CLINICAL EVALUATION OF GLOMERULAR FILTRATION
advertisement

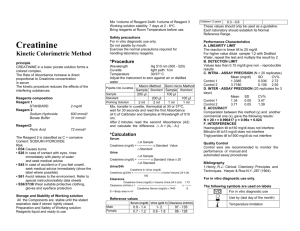
CLINICAL EVALUATION OF GLOMERULAR FILTRATION S.P. DiBartola, DVM D.J. Chew, DVM LEARNING OBECTIVES 1. Understand the meaning of the terms renal disease, renal failure, azotemia, and uremia. 2. Understand the concept of pre-renal, primary, and post-renal azotemia and be able to localize azotemia in a patient, given relevant clinical information. 3. Understand what the magnitude of azotemia can and cannot tell the clinician about the patient. 4. Understand the metabolism and excretion of urea and creatinine. 5. Understand the concept of clearance. 6. Understand the value and limitation of creatinine clearance determinations and the difference between exogenous and endogenous creatinine clearances. I. Clinical characteristics of the ideal substance to measure glomerular filtration rate (GFR) A. B. C. D. E. F. G. Freely filtered at the glomerulus Not bound to plasma proteins Not metabolized Non-toxic Excreted only by the kidneys Neither reabsorbed nor secreted by the renal tubules Stable in blood and urine and easily measured II. Definitions A. Renal disease implies the presence of histologic lesions in the kidney but does not specify any degree of renal dysfunction B. Renal failure implies that at least 75% of the total nephron population has become non-functional but does not necessarily imply underlying histologic lesions in the kidney. Renal failure occurs when the kidneys are no longer able to maintain the regulatory, excretory, and endocrine functions required of them resulting in retention of nitrogenous solutes and derangement of fluid, electrolyte, and acidbase balance. C. Azotemia refers to the increased concentration of non-protein nitrogenous waste products (e.g., urea, creatinine) in the blood. Azotemia may or may note be associated with clinical signs. 1. Pre-renal azotemia is that due to reduced renal perfusion (e.g., shock, dehydration, congestive heart failure) 2. Primary (intrinsic) renal azotemia is that due to renal parenchymal disease 3. Post-renal azotemia is that due to impaired elimination of urine from the body (e.g. urethral obstruction, ruptured bladder) D. Uremia refers to the constellation of clinical and biochemical abnormalities associated with a critical loss of functioning nephrons and includes the extra-renal manifestations of renal failure (e.g., uremic gastroenteritis, hyperparathyroidism) III. Blood urea nitrogen (BUN) A. The term blood urea nitrogen (BUN) is used most commonly but some authors prefer serum urea nitrogen (SUN) or plasma urea nitrogen (PUN), depending on the sample submitted. Urea nitrogen concentration is the same in blood, serum, or plasma. Urea nitrogen, however, is not the same as urea concentration. Only 47% of urea is nitrogen, and BUN = 0.47 × urea concentration. B. Normal BUN concentrations in domestic animals are: 1. 2. 3. 4. Dogs Cats Horses Cattle 8-25 mg/dL 15-35 mg/dL 10-27 mg/dL 5-23 mg/dL C. Metabolism of urea 1. Normally, very little urea is consumed in the diet. 2. Urea is an endproduct of protein and amino acid catabolism and is synthesized in the liver using ammonia (NH3) derived from amino acids. In the urea cycle, two NH3 molecules are combined with one molecule of CO2 to form urea.* Proteins contributing to urea synthesis may either be endogenous (i.e., body proteins) or exogenous (i.e., dietary proteins). 3. Urea is freely permeable across cell membranes and is distributed throughout total body water (i.e., intracellular and extracellular water). *The actual summary equation is: NH4+ + CO2 + 3 ATP4- + 2 H2O + aspartate- urea + 2 ADP3- + 2 Pi2- + AMP2- + PPi3- + fumarate- + 5 H+. Where Pi refers to phosphate and PPi to pyrophosphate and the second molecule of NH3 comes from aspartate. D. Excretion of urea 1. Quantitatively, excretion by the kidneys is the most important route of urea excretion. a. Urea is filtered at the glomeruli. b. It is passively reabsorbed from renal tubular fluid, depending upon renal tubular flow rate. i. Less urea is passively reabsorbed with more rapid tubular flow rates. ii. More urea is passively reabsorbed with slower tubular flow rates. iii. Even at maximal renal tubular flow rates, up to 40% of filtered urea is reabsorbed. c. Urea is not secreted by the renal tubular cells. 2. Production of urea and excretion into urine do not proceed at a constant rate but vary with protein intake. High protein meals increase GFR and urea excretion. 3. As much as 25% of synthesized urea may be degraded by enteric bacteria. 4. Urea excretion requires no metabolic work by the kidneys. The work of glomerular filtration is provided by cardiac contraction. 5. The prevailing BUN concentration reflects renal excretion of urea and the rate of protein catabolism in the body. E. Measurement of urea 1. The urease method is most specific and accurate. 2. Most commercial laboratories use a diacetylmonoxamine method that is less specific but provides results comparable to the urease method when the BUN concentration is < 100 mg/dL. The diacetylmonoxamine method may overestimate the urea nitrogen concentration when the BUN exceeds 100 mg/dL. 3. Dipstrip test pads (e.g., Azostix) utilize urea methodlogy but are not very accurate. 