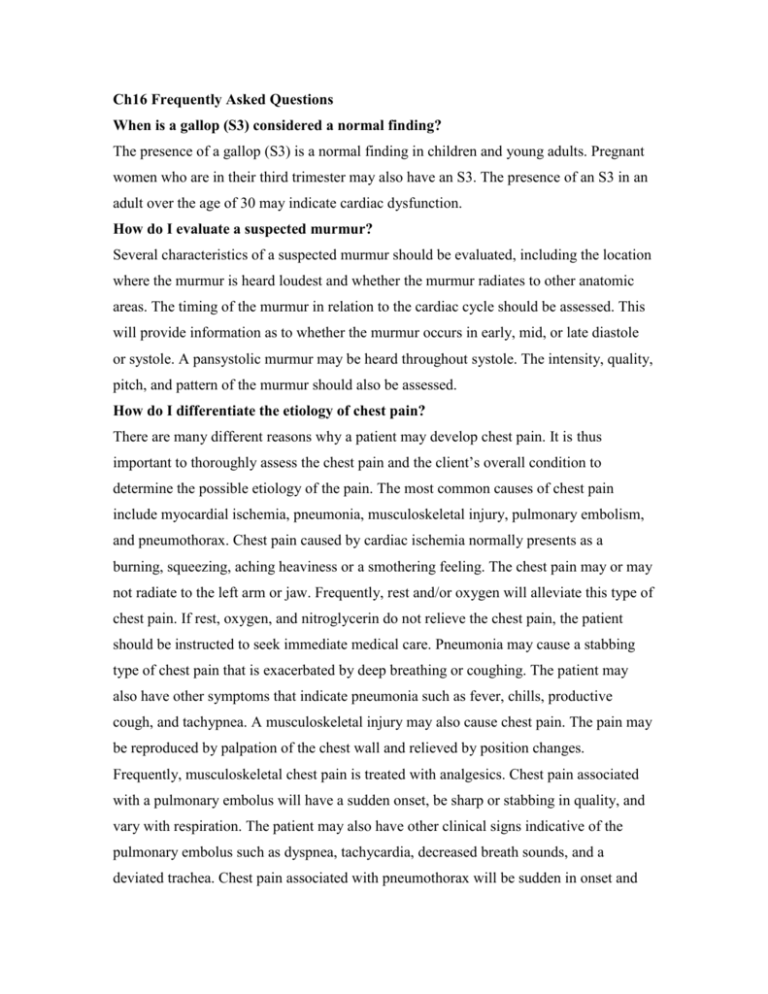
Ch16 Frequently Asked Questions
When is a gallop (S3) considered a normal finding?
The presence of a gallop (S3) is a normal finding in children and young adults. Pregnant
women who are in their third trimester may also have an S3. The presence of an S3 in an
adult over the age of 30 may indicate cardiac dysfunction.
How do I evaluate a suspected murmur?
Several characteristics of a suspected murmur should be evaluated, including the location
where the murmur is heard loudest and whether the murmur radiates to other anatomic
areas. The timing of the murmur in relation to the cardiac cycle should be assessed. This
will provide information as to whether the murmur occurs in early, mid, or late diastole
or systole. A pansystolic murmur may be heard throughout systole. The intensity, quality,
pitch, and pattern of the murmur should also be assessed.
How do I differentiate the etiology of chest pain?
There are many different reasons why a patient may develop chest pain. It is thus
important to thoroughly assess the chest pain and the client’s overall condition to
determine the possible etiology of the pain. The most common causes of chest pain
include myocardial ischemia, pneumonia, musculoskeletal injury, pulmonary embolism,
and pneumothorax. Chest pain caused by cardiac ischemia normally presents as a
burning, squeezing, aching heaviness or a smothering feeling. The chest pain may or may
not radiate to the left arm or jaw. Frequently, rest and/or oxygen will alleviate this type of
chest pain. If rest, oxygen, and nitroglycerin do not relieve the chest pain, the patient
should be instructed to seek immediate medical care. Pneumonia may cause a stabbing
type of chest pain that is exacerbated by deep breathing or coughing. The patient may
also have other symptoms that indicate pneumonia such as fever, chills, productive
cough, and tachypnea. A musculoskeletal injury may also cause chest pain. The pain may
be reproduced by palpation of the chest wall and relieved by position changes.
Frequently, musculoskeletal chest pain is treated with analgesics. Chest pain associated
with a pulmonary embolus will have a sudden onset, be sharp or stabbing in quality, and
vary with respiration. The patient may also have other clinical signs indicative of the
pulmonary embolus such as dyspnea, tachycardia, decreased breath sounds, and a
deviated trachea. Chest pain associated with pneumothorax will be sudden in onset and
described as a tearing or pleuritic chest pain. Breathing will worsen it. The patient may
also have other signs of pneumothorax such as dyspnea, tachycardia, decreased breath
sounds, and a deviated trachea.
Copyright © 2010 by Delmar/Cengage Learning. All rights reserved.