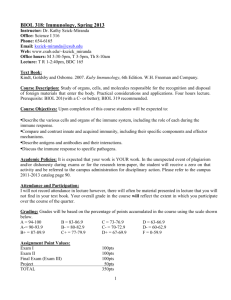
Lecture notes
advertisement

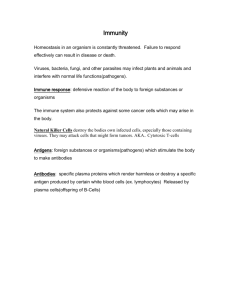
Introduction to Immunology The challenge of infection and the constitution of the immune system Infections are a major cause of morbidity and mortality worldwide. The body fights infection through the functions of its immune system, whose power has been harnessed by the development of vaccination (immunisation). A major success of vaccination has been the worldwide eradication of smallpox. There are many types of infective agents. Within the main categories of viruses, bacteria, fungi, protozoa and parasitic worms there are many different species each of which poses a different threat to the body. Furthermore, the differences in nature, mode of entry into the body, and mechanisms of replication and spread in the body of different infective agents mean that a range of defensive mechanisms is necessary. Thus, a variety of cellular and molecular components constitute the immune system. The cellular constituents of the immune system include the white blood cells (leucocytes), as well as cells in specialised tissues and cells scattered throughout most tissues of the body. They can be categorised according to their developmental origin from stem cells in the bone marrow (myeloid and lymphoid), or their morphology (the polymorphonuclear leucocytes known as granulocytes, and mononuclear cells). There are a large number of secreted molecular mediators of immunity. Some have anti-microbial activities, whereas others have regulatory or inflammatory effects. The constituents of the immune system are spread throughout the body. This is particularly illustrated by the lymphocytes. They are produced and develop in the primary lymphoid organs (bone marrow and thymus) and then recirculate around the body in the blood. They congregate in specialised lymphoid tissues that include the spleen, lymph nodes and mucosa-associated lymphoid tissues (MALT). Lymphocytes enter the spleen from the blood and then return directly to the blood stream. Most lymphocytes that enter lymph nodes do so directly from the blood, but some diffuse into other tissues and drain to lymph nodes via the afferent lymphatics. Lymphocytes return to the blood stream from lymph nodes via the efferent lymphatics, with most entering the blood at the thoracic duct. The nature of immunity The major functions of the immune system are the recognition of infective agents by interacting with microbes and their components, and defence of the body by the elimination of microbes and their components. Immune recognition and defence are achieved in two ways: by components of the immune system that generate innate immunity, and others that generate adaptive immunity. The main features of innate immunity are that it is quickly activated when infection occurs; it remains the same on repeated exposure to the same microbe and is moderately efficient. Innate immunity provides a general response to categories of microbes (eg. viruses or bacteria), and is triggered by the recognition of chemical structures that are characteristic of microbes – these are often termed pathogen-associated molecular patterns (PAMPs), eg. bacterial lipopolysaccharide and viral double-stranded RNA. These PAMPs interact with pattern recognition receptors expressed on cell surfaces (eg. toll-like receptors). The main features of adaptive (also known as acquired) immunity are that it is more slowly activated than innate immunity, but its efficacy improves upon repeated exposure to the same microbe. Once activated, adaptive immunity is highly efficient and provides specific responses tailored to each individual type of microbe. This is because adaptive immunity involves recognition of antigens specific to each type of microbe that are recognised by antigenreceptors that are clonally expressed by lymphocytes. Thus, lymphocytes are the cell type responsible for the properties of adaptive immunity. The first infection by a particular microbe generates a primary immune response. This normally requires microbes to penetrate surface epithelial barriers of the body, eg. the epidermis of the skin. An immediate local innate response in the infected tissues is generated by components of the immune system resident in those tissues (eg. macrophages and complement proteins). This also generates inflammatory mediators (augmented by the activation of mast cells) that attract further leucocytes and serum proteins into the infected tissues from the blood stream. While the above innate response is being generated, antigens are carried from the site of infection to nearby lymphoid tissues (eg. lymph nodes) in order to generate an adaptive immune response. Some antigens are carried free in the lymph, and some are captured by specialised cells, present in most tissues of the body, called dendritic cells: these migrate to the lymphoid tissues carrying the antigens with them. In the lymphoid tissues the antigens activate lymphocytes that specifically recognise them (which will be only a few of all the lymphocytes in these tissues). The specifically activated lymphocytes and antibodies (produced by the B lymphocytes) can then recirculate back to the site of infection. If re-infection with the same type of microbe occurs soon after the response above, then pre-formed antibodies and effector lymphocytes will be available immediately. A later re-infection will generate a secondary immune response by memory lymphocytes formed during the primary response: these give a faster and bigger response than occurred in the primary response, hence the term adaptive immunity. Different types of defensive strategy are required to deal with microbes that occupy different tissue compartments when they infect the body. Microbes that remain outside cells (extra-cellular) are available for being coated (opsonised) by antibodies and complement proteins, and can be engulfed and digested by phagocytes. Some microbes that have been phagocytosed by macrophages are resistant to digestion and can survive and replicate in intracellular vesicles, in which case the macrophages require activation signals from helper T lymphocytes to increase their digestive capacity. Other microbes deliberately infect cells: this applies to all viruses that use the metabolic machinery of the cells they infect to bring about their replication. Interferon proteins can block the replication of viruses in infected cells, and killer cells (natural killer cells and cytotoxic T cells) kill infected cells thereby preventing replication of the intra-cellular microbes. Immunopathology Refers to those diseases in which the immune system is involved in the pathophysiology. This may involve defects in, or inappropriate activity of, the immune system. Immunodeficiency disorders are those in which particular components of the immune system are missing or defective. Primary immunodeficiencies are genetic disorders, eg. severe combined immunodeficiency, in which lymphocytes are not produced. Secondary immunodeficiencies are acquired during life, eg. acquired immunodeficiency syndrome (AIDS) due to infection with human immunodeficiency virus (HIV) that infects and kills helper T lymphocytes. Allergies are due to inappropriate adaptive immunity against non-infective environmental materials (termed allergens) that leads to inflammatory tissue damage. Examples include allergic rhinitis (eg. hayfever caused by plant pollens), asthma (that may be caused by house dust mite proteins), and eczema. Anaphylaxis is a very dangerous systemic form of allergic response. All the above are examples of atopic allergies: a different type of allergic response is seen in contact dermatitis (eg. nickel allergy). Allergies affect up to 30% of the UK population. In autoimmune diseases, adaptive immunity is generated directly against certain of the body’s own components (referred to as autoantigens). Examples include autoimmune thyroiditis, rheumatoid arthritis and systemic lupus erythematosus (SLE). About 5% of the UK population are affected by autoimmune diseases. The rejection of transplanted tissue grafts is a man-made form of immunological tissue damage caused by antigenic differences in tissue components between donor and recipient that generate an adaptive anti-graft immune response by the recipient. Lymphoproliferative diseases occur when there is malignant transformation of cells of the immune system: they include lymphomas, leukaemias and myelomas. Recommended reading: Todd I, Spickett G (2005) Lecture Notes: Immunology. 5th edition. Blackwell Publishing. Chapter 1. OR Todd I, Spickett G (April 2010) Lecture Notes: Immunology. 6th edition. Wiley/Blackwell. Chapter 1.