4. Laboratory measurement of BUN is technically easy and reproducible. F. Increased BUN 1. Non-renal factors a. High protein meal i. BUN concentrations of 30-40 mg/dL may be observed 4-8 hrs after feeding. ii. Food (not water!) should be withheld for 12 hours before sampling to avoid confusion. b. Hemorrhage into the gastrointestinal tract c. Increased catabolism (e.g., fever, burns, infection) d. Drugs (e.g., glucocorticoids, azathioprine, tetracyclines) 2. Renal factors a. Pre-renal b. Primary (intrinsic) renal c. Post-renal G. Decreased BUN 1. Non-renal factors a. Low protein diet b. Severe liver disease or portosystemic shunting of blood c. Anabolic steroids IV. Creatinine A. Normal serum creatinine concentrations in domestic animals are: 1. 2. 3. 4. Dogs Cats Horses Cattle 0.3-1.2 mg/dL 0.8-1.8 mg/dL 1.0-1.8 mg/dL 0.6-1.5 mg/dL B. Metabolism of creatinine 1. Creatinine is a spontaneous, non-enzymatic breakdown product of phosphocreatine in muscle. 2. Creatinine is released into the blood from muscle at a relatively constant rate for a given individual. 3. The daily rate of production of creatinine is determined largely by the age, sex, and muscle mass of the individual. a. Young animals have lower serum creatinine concentrations than mature ones. b. Males have slightly higher serum creatinine concentrations than females. c. Well-muscled individuals have slightly higher serum creatinine concentrations than thinner ones. 4. Serum creatinine concentration is not altered appreciably by diet. 5. Creatinine is not metabolized in the body. C. Excretion of creatinine 1. Creatinine is excreted by the kidneys almost entirely by glomerular filtration. 2. Its rate of excretion is relatively constant in the steady state and its serum concentration varies inversely with GFR. Consequently, its clearance is a good estimate of GFR (see below). 3. For the most part, creatinine is neither reabsorbed nor secreted by the renal tubules. There is a weak secretory mechanism for creatinine in the renal tubules, but this does not seriously jeopardize the usefulness of creatinine as an indicator of GFR. 4. Enteric metabolism of creatinine is not thought to be quantitatively important. D. Measurement of creatinine 1. Creatinine usually is measured by the alkaline picrate reaction, which is not entirely specific for creatinine and measures another group of substances collectively known as non-creatinine chromagens. a. Non-creatinine chromagens may constitute up to 50% of the measured creatinine at normal serum creatinine concentrations. b. Non-creatinine chromagens do not appear in the urine. c. Special methods have been designed to circumvent the problem of noncreatinine chromagens but these methods are difficult and not routinely used by commercial laboratories. 2. As serum creatinine concentration increases as a result of the progression of renal disease and decline in GFR, the amount of non-creatinine chromagens is unchanged and contributes proportionately less to the total measured serum creatinine concentration. E. Increased creatinine concentration 1. Non-renal factors are of minimal importance a. Massive muscle necrosis b. Prolonged strenuous exercise 2. Renal factors a. Pre-renal b. Primary (intrinsic) renal c. Post-renal F. Decreased creatinine concentration (uncommon) 1. Severe loss of muscle mass 2. Small body size 3. Young age V. Interpretation of BUN and serum creatinine concentrations A. The relationship of BUN or serum creatinine to GFR is a rectangular hyperbola (see Figure 1) Figure 1: Steady state relationship between BUN or serum creatinine and percentage of functional nephrons or percentage of normal glomerular filtration rate (GFR). 1. The slope of the curve is small when GFR is mildly or moderately decreased (i.e., large changes in GFR early in the course of renal disease cause small increases in BUN or serum creatinine concentration that may be difficult to appreciate clinically) 2. The slope of the curve is large when GFR is severely reduced (i.e., small changes in GFR in advanced renal disease cause large changes in BUN or serum creatinine concentration) B. The inverse relationship between BUN and serum creatinine concentrations and GFR is only valid in the steady state. C. When non-renal variables have been eliminated from consideration, an increase in BUN or serum creatinine concentration above normal implies that at least 75% of the nephrons are not functioning. 1. Neither the cause nor the reversibility of this malfunction can be predicted from the magnitude of BUN or serum creatinine concentration. 