HYPERLIPIDEMIA
advertisement

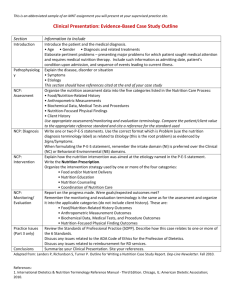
©2006 American Dietetic Association Disorders of Lipid Metabolism Toolkit Encounter Process for Disorders of Lipid Metabolism ENCOUNTER: Initial Encounter 45 to 90 minutes Nutrition Care Process and Documentation For more information on the Nutrition Care Process refer to ADA’s Nutrition Diagnosis: A Critical Step in the Nutrition Care Process, 2006 (http://www.eatright.org/cps/rde/xchg/ada/hs.xsl/career_912_ENU_HTML.htm) Assessment Obtain the following from client, medical record/information system or clinical referral form within 30 days of encounter. Client History consists of four areas: medication and supplement history, social history, medical/health history, and personal history. Medication and Supplement History includes, for instance, prescription lipid-lowering, antihypertensive, diabetes, and thyroid medications, over the counter (OTC) drugs, herbal and dietary supplements (for example folate, B-complex vitamins, Co-enzyme Q10, those with potential for food/drug interaction), and illegal drugs. Social History may include such items as smoking history, alcohol intake (frequency and amount), socioeconomic status, social and medical support, cultural and religious beliefs, housing situation, and social isolation/connection. Medical/Health History includes chief nutrition complaint, present/past illness particularly of cardiovascular disease, diabetes, thyroid disease, evaluate risk factors for cardiovascular disease, metabolic syndrome, family medical history, especially of premature cardiovascular disease, mental/emotional health and cognitive abilities. Personal History consists of factors including age, occupation, role in family, and education level. Biochemical Data includes laboratory data, for example, lipid profile, glucose, hemoglobin A1C, liver function tests, thyroid, Lp(a), homocysteine, and high-sensitivity C reactive protein. Anthropometric Measurements include height, weight, weight history, body mass index (BMI), waist circumference (WC), waist to hip ratio (WHR) Physical Exam Findings includes blood pressure, general physical appearance (abdominal girth and presence of xanthomas) muscle and subcutaneous fat wasting, and affect Food and Nutrition History consists of four areas: Food consumption, nutrition and health awareness and management, physical activity and exercise, and food availability Food Consumption may include factors such as detailed food and nutrient intake, calculation of specific nutrients (fat intake, percentage of calories from fat and type, sources of fat, total and soluble fiber intake, fish and soy products consumption, intake of folate and B vitamins, use of plant stanol/sterol esters), meal and snack patterns, environmental cues to eating, and current diets or food modifications, food allergies or food aversions, and frequency and choices of restaurant meals. Nutrition and Health Awareness and Management includes, for example, knowledge and beliefs about nutrition recommendations for lipid management, motivation and willingness to make necessary dietary and lifestyle changes to achieve expected lipid and non-lipid outcomes and goals, self-monitoring and management practices, and past nutrition counseling and education. ©2006 American Dietetic Association Disorders of Lipid Metabolism Toolkit Physical Activity and Exercise consists of activity patterns, amount of sedentary time (e.g. TV, phone, computer), and exercise intensity, frequency, and duration. Food Availability encompasses factors such as food planning, purchasing, preparation abilities and limitations, food safety practices, food and nutrition program utilization, and food insecurity. Documentation Needed: Medical record documentation Referrals from other health care professionals Diagnosis Whenever possible, a nutrition diagnosis statement is written in the PES format that states the problem (P), the etiology (E) and signs/symptoms (S). The Problem or Nutrition Diagnosis Label describes alterations in the patient/clients’ nutrition status that dietetics professionals are responsible for treating independently. Nutrition diagnosis differs from medical diagnosis in that a nutrition diagnosis changes as the patient/client response changes. The medical diagnosis does not change as long as the disease or condition exists. A nutrition diagnosis allows the dietetics professional to identify realistic and measurable outcomes, formulate interventions, and monitor and evaluate change. Example of Nutrition Diagnoses (Problems) related to Disorders of Lipid Metabolism √ √ NI-1.5 Excessive energy intake NI-2.2 Excessive oral food/bev. intake NI-4.3 Excessive alcohol intake NI-51.3 Inappropriate intake of food fatsspecify: NI-53.3 Inappropriate intake of types of carbohydrate—specify: NI-53.5 Inadequate fiber intake Other: NC-2.3 Food-medication interaction NC-3.3 Overweight/obesity NB-1.1 Food, nutrition and nutrition related knowledge deficit NB-1.3 Not ready for diet/lifestyle change NB-1.6 Limited adherence to nutritionrelated recommendations NB-2.1 Physical inactivity The Definition of Nutrition Diagnosis Label