Common-Cardiac-Complaints-case-study-4-1
advertisement

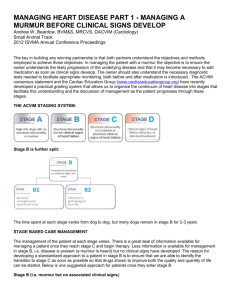
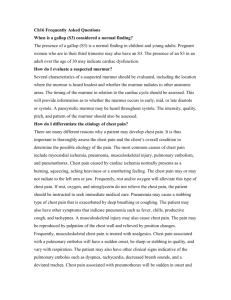
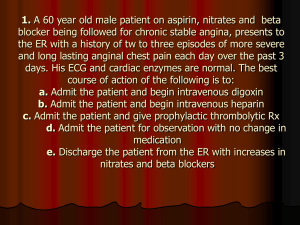
Common Cardiac Complaints Case study # 4 1. Chest Pain: Cardiac and Non-cardiac (20 Points) a) Ms. Davis is a 50 year old financial bank manager that presents with a complaint of mid- sternal chest pain. That is intermittently sharp, aggravated by stretching. She was perfectly fine until 1 week ago when she helped a neighbor move. What physical finding on your exam would most help you diagnose the origin of Ms. Davis chest pain? What is your likely diagnosis and treatment plan for Ms. Davis? Describe the common non-cardiac causes of chest pain, for each list diagnostic indicators, history, exam, and diagnostic testing to help confirm origin of chest pain. b) Mr. Matthews is a 65 year old retired school teacher, who has smoked 1 pack per day for 30 years who complains of chest pain lasting about 20 minutes, usually happens when he exerts himself and when he feels stressed. Associated factors include fatigue, dizziness, and diaphoresis. He denies chest pain at time of clinic visit. Review of systems is negative. His blood pressure is 150/90, HR88. Exam: Alert and oriented x3, Appears anxious Eyes: PERRLA, EOMI intact, fundoscopic exam normal Lungs: CTA Cardiac: RRR S1 S2 S4 no murmur. Abdomen: Rounded, + BS, Non tender, no organomegally. Extremities: no edema, Pedal Pulses 2+ bilaterally. What labs and diagnostic studies if any would you order? What is your most likely diagnosis? What would be your most appropriate plan for this patient explain your answer 2. Heart Murmurs (20 points) a) A 41-year-old retired played in the National Basketball Association presents for evaluation of perceived decrease in exertional tolerance. On examination, he is slender and of tall stature and has a low upper-to lower-extremity segment ration. He has mild scoliosis and a subtle pectus deformity. His lung fields are clear. On cardiac examination, blood pressure is 160/50 mm hg. Palpation of the apex shows its location to be in the sixth intercostal space in the anterior axillary line. The first heart sound is normal, and the second heart sound is physiologically split. There is a long blowing, grade 2-3/6 1 holodiastolic murmur head along the left sternal border, which also is easily audible at the apex, and a third heat sound also is present. In addition to the diastolic murmur, there is a soft 2/6 mid-peaking systolic ejection quality murmur. Based on your exam what is this patient likely to have? What descriptive criteria are used to describe heart sounds? If your patient cardiac exam had revealed a 3/6 crescendo-decrescendo systolic murmur with radiation to the neck, what would your patient likely have based on this finding? What is the difference between a physiologic murmur and a pathologic murmur? b) You examine an 18 year old man who is seeking a sports clearance physical examination. You note a midsystolic murmur that gets louder when he stands. What is your likely conclusion? Explain your answer What work up is necessary? Explain your answer. 3. Newborn/infant red flags (10 points) Describe specific findings seen in a newborn/infant/toddler that would increase your index of suspicion of a cardiac problem? 4. Pregnancy & aging cardiac normal variations (10 points) a) Describe specific normal cardiac changes seen in pregnancy and aging. 5. Heart Failure (20 Points) a) Mr Edwards presents to your clinic for his annual physical and refill of his medications. He has history of HTN and Dyslipidemia. His medications include HCTZ 25 mg daily and Simvastatin 40 mg. He does not smoke, and denies chest pain. On your exam you note that he appears short of breath. You inquire more and find he tells you he has increases SOB when he is lying down. List three additional examination findings that would cause you to suspect that Mr. Edwards has CHF? 1. 2. 3. What are the treatment priorities for a patient in CHF? 1. 2 2. 3. You do an EKG, knowing the history of Mr Edwards what finding on his EKG would you note as contributory to his CHF? You also do a chest x-ray. What findings on the chest x-ray would lead you to suspect CHF? b) You examine Mrs. Watson, an 80-year-old woman who has a history of CHF. She is in the office because of increasing shortness of breath. When auscultation her heart, you note a tachycardia with a rate of 104 beats per minute and an extra heart sound early in diastole. What does this sound most likely represent? (hintwhat murmur, gallop sound) You choose to add a beta blocker to her medications. Your rationale for using beta blocker therapy in treating a patient with CHF is to: (explain your answer). What labs would you order today if any? Explain your answer 3