2. The magnitude of the BUN or serum creatinine concentration cannot be used to predict whether the azotemia is pre-renal, primary renal, or post-renal in origin. a. Pre-renal azotemia tends to be mild b. Post-renal azotemia tends to be severe c. There is so much overlap that localization of azotemia based on magnitude is not possible in individual patients 3. The magnitude of the BUN or serum creatinine concentration cannot be used to differentiate acute versus chronic, reversible versus irreversible, or progressive versus non-progressive disease processes. D. The BUN/creatinine ratio in pre-renal and post-renal azotemia may be increased because of increased tubular reabsorption of urea at lower tubular flow rates in dehydration or greater absorption of urea (as compared with creeatinine) across peritoneal membranes in animals with uroabodmen. E. A decrease in the BUN/creatinine ratio often follows fluid therapy and usually reflects decreased tubular reabsorption of urea rather than increased GFR. F. Both BUN and serum creatinine concentration are relatively insensitive indicators of renal function and one is not more sensitive than the other. Serum creatinine concentration, however, is affected by fewer non-renal variables. G. Localization of azotemia requires consideration of the history and physical examination, the patient's urine specific gravity before any fluid therapy or drugs that may interfere with concentrating ability (e.g. glucocorticoids, diuretics), and the patient's response to fluid therapy. See notes on Clinical Evaluation of Tubular Function for details. Some examples: 1. A dog is presented for persistent vomiting and is estimated to be 10% dehydrated on physical examination. BUN is 70 mg/dL and USG is 1.054. After fluid therapy, BUN is 20 mg/dL. Conclusion: pre-renal azotemia. 2. A dog is presented for weight loss, lethargy, anorexia, and vomiting and is estimated to be 10% dehydrated on physical examination. BUN is 175 mg/dL and USG is 1.013. After fluid therapy, BUN is 75 mg/dL. Conclusion: prerenal and renal azotemia. 3. A dog is presented for lethargy and vomiting and is estimated to be 10% dehydrated on physical examination. BUN is 70 mg/dL and USG is 1.013. After fluid therapy, BUN is 20 mg/dL. Conclusion: pre-renal azotemia and underlying renal disease. VI. Concept of clearance A. The renal clearance of a substance is that volume of plasma that would have to be filtered by the glomeruli in one minute to account for the amount of that substance appearing in the urine each minute under steady state conditions. Put differently, it is that volume of plasma that contains the same amount of the substance that is excreted in the urine in one minute under steady state conditions. The general clearance formula (ml/min) is UxV/Px.Where, Ux = Urine concentration of x (mg/dL) Px = Plasma concentration of x (mg/dL) V = Urine output (mL/min) B. The renal clearance of a substance that is neither reabsorbed nor secreted by the tubules is equal to the GFR. For such a substance in a steady state, the amount filtered equals the amount excreted. Thus, GFR × Px = Ux × V Dividing both sides of the equation by Px gives the general clearance formula (UxV/Px) which in this case is equal to the GFR. C. If x is reabsorbed from the tubules, Cx will be less than GFR because Ux will be decreased and Px will be increased. D. If x is secreted into the tubules, Cx will be greater than GFR because Ux will be increased and Px will be decreased. E. Clearance values usually are expressed relative to body weight (ml/min/kg) or body surface area (ml/min/M2) F. Inulin is a polymer of fructose that meets all the criteria for the ideal substance to measure GFR (listed at the beginning of this set of notes) and inulin clearance is considered the "gold standard" for GFR determination. Inulin does not occur naturally in the body and it must be infused into the animal at a constant rate to determine its renal clearance. Consequently, inulin is not used clinically the estimate GFR. G. Creatinine is produced endogenously and excreted by the body by glomerular filtration without significant tubular reabsorption or secretion. Thus, its clearance can be used to estimate GFR in the steady state. Normal endogenous creatinine clearance in domestic animals is 2 to 5 ml/min/kg. Dogs normally have values at the higher end of this range, cats values in the middle, and horses and cattle values at the lower end of the range. H. The only requirements for determination of endogenous creatinine clearance are an accurately timed collection of urine (usually 24 hours), determination of the patient's body weight, and serum and urine creatinine concentrations. Failure to collect all urine produced will erroneously reduce the calculated clearance value. I. Endogenous creatinine clearance slightly underestimates GFR as measured by inulin clearance because determination of Px includes non-creatinine chromagens when the alkaline picrate technique is used to measure creatinine but Ux does not. In the dog, this error is somewhat offset by a weak secretory mechanism for creatinine in the renal tubules. J. To eliminate inaccuracy caused by non-creatinine chromagens, some investigators have advocated use of exogenous creatinine clearance. In this procedure, creatinine is administered subcutaneously or intravenously to increase serum creatinine concentration approximately 10-fold and reduce