briefly describes the Nutrition Diagnosis Label to differentiate a discrete problem area (see Nutrition Diagnosis Manual for diagnosis list and more information). For example, the nutrition diagnosis of inappropriate intake of saturated fat is defined as the intake of wrong type or quality of food fats compared to established reference standards or recommendations based upon physiological needs. The Etiology (Cause/Contributing Risk Factors) are those factors contributing to the existence of, or maintenance of pathophysiological, psychosocial, situational, developmental, cultural, or environmental problems. It is linked to the diagnosis labeled by the words “related to” what is trying to be altered through medical nutrition therapy. For example, related to food and nutrition deficit. The Signs and Symptoms (Defining Characteristics) consist of subjective or objective data used to determine whether the patient/client has the nutrition diagnosis specified. These are the signs and symptoms gathered through nutrition assessment. It is linked to the etiology by the words “as evidenced by” what will be monitored and evaluated through follow-up. For example “as evidenced by LDL cholesterol >130 mg/dL.” ©2006 American Dietetic Association Disorders of Lipid Metabolism Toolkit Evaluating your PES statement: To evaluate whether your PES statement is appropriate ask the following questions: A. Can the RD resolve or improve the nutrition diagnosis? Can you envision an intervention that would address the etiology and thus resolve or improve the problem? If not, is your intervention targeted to reducing or eliminating the signs and symptoms? B. Does your nutrition assessment data support the Nutrition Diagnosis, etiology, and signs and symptoms? C. Is the etiology listed the “root cause?” Ask “Why” 5 times D. Will measuring the Signs and Symptoms tell you if the problem is resolved or improved? E. Are the Signs and Symptoms specific enough that you can measure and evaluate changes at the next visit to document resolution or improvement of the nutrition diagnosis? F. When all things are equal and you have a choice between stating the PES statement using two nutrition diagnosis labels in different domains, consider the intake nutrition diagnosis. Intervention Prioritize and select specific intervention strategies that are focused on the etiology of the problem. Interventions should be quantifiable, achievable and time defined. Communicate and carry out plan. Food and/or Nutrient Delivery (ND) refers to an individualized approach for food/nutrient provision. May relate to meals/snacks, enteral/parenteral nutrition, medical food supplements, vitamin/mineral supplement, bioactive substance supplement, feeding assistance, feeding environment and nutrition-related medication management. Meal Plan- provide a nutrition prescription based on the recommendations in the Disorders of Lipid Metabolism Evidence-Based Nutrition Practice Guidelines. Nutrition prescription should be individualized and based on client needs, consistent with client preferences and not contraindicated by risk or harm. Those dietary/lifestyle modifications not addressed in the initial encounter can be addressed as part of on-going follow-up encounters. Refer to Summary Page. Nutrition Education (E) is a formal process to instruct or train a patient/client in a skill or to impart knowledge to help patients/clients voluntarily manage or modify food choices and eating behavior to maintain or improve health. May include initial/brief education or comprehensive nutrition education. Discuss risk factors associated with heart disease and metabolic syndrome. Explain the effects of a cardioprotective diet, physical activity, and weight loss (if applicable) on lipid management. Physical Activity Plan–discuss benefits of physical activity, both aerobic and resistance activities, and impact on lipid, glucose, blood pressure, and weight management. Nutrition Counseling (C-1) is a supportive process, characterized by a collaborative counselorpatient/client relationship, to set priorities, establish goals, and create individualized action plans, which acknowledge and foster responsibility for self-care to treat an existing condition and promote health. May include theory or approaches, strategies and phases of counseling (e.g. behavioral modification, motivational interviewing, self-monitoring, goal setting, social support, and resolving) ©2006 American Dietetic Association Disorders of Lipid Metabolism Toolkit Self-monitoring–discuss techniques useful in recording food and beverage intake, behavior, and physical activity patterns. Individualized behavioral goals to address nutrition diagnosis–specific strategies related to the communication in Self Management Training, which are individualized to the setting and client. These can include reducing the amount of fat and changing sources of fat used in cooking, increasing fish intake, limiting foods with trans fatty acids, incorporating plant stanol/sterol esters, isocalorically substituting nuts into cardioprotective dietary pattern, increasing daily amount of steps taken, selecting leaner