscle 'cramps' during exercise: a novel hypothesis. J.
Sports Sci. 15: 277-285.
Shirreffs, S.M., and R.J. Maughan (2000). Rehydration and recovery of fluid balance after exercise. Exerc. Sport Sci. Rev., 28: 27-32.
Speedy, D.B., T.D. Noakes, I.R. Rogers, J.M. Thompson, R.G. Campbell, J.A. Kuttner, D.R. Boswell, S. Wright, and M. Hamlin (1999).
Hyponatremia in ultradistance athletes. Med. Sci. Sports Exerc. 31: 809-815.
Stamford, B. (1993). Muscle cramps: untying the knots. Physician Sportsmed. 21:115-116.
Taubes, G. (1998). The (political) science of salt. Science 281: 898-907.
Vaamonde, C.A. (1982). Sodium depletion. In: S. Papper (ed.) Sodium: Its Biological Significance. Boca Raton, FL: CRC Press, pp. 207-234.
Vrijens, D.M., and N.J. Rehrer, (1999). Sodium-free fluid ingestion decreases plasma sodium during exercise in the heat, J. Appl. Physiol.
86: 1847-1851.
Wenger, C.B. (1988). Human heat acclimatization, In: K.B. Pandolf, M.N. Sawka, and R.R. Gonzalez (eds.) Human Performance Physiology and Environmental Medicine at Terrestrial Extremes. Indianapolis, IN: Benchmark Press, pp. 153-197.
Williamson, S.L., R.W. Johnson, P.G. Hudkins, and S.M. Strate (1993). Exertion cramps: a prospective study of biochemical and anthropometric variables in bicycle riders. Cycling Sci. 5: 15-20.