the relative effect of non-creatinine chromagens. Exogenous creatinine clearance exceeds endogenous creatinine clearance and closely approximates inulin clearance. K. In chronic progressive renal disease, urinary concentrating ability is impaired after 67% of the nephron population has become non-functional whereas azotemia does not develop until 75% of the nephrons have become non-functional (see notes on Chronic Renal Failure for more details). The main indication for determination of creatinine clearance is the clinical suspicion of renal disease in a patient with polyuria and polydipsia but normal BUN and serum creatinine concentrations. This test is not helpful in hydrated patients that are already azotemic. L. Variation in creatinine clearance determinations in normal animals can arise from many factors and attempts should be made to control as many of them as possible. 1. Different methods of urine collection 2. Fasted or fed condition (i.e. protein feeding can augment GFR for several hours) 3. State of hydration 4. Use of anesthesia VII. Sodium sulfanilate A. Sodium sulfanilate is excreted solely by glomerular filtration and measurement of its plasma half life has been used as an indicator of GFR. B. It is administered intravenously at a dosage of 20 mg/kg in the dog and 11 mg/kg in the cat and heparinized blood samples are collected at 30, 60, and 90 minutes. Normal values in dogs are 40-80 minutes. In cats, normal values are approximately 40-60 minutes and values of approximately 30-50 minutes have been obtained in horses. C. This test should not be performed if the animal has received sulfonamide medications as they may cross-react with sulfanilate. D. The advantage of this procedure is that urine samples are not required but its disadvantage is that a numerical value for GFR is not obtained. It is seldom performed in the clinical evaluation of renal function in domestic animals. VIII. Radioisotopes A. Radioisotopes have been used to determine GFR, effective renal plasma flow (ERPF), and filtration fraction (FF) in dogs and cats. B. The advantages of radioisotope procedures are that they do not require collection of urine and are not time consuming. The major disadvantages are the use of radioactive compounds and the need for special equipment and expertise. C. ERPF values for cats are lower than those observed in dogs and may represent actual species differences in renal blood flow. In one study, filtration fraction values were 0.39 in cats and 0.34 in dogs D. Nuclear imaging using 99mTc-diethylenetriaminepentaacetic acid (DTPA) has been used to determine GFR in dogs and cats. This method has the advantage of allowing GFR for individual kidneys to be determined. E. These techniques are beyond the scope of routine veterinary practice. Note: The subject urinary protein excretion in health and disease is covered in the notes on Urinalysis and those on Diseases of the Glomerulus. STUDY QUESTIONS 1. What are the criteria for the ideal substance used to measure glomerular filtration rate? 2. What is the difference between azotemia and uremia? 3. What is meant by "localization of azotemia?" What information is needed to "localize" a patient's azotemia? 4. Where does urea originate? 5. How is urea handled by the kidney? 6. What non-renal variables affect BUN? 7. Where does creatinine originate? 8. How is creatinine handled by the kidney? 9. What are non-creatinine chromagens and how do they affect the measurement of creatinine in the laboratory? 10. Compare and contrast BUN and serum creatinine as indicators of renal function. Is one better than the other? Is one affected by fewer non-renal variables than the other? 11. What is the relationship of BUN or serum creatinine concentration to glomerular filtration rate? If GFR acutely falls by 50% what will happen to serum creatinine or BUN concentration? 12. What percentage of the nephron population must be non-functional to cause an increase in BUN or serum creatinine concentration? 13. Of what value is the magnitude of BUN increase in localizing azotemia? In differentiating acute from chronic disease? In differentiating progressive from nonprogressive disease? 14. What causes the increase in BUN/creatinine ratio that occasionally is observed in prerenal azotemia? 15. What is meant by the renal clearance of a substance? 16. How will Cx compare to inulin clearance for a substance x that is partially reabsorbed by the renal tubules? For a substance x that is partially secreted by the renal tubules? 17. What is the difference between endogenous and exogenous creatinine clearance? 18. Is exogenous creatinine clearance better than endogenous creatinine clearance? Why or why not? 19. Sulfanilate gives information about which renal function? In what way is sulfanilate half life advantageous over creatinine clearance? REFERENCES 1. Finco DR, Duncan JR: Evaluation of blood urea nitrogen and serum creatinine concentrations as indicators of renal dysfunction: A study of 111 cases and a review of the literature. J Am Vet Med Assoc 168:593-601, 1976. Last edited: January 4, 2002.