sources of animal protein when dining out, and avoiding sauces and gravies. Coordination of Nutrition Care (RC) is consultation with, referral to, or coordination of nutrition care with other health care providers, institutions, or agencies that can assist in treating or managing nutrition-related problems. Recommendations–to provider or others on health care team to reinforce nutrition and physical activity goals, recheck laboratory data, re-evaluate dosage and necessity of lipidlowering medications. Document at top of progress note. Referral(s)–includes, for example, endocrine evaluation, smoking cessation program, cardiac rehabilitation, and weight loss program Documentation–document initial progress note in client’s medical record/information system, according to organization’s policy. Contact information–instruct client to call or e-mail with questions and concerns Referral Source–send copy of initial progress note to physician and place original in client’s medical record. Confirm Appointment–put system in place to confirm client appointments to enhance show rates. Expected Outcomes: determine and review with client the expected outcome, amount of change (if applicable) and timeline for each of the following areas. Expected outcomes should be written in observable and measurable terms that are clear and concise. Expected outcomes should be client-centered and need to be tailored to what is reasonable to the client’s circumstances and appropriate expectations for treatments and outcomes. Biochemical–includes decreases in total cholesterol, LDL, Non-HDL (if Trig >200 mg/dL), fasting glucose within normal limits (WNL) or decrease, HDL increase. Anthropometric–includes maintains or achieves reasonable body weight, BMI, WC, WHR Physical and Food/Nutrition–includes BP WNL or decrease, decreases in saturated and trans fat, and cholesterol, increases in soluble fiber, incorporation of plant stanol/sterol esters, includes intake of fish, soy, nuts on weekly basis, calories and physical activity to maintain/reduce weight. Materials provided –client education resources pertaining to the treatment of Disorders of Lipid Metabolism √ √ Hypercholesterolemia Nutrition Therapy * Omega-3 Fat Tips Hypertriglyceridemia Nutrition Therapy * Soluble Fiber Tips Label Reading, Shopping Tips, Cooking Tips Plant Sterols and Stanols Tips * Trans Fat Tips Nuts Tips Other: Alcohol Tips * from ADA Nutrition Care Manual; ** from ADA Disorders of Lipid Metabolism EAL Toolkit ©2006 American Dietetic Association Disorders of Lipid Metabolism Toolkit Monitoring and Evaluation Follow-up on Expected Outcomes: specify next appointment and goal. For example, recommend appointment in 4 to 6 weeks to evaluate dietary intake according to behavioral goals. Future Plans for care: nutrition care, monitoring and follow-up or discharge, specify follow-up appointment schedule (per Evidence-Based Guidelines). Follow-up with client every 4 to 6 weeks depending on patient’s cardiovascular risk category, amount of dietary modifications needed to reach target goals, and level of motivation. ©2006 American Dietetic Association Disorders of Lipid Metabolism Toolkit ENCOUNTER: Follow-up Encounter(s) 30 to 60 minutes. Number and duration of encounters will depend on patient’s risk category, number of Therapeutic Lifestyle Changes that need to be made, and the motivational level of the patient. Nutrition Care Process and Documentation Assessment Obtain the following from client, medical record/information system or clinical referral form within 30 days of encounter. Review changes in biochemical data, anthroprometric measurements, and physical exam findings if applicable. Client History Review possible changes in medication and supplement history, social history, medical/health history, and personal history. Medication and supplement history may include prescription lipid-lowering, antihypertensive, diabetes, and thyroid medications, over the counter (OTC) drugs, herbal and dietary supplements for example folate, B-complex vitamins, Co-enzyme Q10, those with potential for food/drug interaction, and illegal drugs. Social history may include such items as smoking history, alcohol intake (frequency and amount), socioeconomic status, social and medical support, cultural and religious beliefs, housing situation, and social isolation/connection. Medical/health history includes comorbidities (hypertension, diabetes, obesity) and need for additional dietary modifications and combinations of evidence-based practice guidelines. Personal history consists of factors including age, occupation, role in family, and education level. Biochemical Data document and review changes in laboratory data, for example, lipid profile, glucose, hemoglobin A1C, liver function tests, thyroid, Lp(a), homocysteine, and high-sensitivity C reactive protein. Anthropometric Measurements document and review changes in height, weight, weight history, body mass index (BMI), waist circumference (WC), waist to hip ratio (WHR). Physical exam findings document and review changes in blood pressure, general physical appearance (abdominal girth and presence of xanthomas) muscle and subcutaneous fat wasting, and affect. Food and Nutrition History consists of four areas: Food consumption, nutrition and health awareness and management, physical activity and exercise, and food availability Food consumption: Review food and nutrient intake, include calculation of specific nutrients (fat intake, percent of calories from fat and type, sources of fat, total and soluble fiber intake, fish and soy products consumption, intake of folate and B vitamins, use of plant stanol/sterol esters) meal and snack patterns, environmental cues to eating, and current diets and food modifications, food allergies or food aversions, frequency and choices of restaurant meals. Self-monitoring records: Review records with client and evaluate client’s comprehension, receptivity and compliance of nutrition prescription. Provide feedback to client. Physical activity and exercise: Determine and review with client activity patterns, amount of sedentary time (e.g. TV. Phone, computer), and exercise intensity, frequency, and duration. ©2006 American Dietetic Association Disorders of Lipid Metabolism Toolkit Adherence/Barriers to Behavioral Goals: determine client’s understanding and compliance with prescribed plan, provide evidence that the plan is or is not changing behavior status, gather information indicating reasons for lack of progress and support conclusions. For example, client verbalizes need to increase physical activity level to improve glucose and lipid goals, however, client reports lack of time due to caring for a sick parent. Progress/Barriers towards Biochemical, Anthropometric, Physical and Food/Nutrition Goals: identify any positive or negative outcomes, gather information indicating reasons for lack of progress and support conclusions. For example, LDL cholesterol has decreased but is still not at target goal; or patient still consuming red meat four times a week. Documentation needed: Medical record documentation Referrals from other health care professionals Diagnosis Based on patient outcome data list and prioritize new and/or existing diagnosis(es). Write nutrition diagnosis statement in the PES format that states the problem (P), the etiology (E) and signs/symptoms (S). The Problem or Nutrition Diagnosis Label briefly describes the Nutrition Diagnosis Label to differentiate a discrete problem area (see description of initial encounter Nutrition Diagnosis Manual for diagnosis list and more information) The Etiology (Cause/Contributing Risk Factors) are those factors contributing to the existence of, or maintenance of pathophysiological, psychosocial, situational, developmental, cultural, and environmental problems. It is linked to the diagnosis labeled by the words “related to.” The Signs and Symptoms (Defining Characteristics) consist of subjective and objective data used to determine whether the patient/client has the nutrition diagnosis specified. These are the signs and symptoms gathered through nutrition assessment. It is linked to the etiology by the words “as evidenced by.” Intervention Select specific intervention strategies that are focused on the etiology of the problem. Modify plan as needed based on outcomes data collection. Communicate and carry out plan. Food and/or Nutrient Delivery (ND) (refer to description of initial encounter) Nutrition Education (E) (refer to description of initial encounter) Nutrition Counseling (C-1) (refer to description of initial encounter) Individualized Behavioral Goals to Address Nutrition Diagnosis–Revise as changes in condition/response occurs, using collected data on Adherence/Barriers to Behavioral Goals. For example, client’s BMI remains elevated, however her food choices are healthier. Determine and review portion control with client. Coordination of Nutrition Care (RC) (refer to description of initial encounter) includes documentation of follow-up encounter, communicate documentation of encounter to referral source, provide client with contact information for questions and concerns and set up a system for appointment confirmation. Document recommendations at top of progress note. Expected Outcomes–determine and review with client the expected outcome, amount of change (if applicable) and timeline for each of the following areas. Revise using collected data on Progress/Barriers towards Biochemical, Anthropometric, Physical, and Food/Nutrition Goals. (Refer to initial encounter) Materials provided–client education resources (refer to description of initial encounter) ©2006 American Dietetic Association Disorders of Lipid Metabolism Toolkit Monitoring and Evaluation Follow-up on Expected Outcomes–specify next appointment and goal. For example, meets goal set with registered dietitian to reduce amount of saturated and trans fat. Schedule check of lipid profile in 6 weeks. Future Plans for care–nutrition care, monitoring and follow-up or discharge, specify follow-up appointment schedule (per Evidence-Based Guidelines). For example, recommend appointment in 6 weeks to evaluate change in lipid profile in response to nutrition therapy. Review client education materials containing information on food labeling at next visit.